Korean J Radiol.
2017 Apr;18(2):336-344. 10.3348/kjr.2017.18.2.336.
Variations in the Origin of Inferior Phrenic Arteries and Their Relationship to Celiac Axis Variations on CT Angiography
- Affiliations
-
- 1Department of Radiology, Tepecik Training and Research Hospital, Izmir 35110, Turkey. yelizpekcevik@yahoo.com
- 2Hacettepe University, Statistics Department, Ankara 06800, Turkey.
- KMID: 2427945
- DOI: http://doi.org/10.3348/kjr.2017.18.2.336
Abstract
OBJECTIVE
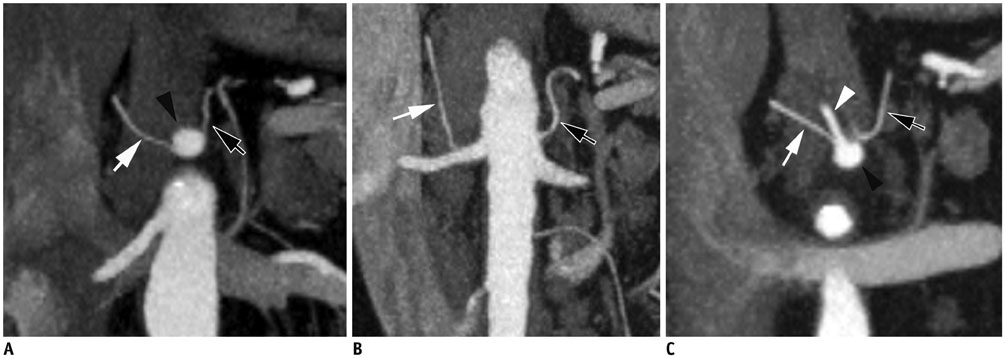
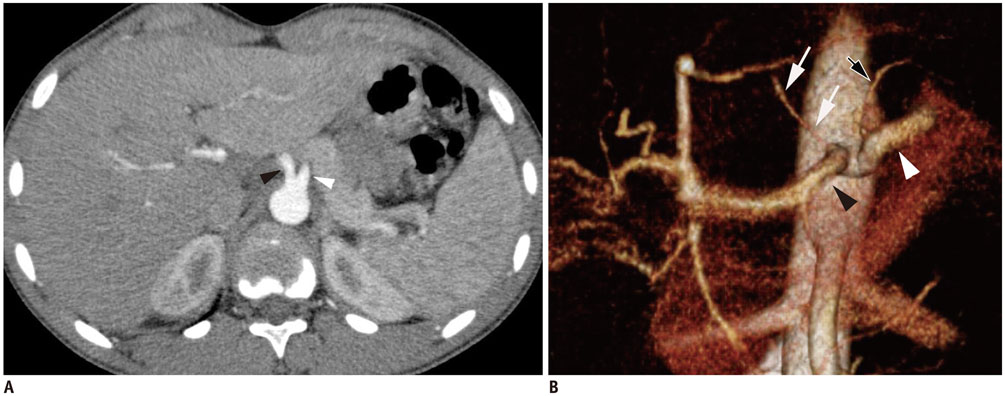
Knowing the origin of the inferior phrenic artery (IPA) is important prior to surgical interventions and interventional radiological procedures related to IPA. We aimed to identify variations in the origin of IPA and to investigate the relationship between the origin of IPA and celiac axis variations using computed tomography angiography (CTA).
