J Korean Neurosurg Soc.
2018 Nov;61(6):707-715. 10.3340/jkns.2017.0296.
Does the Access Angle Change the Risk of Approach-Related Complications in Minimally Invasive Lateral Lumbar Interbody Fusion? An MRI Study
- Affiliations
-
- 1Department of Orthopaedic Surgery, The Second Affiliated Hospital of Zhejiang University School of Medicine, Hangzhou, China. zrcqx@zju.edu.cn
- KMID: 2428112
- DOI: http://doi.org/10.3340/jkns.2017.0296
Abstract
OBJECTIVE
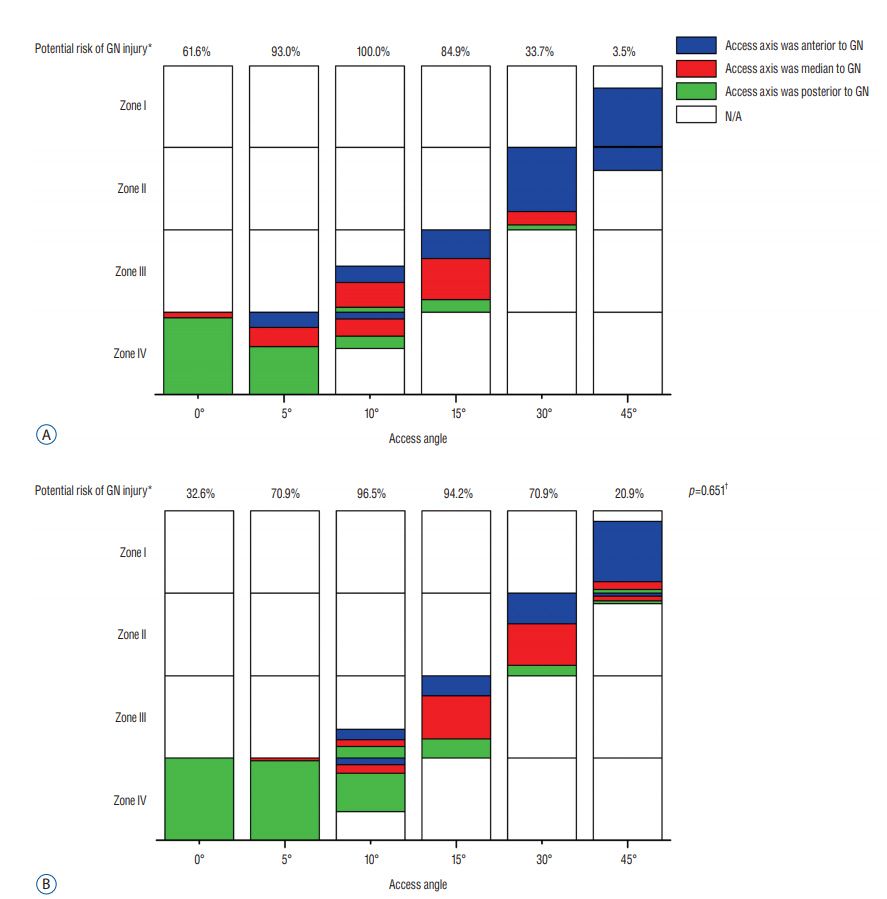
To investigate the potential risk of approach-related complications at different access angles in minimally invasive lateral lumbar interbody fusion.
METHODS
Eighty-six axial magnetic resonance images were obtained to analyze the risk of approach-related complications. The access corridor were simulated at different access angles and the potential risk of neurovascular structure injury was evaluated when the access corridor touching or overlapping the corresponding structures at each angle. Furthermore, the safe corridor length was measured when the corridor width was 18 and 22 mm.
RESULTS
When access angle was 0°, the potential risk of ipsilateral nerve roots injury was 54.7% at L4-L5. When access angle was 45°, the potential risk of abdominal aorta, contralateral nerve roots or central canal injury at L4-L5 was 79.1%, 74.4%, and 30.2%, respectively. The length of the 18 mm-wide access corridor was largest at 0° and it could reach 44.5 mm at L3-L4 and 46.4 mm at L4-L5. While the length of the 22 mm-wide access corridor was 42.3 mm at L3-L4 and 44.1 mm at L4-L5 at 0°.
