J Korean Orthop Assoc.
2018 Jun;53(3):248-255. 10.4055/jkoa.2018.53.3.248.
The Efficacy of Different Ropivacaine Concentrations (0.5%, 0.6%, vs . 0.75%) for Regional Nerve Block in Lower Extremity: A Prospective Randomized Controlled Trial
- Affiliations
-
- 1Department of Orthopedic Surgery, Chungnam National University School of Medicine, Daejeon, Korea. faschan@hanmail.net
- KMID: 2429173
- DOI: http://doi.org/10.4055/jkoa.2018.53.3.248
Abstract
- PURPOSE
There have only been a few studies on optimal usage of injection material in the regional nerve block for lower extremity operations. The purpose of this study was to evaluate the efficacy of different concentrations of ropivacaine.
MATERIALS AND METHODS
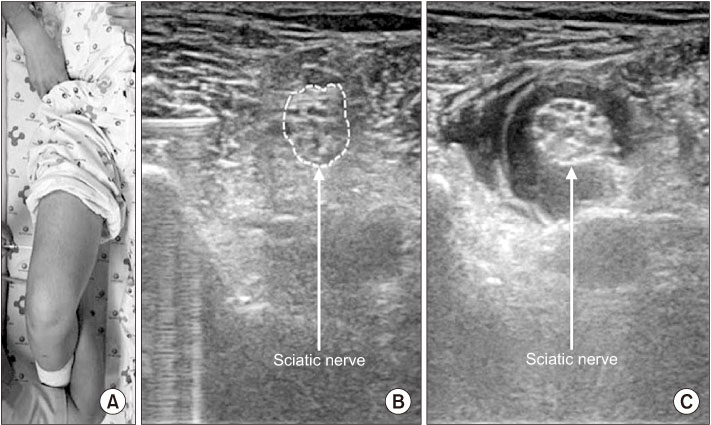
A total of 339 patients underwent lower extremity surgery under ultrasound-guided nerve block (combined femoral and sciatic nerve block) at a Chungnam National University Hospital between March 2016 and February 2017 and were randomly assigned to three groups: Group A (0.5%, 44 ml), group B (0.6%, 30 ml), and group C (0.75%, 30 ml). The interval between nerve block procedure and onset of the complete anesthetic effect (complete anesthetic time) was investigated. The degrees of intraoperative pain, and postoperative pain were evaluated using a visual analogue scale (VAS) score. Patient's satisfaction (0-10) was investigated. To evaluate the efficacy in accordance with the concentration under the same dose and same volume, group A and B were compared with group C respectively.
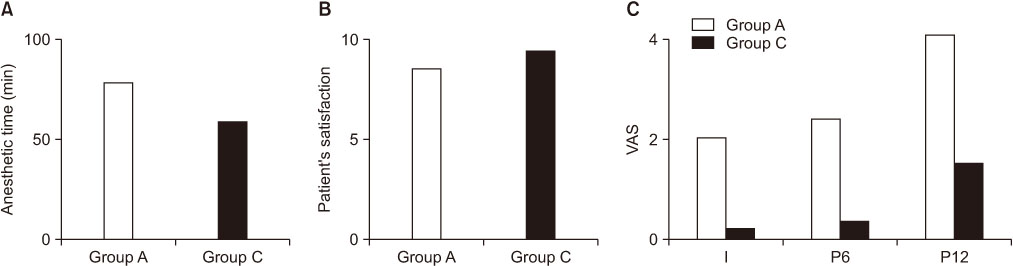
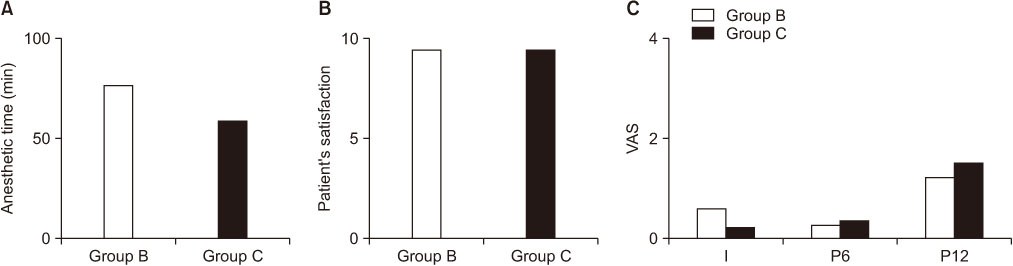
RESULTS
There were 108, 118, and 113, in groups A, B, and C, respectively; and there were no significant differences with respect to the number, age, sex, and type of operation (p>0.05). The mean complete anesthetic times were 78.5, 76.4, and 58.6 minutes, respectively. The mean intraoperative VAS scores were 2.04, 0.62, and 0.24; and the mean postoperative VAS scores (6 hours/12 hours) were 2.41/4.08, 0.27/1.24, and 0.38/1.54. The mean patient's satisfactory scores were 8.53, 9.38, and 9.40, respectively. Compared with group C, group A showed significantly longer complete anesthetic time (p < 0.05) and higher intra, postoperative VAS scores (all p < 0.05). Group B showed longer complete anesthetic time (p < 0.05), but no significant difference of intra, postoperative VAS scores (all p>0.05). Patient's satisfactory scores in both group A and B were similar to group C (p>0.05, p>0.05). There were no specific adverse reactions in all groups.
