Ann Surg Treat Res.
2019 Jan;96(1):41-46. 10.4174/astr.2019.96.1.41.
Prospective study on the safety and feasibility of early ileostomy closure 2 weeks after lower anterior resection for rectal cancer
- Affiliations
-
- 1Department of Surgery, Chungnam National University Hospital, Daejeon, Korea. jkim@cnu.ac.kr
- 2Department of Surgery, Kangbuk Samsung Hospital, Seoul, Korea.
- KMID: 2429753
- DOI: http://doi.org/10.4174/astr.2019.96.1.41
Abstract
- PURPOSE
Transient loop ileostomies in rectal cancer surgery are generally closed after 2 or more months to allow adequate time for anastomotic healing. Maintaining the ileostomy may cause medical, surgical, or psychological complications; it also reduces the quality of life, and increase treatment costs. We performed this study to evaluate the safety and feasibility of early ileostomy closure 2 weeks postoperatively.
METHODS
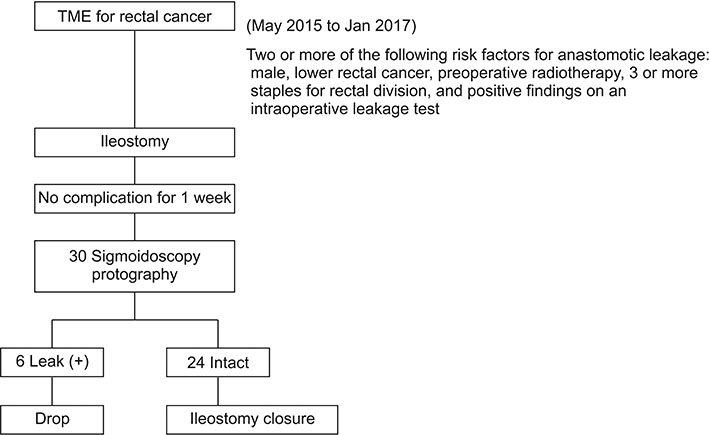
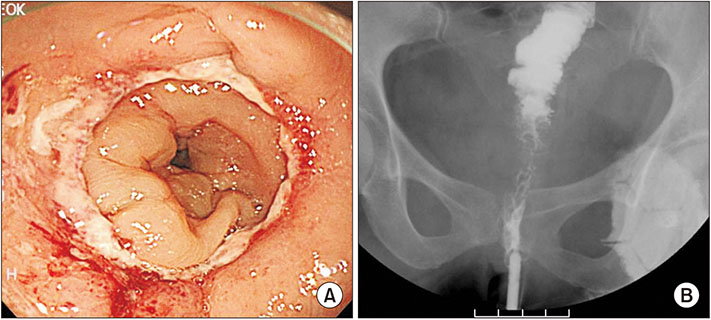
If a patient who underwent total mesorectal excision had 2 or more risk factors for anastomotic leakage, a loop ileostomy was created. After confirmation of intact anastomosis via sigmoidoscopy and proctography 1 week postoperatively, the patient was enrolled and ileostomy was closed 2 weeks postoperatively. The primary endpoint was the frequency of complication after ileostomy repair.
RESULTS
Thirty patients were enrolled in the study and 6 were excluded due to anastomotic leakage. Except for 1 case of wound infection (4.2%), no patient experienced any complication including newly developed leakage after the ileostomy closure. The mean duration to repair was 13.1 days (range, 8-16 days) and mean duration to the start of adjuvant treatment after radical surgery was 5.37 weeks (range, 3.0-8.1 weeks).
CONCLUSION
Transient loop ileostomy, which is confirmed to be intact endoscopically and radiologically, can be safely closed 2 weeks postoperatively without requiring a significant delay in adjuvant chemotherapy.
Keyword
MeSH Terms
Figure
Reference
-
1. Mealy K, Burke P, Hyland J. Anterior resection without a defunctioning colostomy: questions of safety. Br J Surg. 1992; 79:305–307.
Article2. Machado M, Hallbook O, Goldman S, Nystrom PO, Jarhult J, Sjodahl R. Defunctioning stoma in low anterior resection with colonic pouch for rectal cancer: a comparison between two hospitals with a different policy. Dis Colon Rectum. 2002; 45:940–945.3. Matthiessen P, Hallbook O, Rutegard J, Simert G, Sjodahl R. Defunctioning stoma reduces symptomatic anastomotic leakage after low anterior resection of the rectum for cancer: a randomized multicenter trial. Ann Surg. 2007; 246:207–214.