CONCLUSION
Changes in the access angle would not only affect the ipsilateral neurovascular structures, but also might adversely influence the contralateral neural elements. It should be also noted to surgeons that alteration of the access angle changed the corridor length.
Keyword
Figure
Cited by 2 articles
-
Learning Curve and Complications Experience of Oblique Lateral Interbody Fusion : A Single-Center 143 Consecutive Cases
Bu Kwang Oh, Dong Wuk Son, Su Hun Lee, Jun Seok Lee, Soon Ki Sung, Sang Weon Lee, Geun Sung Song
J Korean Neurosurg Soc. 2021;64(3):447-459. doi: 10.3340/jkns.2020.0342.A Comprehensive Analysis of Potential Complications after Oblique Lumbar Interbody Fusion : A Review of Postoperative Magnetic Resonance Scans in Over 400 Cases
Kang-Hoon Lee, Su-Hun Lee, Jun-Seok Lee, Young-Ha Kim, Soon-Ki Sung, Dong-Wuk Son, Sang-Weon Lee, Geun-Sung Song
J Korean Neurosurg Soc. 2024;67(5):550-559. doi: 10.3340/jkns.2023.0238.
Reference
-
References
1. Abe K, Orita S, Mannoji C, Motegi H, Aramomi M, Ishikawa T, et al. Perioperative complications in 155 patients who underwent oblique lateral interbody fusion surgery: perspectives and indications from a retrospective, multicenter survey. Spine (Phila Pa 1976). 42:55–62. 2017.
Article2. Ahmadian A, Deukmedjian AR, Abel N, Dakwar E, Uribe JS. Analysis of lumbar plexopathies and nerve injury after lateral retroperitoneal transpsoas approach: diagnostic standardization. J Neurosurg Spine. 18:289–297. 2013.
Article3. Aichmair A, Fantini GA, Garvin S, Beckman J, Girardi FP. Aortic perforation during lateral lumbar interbody fusion. J Spinal Disord Tech. 28:71–75. 2015.
Article4. Anand N, Rosemann R, Khalsa B, Baron EM. Mid-term to long-term clinical and functional outcomes of minimally invasive correction and fusion for adults with scoliosis. Neurosurg Focus. 28:E6. 2010.
Article5. Assina R, Majmundar NJ, Herschman Y, Heary RF. First report of major vascular injury due to lateral transpsoas approach leading to fatality. J Neurosurg Spine. 21:794–798. 2014.
Article6. Banagan K, Gelb D, Poelstra K, Ludwig S. Anatomic mapping of lumbar nerve roots during a direct lateral transpsoas approach to the spine: a cadaveric study. Spine (Phila Pa 1976). 36:E687–E691. 2011.7. Beckman JM, Vincent B, Park MS, Billys JB, Isaacs RE, Pimenta L, et al. Contralateral psoas hematoma after minimally invasive, lateral retroperitoneal transpsoas lumbar interbody fusion: a multicenter review of 3950 lumbar levels. J Neurosurg Spine. 26:50–54. 2017.
Article8. Berjano P, Balsano M, Buric J, Petruzzi M, Lamartina C. Direct lateral access lumbar and thoracolumbar fusion: preliminary results. Eur Spine J 21 Suppl. 1:S37–S42. 2012.
Article9. Chang J, Kim JS, Jo H. Ventral dural injury after oblique lumbar interbody fusion. World Neurosurg. 98:881.e1–881.e4. 2017.
Article10. Fujibayashi S, Kawakami N, Asazuma T, Ito M, Mizutani J, Nagashima H, et al. Complications associated with lateral interbody fusion: nationwide survey of 2998 cases during the first two years of its use in Japan. Spine (Phila Pa 1976). 42:1478–1484. 2017.
Article11. Guérin P, Obeid I, Gille O, Bourghli A, Luc S, Pointillart V, et al. Safe working zones using the minimally invasive lateral retroperitoneal transpsoas approach: a morphometric study. Surg Radiol Anat. 33:665–671. 2011.
Article12. He L, Kang Z, Tang WJ, Rong LM. A MRI study of lumbar plexus with respect to the lateral transpsoas approach to the lumbar spine. Eur Spine J. 24:2538–2545. 2015.