CONCLUSION
Ropivacaine 0.6% as well as 0.75% are safe and effective anesthetics under the same volume (30 ml) for regional nerve block of the lower extremity. However, taking into account of the longer complete anesthetic time, the operation start time must be adjusted.
Keyword
MeSH Terms
Figure
Reference
-
1. Kang C, Hwang DS, Kim YM, et al. Ultrasound-guided femorosciatic nerve block by orthopaedist for ankle fracture operation. J Korean Foot Ankle Soc. 2010; 14:90–96.2. Kang C. Ultrasound-guided regional nerve block in lower extremity. J Korean Orthop US Soc. 2012; 1:50–59.3. Mohan V. TKR under combined femoral and sciatic nerve blocks. Kerala J Orthop. 2015; 27:104–106.4. Klein SM, Greengrass RA, Steele SM, et al. A comparison of 0.5% bupivacaine, 0.5% ropivacaine, and 0.75% ropivacaine for interscalene brachial plexus block. Anesth Analg. 1998; 87:1316–1319.
Article5. McClure JH. Ropivacaine. Br J Anaesth. 1996; 76:300–307.
Article6. McClellan KJ, Faulds D. Ropivacaine: an update of its use in regional anaesthesia. Drugs. 2000; 60:1065–1093.7. Zhai W, Wang X, Rong Y, Li M, Wang H. Effects of a fixed low-dose ropivacaine with different volume and concentrations on interscalene brachial plexus block: a randomized controlled trial. BMC Anesthesiol. 2016; 16:80.
Article8. Su Y, Zhang Z, Zhang Y, Li H, Shi W. Efficacy of ropivacaine by the concentration of 0.25%, 0.5%, and 0.75% on surgical performance, postoperative analgesia, and patient's satisfaction in inguinal hernioplasty: a randomized controlled trial. Patient Prefer Adherence. 2015; 9:1375–1379.9. Fredrickson MJ, Abeysekera A, White R. Randomized study of the effect of local anesthetic volume and concentration on the duration of peripheral nerve blockade. Reg Anesth Pain Med. 2012; 37:495–501.
Article10. Marhofer P, Eichenberger U, Stöckli S, et al. Ultrasonographic guided axillary plexus blocks with low volumes of local anaesthetics: a crossover volunteer study. Anaesthesia. 2010; 65:266–271.