Article4. Huser N, Michalski CW, Erkan M, Schuster T, Rosenberg R, Kleeff J, et al. Systematic review and meta-analysis of the role of defunctioning stoma in low rectal cancer surgery. Ann Surg. 2008; 248:52–60.5. Perez RO, Habr-Gama A, Seid VE, Proscurshim I, Sousa AH Jr, Kiss DR, et al. Loop ileostomy morbidity: timing of closure matters. Dis Colon Rectum. 2006; 49:1539–1545.
Article6. O'Leary DP, Fide CJ, Foy C, Lucarotti ME. Quality of life after low anterior resection with total mesorectal excision and temporary loop ileostomy for rectal carcinoma. Br J Surg. 2001; 88:1216–1220.7. Tsunoda A, Tsunoda Y, Narita K, Watanabe M, Nakao K, Kusano M. Quality of life after low anterior resection and temporary loop ileostomy. Dis Colon Rectum. 2008; 51:218–222.
Article8. Menegaux F, Jordi-Galais P, Turrin N, Chigot JP. Closure of small bowel stomas on postoperative day 10. Eur J Surg. 2002; 168:713–715.
Article9. Bakx R, Busch OR, van Geldere D, Bemelman WA, Slors JF, van Lanschot JJ. Feasibility of early closure of loop ileostomies: a pilot study. Dis Colon Rectum. 2003; 46:1680–1684.10. Hindenburg T, Rosenberg J. Closing a temporary ileostomy within two weeks. Dan Med Bull. 2010; 57:A4157.11. Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009; 250:187–196.12. Martens MF, Hendriks T. Postoperative changes in collagen synthesis in intestinal anastomoses of the rat: differences between small and large bowel. Gut. 1991; 32:1482–1487.
Article13. Alves A, Panis Y, Lelong B, Dousset B, Benoist S, Vicaut E. Randomized clinical trial of early versus delayed temporary stoma closure after proctectomy. Br J Surg. 2008; 95:693–698.
Article14. Danielsen AK, Park J, Jansen JE, Bock D, Skullman S, Wedin A, et al. Early closure of a temporary ileostomy in patients with rectal cancer: a multicenter randomized controlled trial. Ann Surg. 2017; 265:284–290.15. Goussous N, Kemp KM, Bannon MP, Kendrick ML, Srvantstyan B, Khasawneh MA, et al. Early postoperative small bowel obstruction: open vs laparoscopic. Am J Surg. 2015; 209:385–390.
Article16. Wong KS, Remzi FH, Gorgun E, Arrigain S, Church JM, Preen M, et al. Loop ileostomy closure after restorative proctocolectomy: outcome in 1,504 patients. Dis Colon Rectum. 2005; 48:243–250.
Article17. Chow A, Tilney HS, Paraskeva P, Jeyarajah S, Zacharakis E, Purkayastha S. The morbidity surrounding reversal of defunctioning ileostomies: a systematic review of 48 studies including 6,107 cases. Int J Colorectal Dis. 2009; 24:711–723.
Article18. Hensler T, Hecker H, Heeg K, Heidecke CD, Bartels H, Barthlen W, et al. Distinct mechanisms of immunosuppression as a consequence of major surgery. Infect Immun. 1997; 65:2283–2291.
Article19. Sun Z, Adam MA, Kim J, Nussbaum DP, Benrashid E, Mantyh CR, et al. Determining the optimal timing for initiation of adjuvant chemotherapy after resection for stage II and III colon cancer. Dis Colon Rectum. 2016; 59:87–93.
Article20. Biagi JJ, Raphael MJ, Mackillop WJ, Kong W, King WD, Booth CM. Association between time to initiation of adjuvant chemotherapy and survival in colorectal cancer: a systematic review and meta-analysis. JAMA. 2011; 305:2335–2342.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Anastomotic Sinus That Developed From Leakage After a Rectal Cancer Resection: Should We Wait for Closure of the Stoma Until the Complete Resolution of the Sinus?
- Risk factors of stoma re-creation after closure of diverting ileostomy in patients with rectal cancer who underwent low anterior resection or intersphincteric resection with loop ileostomy
- Clinical Outcomes of Ileostomy Closure According to Timing During Adjuvant Chemotherapy After Rectal Cancer Surgery
- Routine barium enema prior to closure of defunctioning ileostomy is not necessary
- Double Stapling Technique in Low Anterior Resection for Rectal Cancer