Article13. Hijji FY, Narain AS, Bohl DD, Ahn J, Long WW, DiBattista JV, et al. Lateral lumbar interbody fusion: a systematic review of complication rates. Spine J. 17:1412–1419. 2017.
Article14. Kepler CK, Bogner EA, Herzog RJ, Huang RC. Anatomy of the psoas muscle and lumbar plexus with respect to the surgical approach for lateral transpsoas interbody fusion. Eur Spine J. 20:550–556. 2011.
Article15. Kim JS, Choi WS, Sung JH. 314 minimally invasive oblique lateral interbody fusion for L4-5: clinical outcomes and perioperative complications. Neurosurgery 63 Suppl. 1:190–191. 2016.16. Le TV, Baaj AA, Dakwar E, Burkett CJ, Murray G, Smith DA, et al. Subsidence of polyetheretherketone intervertebral cages in minimally invasive lateral retroperitoneal transpsoas lumbar interbody fusion. Spine (Phila Pa 1976). 37:1268–1273. 2012.
Article17. Marchi L, Abdala N, Oliveira L, Amaral R, Coutinho E, Pimenta L. Radiographic and clinical evaluation of cage subsidence after stand-alone lateral interbody fusion. J Neurosurg Spine. 19:110–118. 2013.
Article18. Moller DJ, Slimack NP, Acosta FL Jr, Koski TR, Fessler RG, Liu JC. Minimally invasive lateral lumbar interbody fusion and transpsoas approachrelated morbidity. Neurosurg Focus. 31:E4. 2011.
Article19. Molloy S, Butler JS, Benton A, Malhotra K, Selvadurai S, Agu O. A new extensile anterolateral retroperitoneal approach for lumbar interbody fusion from L1 to S1: a prospective series with clinical outcomes. Spine J. 16:786–791. 2016.
Article20. O’Brien J, Haines C, Dooley ZA, Turner AW, Jackson D. Femoral nerve strain at L4-L5 is minimized by hip flexion and increased by table break when performing lateral interbody fusion. Spine (Phila Pa 1976). 39:33–38. 2014.
Article21. Ozgur BM, Aryan HE, Pimenta L, Taylor WR. Extreme lateral interbody fusion (XLIF): a novel surgical technique for anterior lumbar interbody fusion. Spine J. 6:435–443. 2006.
Article22. Papanastassiou ID, Eleraky M, Vrionis FD. Contralateral femoral nerve compression: An unrecognized complication after extreme lateral interbody fusion (XLIF). J Clin Neurosci. 18:149–151. 2011.
Article23. Phan K, Maharaj M, Assem Y, Mobbs RJ. Review of early clinical results and complications associated with oblique lumbar interbody fusion (OLIF). J Clin Neurosci. 31:23–29. 2016.
Article24. Regev GJ, Haloman S, Chen L, Dhawan M, Lee YP, Garfin SR, et al. Incidence and prevention of intervertebral cage overhang with minimally invasive lateral approach fusions. Spine (Phila Pa 1976). 35:1406–1411. 2010.
Article25. Taher F, Hughes AP, Lebl DR, Sama AA, Pumberger M, Aichmair A, et al. Contralateral motor deficits after lateral lumbar interbody fusion. Spine (Phila Pa 1976). 38:1959–1963. 2013.
Article26. Yusof MI, Nadarajan E, Abdullah MS. The morphometric study of l3-L4 and L4-L5 lumbar spine in Asian population using magnetic resonance imaging: feasibility analysis for transpsoas lumbar interbody fusion. Spine (Phila Pa 1976). 39:E811–E816. 2014.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Minimally Invasive Lateral Lumbar Interbody Fusion: Indications, Outcomes and Complications
- Lateral Lumbar Interbody Fusion
- Minimally Invasive Strategy for Uniportal Full-Endoscopic Transforaminal Lumbar Interbody Fusion Using a Large Cage Utilized in Oblique Lumbar Interbody Fusion
- Minimally Invasive Lateral Lumbar Interbody Fusion: Surgical Technique and Review
- Minimally Invasive Transforaminal Lumbar Interbody Fusion with the Space-D Access System