Article11. O'Donnell B, Riordan J, Ahmad I, Iohom G. Brief reports: a clinical evaluation of block characteristics using one milliliter 2% lidocaine in ultrasound-guided axillary brachial plexus block. Anesth Analg. 2010; 111:808–810.12. Wank W, Büttner J, Maier KR, Emanuelson BM, Selander D. Pharmacokinetics and efficacy of 40 ml ropivacaine 7.5 mg/ml (300 mg), for axillary brachial plexus block--an open pilot study. Eur J Drug Metab Pharmacokinet. 2002; 27:53–59.13. Baddoo H. A preliminary report on the use of peripheral nerve blocks for lower limb amputations. Ghana Med J. 2009; 43:24–28.14. Denny NM, Harrop-Griffiths W. Editorial I: Location, location, location! Ultrasound imaging in regional anaesthesia. Br J Anaesth. 2005; 94:1–3.
Article15. O'Donnell BD, Szűcs S. Peripheral nerve block and local anaesthetic dose, how much is enough? Anaesthesia. 2014; 69:665–668.16. Nader A, Kendall MC, De Oliveira GS, et al. A dose-ranging study of 0.5% bupivacaine or ropivacaine on the success and duration of the ultrasound-guided, nerve-stimulator-assisted sciatic nerve block: a double-blind, randomized clinical trial. Reg Anesth Pain Med. 2013; 38:492–502.17. Markham A, Faulds D. Ropivacaine. A review of its pharmacology and therapeutic use in regional anaesthesia. Drugs. 1996; 52:429–449.18. Krenn H, Deusch E, Balogh B, et al. Increasing the injection volume by dilution improves the onset of motor blockade, but not sensory blockade of ropivacaine for brachial plexus block. Eur J Anaesthesiol. 2003; 20:21–25.
Article19. Kimura Y, Kamada Y, Kimura A, Orimo K. Ropivacaine-induced toxicity with overdose suspected after axillary brachial plexus block. J Anesth. 2007; 21:413–416.
Article20. Satsumae T, Tanaka M, Saito S, Inomata S. Convulsions after ropivacaine 300 mg for brachial plexus block. Br J Anaesth. 2008; 101:860–862.
Article21. Wong AK, Keeney LG, Chen L, Williams R, Liu J, Elkassabany NM. Effect of local anesthetic concentration (0.2% vs 0.1% ropivacaine) on pulmonary function, and analgesia after ultrasound-guided interscalene brachial plexus block: a randomized controlled study. Pain Med. 2016; 17:2397–2403.
Article22. Schoenmakers KP, Fenten MG, Louwerens JW, Scheffer GJ, Stienstra R. The effects of adding epinephrine to ropivacaine for popliteal nerve block on the duration of postoperative analgesia: a randomized controlled trial. BMC Anesthesiol. 2015; 15:100.
Article23. Bailard NS, Ortiz J, Flores RA. Additives to local anesthetics for peripheral nerve blocks: evidence, limitations, and recommendations. Am J Health Syst Pharm. 2014; 71:373–385.
Article24. Marhofer D, Kettner SC, Marhofer P, Pils S, Weber M, Zeitlinger M. Dexmedetomidine as an adjuvant to ropivacaine prolongs peripheral nerve block: a volunteer study. Br J Anaesth. 2013; 110:438–442.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical efficacy of 0.75% ropivacaine vs. 2% lignocaine hydrochloride with adrenaline (1:80,000) in patients undergoing removal of bilateral maxillary third molars: a randomized controlled trial
- Comparison of clinical efficacy of ropivacaine and lignocaine with adrenaline for implant surgery anesthesia: a split-mouth randomized controlled clinical trial
- The Efficacy of Ultrasound-Guided Lower Extremity Nerve Block in Trauma Patients
- Spinal Anesthesia with 0.75% Isobaric Ropivacaine for Lower Extremity Operation
- Comparison between two different concentrations of a fixed dose of ropivacaine in interscalene brachial plexus block for pain management after arthroscopic shoulder surgery: a randomized clinical trial