MATERIALS AND METHODS
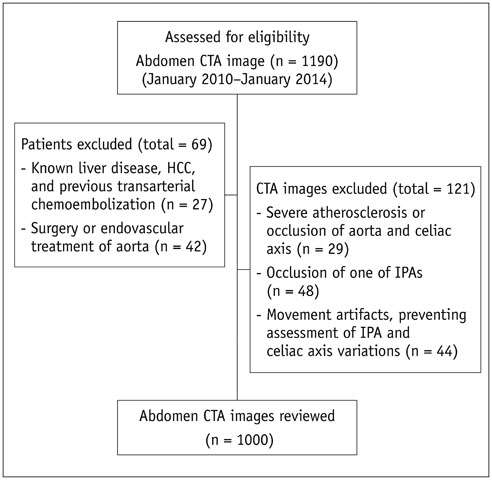
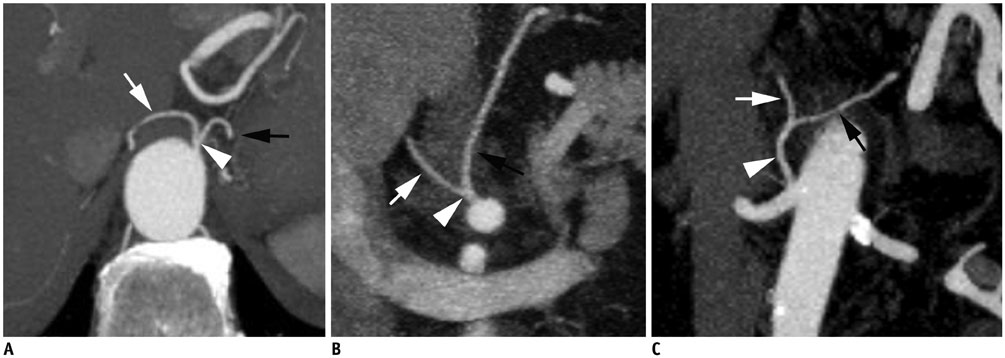
The CTA images of 1000 patients (737 male and 263 female, the mean age 60, range 18-94 years) were reviewed in an analysis of IPA and celiac axis variations. The origin of IPA was divided into two groups, those originating as a common trunk and those originating independently without a truncus. The relationship between the origin of IPA and celiac axis variation was analyzed using Pearson's chi-square test.
RESULTS
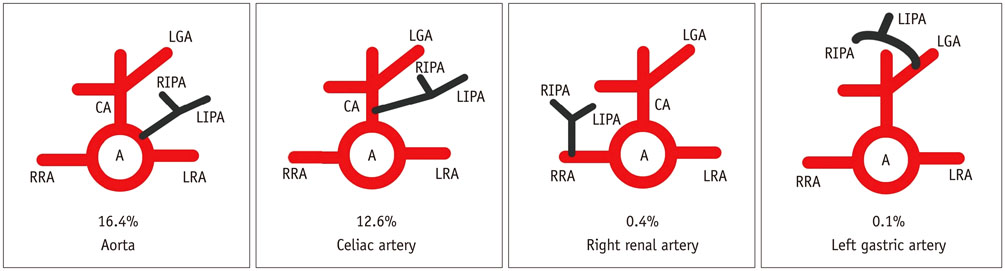
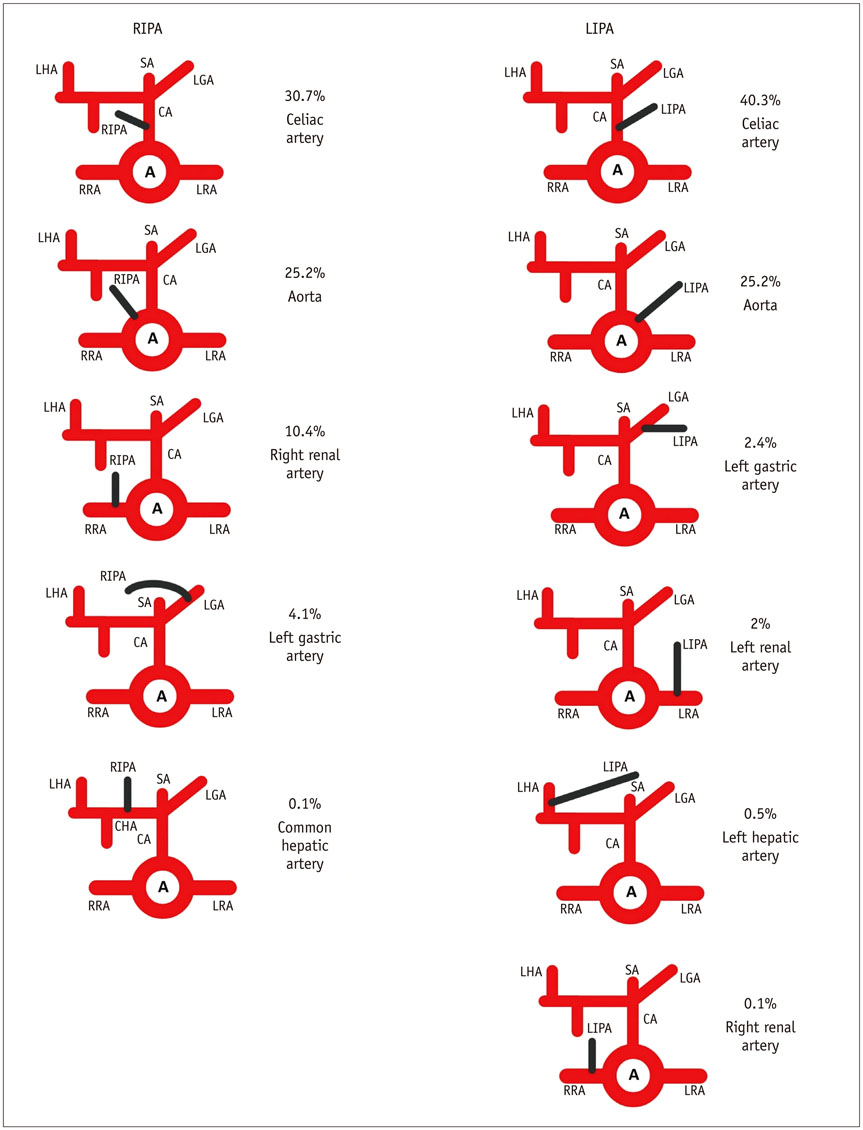
Both IPAs originated from a common trunk in 295 (29.5%) patients. From which the majority of the common trunk originated from the aorta. Contrastingly, the inferior phrenic arteries originated from different origins in 705 (70.5%) patients. The majority of the right inferior phrenic artery (RIPA) and the left inferior phrenic artery (LIPA) originated independently from the celiac axis. Variation in the celiac axis were detected in 110 (11%) patients. The origin of IPA was found to be significantly different in the presence of celiac axis variation.
CONCLUSION
The majority of IPA originated from the aorta in patients with a common IPA trunk, while the majority of RIPA and LIPA originating from the celiac axis in patients without a common IPA trunk. Thus, the origin of IPA may widely differ in the presence of celiac axis variation.
Keyword
MeSH Terms
-
Adolescent
Adult
Aged
Aged, 80 and over
Aorta/anatomy & histology/*diagnostic imaging
Celiac Artery/anatomy & histology/*diagnostic imaging
*Computed Tomography Angiography
Contrast Media/chemistry
Female
Humans
Imaging, Three-Dimensional
Iodine/chemistry
Male
Middle Aged
Retrospective Studies
Young Adult
Contrast Media
Iodine
Figure
Cited by 1 articles
-
Age of Data in Contemporary Research Articles Published in Representative General Radiology Journals
Ji Hun Kang, Dong Hwan Kim, Seong Ho Park, Jung Hwan Baek
Korean J Radiol. 2018;19(6):1172-1178. doi: 10.3348/kjr.2018.19.6.1172.
Reference
-
1. Gwon DI, Ko GY, Yoon HK, Sung KB, Lee JM, Ryu SJ, et al. Inferior phrenic artery: anatomy, variations, pathologic conditions, and interventional management. Radiographics. 2007; 27:687–705.2. Liu PS, Platt JF. CT angiography in the abdomen: a pictorial review and update. Abdom Imaging. 2014; 39:196–214.3. Lee AJ, Gomes AS, Liu DM, Kee ST, Loh CT, McWilliams JP. The road less traveled: importance of the lesser branches of the celiac axis in liver embolotherapy. Radiographics. 2012; 32:1121–1132.4. Basile A, Tsetis D, Montineri A, Puleo S, Massa Saluzzo C, Runza G, et al. MDCT anatomic assessment of right inferior phrenic artery origin related to potential supply to hepatocellular carcinoma and its embolization. Cardiovasc Intervent Radiol. 2008; 31:349–358.5. Gürses İA, Gayretli Ö, Kale A, Öztürk A, Usta A, Şahinoğlu K. Inferior phrenic arteries and their branches, their anatomy and possible clinical importance: an experimental cadaver study. Balkan Med J. 2015; 32:189–195.6. Lee JW, Kim S, Kim CW, Kim KH, Jeon TY. Massive hemoperitoneum due to ruptured inferior phrenic artery pseudoaneurysm after blunt trauma. Emerg Radiol. 2006; 13:147–149.7. Loukas M, Hullett J, Wagner T. Clinical anatomy of the inferior phrenic artery. Clin Anat. 2005; 18:357–365.8. Takanami I. Massive haemoptysis due to chronic pancreatitis: control with inferior phrenic artery embolization. Eur J Cardiothorac Surg. 2000; 18:120–122.9. Arora A, Tyagi P, Gupta A, Arora V, Sharma P, Kumar M, et al. Pseudoaneurysm of the inferior phrenic artery presenting as an upper gastrointestinal bleed by directly rupturing into the stomach in a patient with chronic pancreatitis. Ann Vasc Surg. 2012; 26:860.e9–860.e11.10. Hong SS, Kim AY. Early postoperative bleeding after living donor liver transplantation. Abdom Imaging. 2009; 34:365–370.11. Ozbulbul NI, Yurdakul M, Tola M, Akdogan G, Olcer T. Can multidetector row CT visualize the right and left inferior phrenic artery in a population without disease of the liver? Surg Radiol Anat. 2009; 31:681–685.12. Song SY, Chung JW, Yin YH, Jae HJ, Kim HC, Jeon UB, et al. Celiac axis and common hepatic artery variations in 5002 patients: systematic analysis with spiral CT and DSA. Radiology. 2010; 255:278–288.13. Hieda M, Toyota N, Kakizawa H, Ishikawa M, Horiguchi J, Ito K. The anterior branch of the left inferior phrenic artery arising from the right inferior phrenic artery: an angiographic and CT study. Cardiovasc Intervent Radiol. 2009; 32:250–254.14. Miclaus GD, Matusz P, Loukas M, Ples H. Rare case of the trunk of the inferior phrenic arteries originating from a common stem with a superior additional left renal artery from the abdominal aorta. Clin Anat. 2012; 25:979–982.15. Tanaka R, Ibukuro K, Akita K. The left inferior phrenic artery arising from left hepatic artery or left gastric artery: radiological and anatomical correlation in clinical cases and cadaver dissection. Abdom Imaging. 2008; 33:328–333.16. Gonsalves CF, Brown DB. Chemoembolization of hepatic malignancy. Abdom Imaging. 2009; 34:557–565.17. Kim HC, Chung JW, An S, Seong NJ, Jae HJ, Cho BH, et al. Left inferior phrenic artery feeding hepatocellular carcinoma: angiographic anatomy using C-arm CT. AJR Am J Roentgenol. 2009; 193:W288–W294.18. Jones BV, Vu D. Diagnosis of posttraumatic pericardial tamponade by plain film and computed tomography and control of bleeding by embolotherapy of the left inferior phrenic artery. Cardiovasc Intervent Radiol. 1993; 16:183–185.19. Zeng R, Yao Z, Chen Y, Xu Z, Chen Y, Liu J. Variant arterial supply to the lesser curvature of the stomach and duodenum from double inferior phrenic arteries. Surg Radiol Anat. 2015; 37:867–869.20. Mu GC, Huang Y, Liu ZM, Lin JL, Zhang LL, Zeng YJ. Clinical research in individual information of celiac artery CT imaging and gastric cancer surgery. Clin Transl Oncol. 2013; 15:774–779.21. Ozbülbül NI. CT angiography of the celiac trunk: anatomy, variants and pathologic findings. Diagn Interv Radiol. 2011; 17:150–157.22. Iezzi R, Cotroneo AR, Giancristofaro D, Santoro M, Storto ML. Multidetector-row CT angiographic imaging of the celiac trunk: anatomy and normal variants. Surg Radiol Anat. 2008; 30:303–310.23. Winston CB, Lee NA, Jarnagin WR, Teitcher J, DeMatteo RP, Fong Y, et al. CT angiography for delineation of celiac and superior mesenteric artery variants in patients undergoing hepatobiliary and pancreatic surgery. AJR Am J Roentgenol. 2007; 189:W13–W19.24. So YH, Chung JW, Yin Y, Jae HJ, Jeon UB, Cho BH, et al. The right inferior phrenic artery: origin and proximal anatomy on digital subtraction angiography and thin-section helical computed tomography. J Vasc Interv Radiol. 2009; 20:1164–1171.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Prevalence and clinical relevance of the anatomical variations of suprarenal arteries: a review
- Prevalence of anatomical variants in the branches of celiac and superior mesenteric arteries among Egyptians
- Variations in the branching pattern of the celiac trunk and its clinical significance
- Entirely Replaced Left Gastric Artery from the Left Hepatic Artery: A Case Report
- Study of course and termination of brachial artery by dissection and computed tomography angiography methods with clinical importance