Korean J Leg Med.
2018 Nov;42(4):153-158. 10.7580/kjlm.2018.42.4.153.
Unexpected Death by Sepsis of Staphylococcus aureus with Infective Endocarditis and Paravertebral Abscess in a Fisherman during Sailing out for Fish: An Autopsy Case
- Affiliations
-
- 1Department of Forensic Medicine, Chosun University School of Medicine, Gwangju, Korea. ysk007fm@hotmail.com
- 2Forensic DNA Division, National Forensic Service, Wonju, Korea.
- 3Forensic Medicine Division, National Forensic Service Gwangju Institute, Jangseong, Korea.
- KMID: 2427562
- DOI: http://doi.org/10.7580/kjlm.2018.42.4.153
Abstract
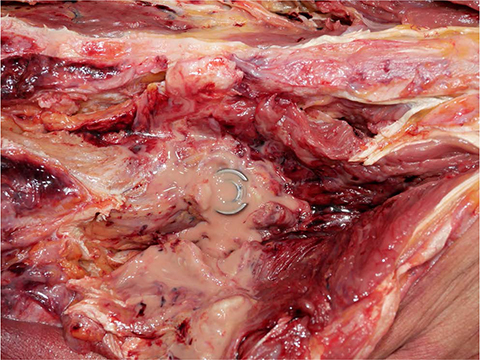
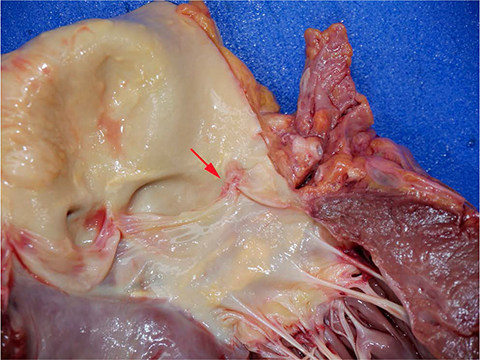
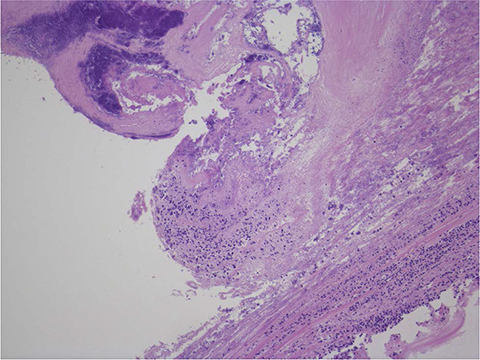
- Staphylococcus aureus is an important cause of human infections, and it is also a commensal that colonizes the nose, axillae, vagina, throat, or skin surfaces. S. aureus has increasingly been recognized as a cause of severe invasive illness, and individuals colonized with this pathogen are subsequently at increased risk of its infections. S. aureus infection is a major cause of skin, soft tissue, respiratory, bone, joint, and endovascular disorders, and staphylococcal bacteremia may cause abscess, endocarditis, pneumonia, metastatic infection, foreign body infection, or sepsis. The authors describe a case of a fisherman who died of sepsis on a fishing boat during sailing out for fish. The autopsy shows paravertebral abscess, pus in the pericardial sac, infective endocarditis with vegetation on the aortic valve cusp, myocarditis, pneumonia and nephritis with bacterial colonization, and also liver cirrhosis and multiple gastric ulcerations.
MeSH Terms
Figure
Reference
-
1. Lowy FD. Staphylococcus aureus infections. N Engl J Med. 1998; 339:520–532.2. Noble WC, Valkenburg HA, Wolters CH. Carriage of Staphylococcus aureus in random samples of a normal population. J Hyg (Lond). 1967; 65:567–573.3. Wenzel RP, Perl TM. The significance of nasal carriage of Staphylococcus aureus and the incidence of postoperative wound infection. J Hosp Infect. 1995; 31:13–24.4. Fowler VG Jr, Miro JM, Hoen B, et al. Staphylococcus aureus endocarditis: a consequence of medical progress. JAMA. 2005; 293:3012–3021.5. Roder BL, Wandall DA, Frimodt-Moller N, et al. Clinical features of Staphylococcus aureus endocarditis: a 10-year experience in Denmark. Arch Intern Med. 1999; 159:462–469.6. Chambers HF, Korzeniowski OM, Sande MA. Staphylococcus aureus endocarditis: clinical manifestations in addicts and nonaddicts. Medicine (Baltimore). 1983; 62:170–177.7. Bone RC. Gram-positive organisms and sepsis. Arch Intern Med. 1994; 154:26–34.
Article8. Libman H, Arbeit RD. Complications associated with Staphylococcus aureus bacteremia. Arch Intern Med. 1984; 144:541–545.9. Zimmerli W, Waldvogel FA, Vaudaux P, et al. Pathogenesis of foreign body infection: description and characteristics of an animal model. J Infect Dis. 1982; 146:487–497.
Article10. Zimmerli W, Lew PD, Waldvogel FA. Pathogenesis of foreign body infection: evidence for a local granulocyte defect. J Clin Invest. 1984; 73:1191–1200.
Article11. Elek SD, Conen PE. The virulence of Staphylococcus pyogenes for man: a study of the problems of wound infection. Br J Exp Pathol. 1957; 38:573–586.12. Adem PV, Montgomery CP, Husain AN, et al. Staphylococcus aureus sepsis and the Waterhouse-Friderichsen syndrome in children. N Engl J Med. 2005; 353:1245–1251.13. Lee JM, Hwang JH, Yi DY, et al. Aggressively progressed MRSA sepsis accompanied by endophthalmitis and endocarditis in preterm infant. Korean J Perinatol. 2015; 26:369–372.
Article14. Melzer M, Eykyn SJ, Gransden WR, et al. Is methicillin-resistant Staphylococcus aureus more virulent than methicillin-susceptible S. aureus? A comparative cohort study of British patients with nosocomial infection and bacteremia. Clin Infect Dis. 2003; 37:1453–1460.15. Williams RE. Healthy carriage of Staphylococcus aureus: its prevalence and importance. Bacteriol Rev. 1963; 27:56–71.16. Kluytmans J, van Belkum A, Verbrugh H. Nasal carriage of Staphylococcus aureus: epidemiology, underlying mechanisms, and associated risks. Clin Microbiol Rev. 1997; 10:505–520.17. Sherertz RJ, Bassetti S, Bassetti-Wyss B. “Cloud” health-care workers. Emerg Infect Dis. 2001; 7:241–244.
Article18. Sattler CA, Correa AG. Coagulase-positive staphylococcal infections (Staphylococcus aureus). In : Feigin RD, Cherry JD, Demmler GJ, Kaplan SL, editors. Textbook of pediatric infectious diseases. Vol. 1. 5th ed. Philadelphia, PA: Saunders;2004. p. 1099–1129.19. Gonzalez BE, Hulten KG, Dishop MK, et al. Pulmonary manifestations in children with invasive community-acquired Staphylococcus aureus infection. Clin Infect Dis. 2005; 41:583–590.20. Sandre RM, Shafran SD. Infective endocarditis: review of 135 cases over 9 years. Clin Infect Dis. 1996; 22:276–286.
Article21. Sanabria TJ, Alpert JS, Goldberg R, et al. Increasing frequency of staphylococcal infective endocarditis: experience at a university hospital, 1981 through 1988. Arch Intern Med. 1990; 150:1305–1309.
Article22. Decker MD, Lybarger JA, Vaughn WK, et al. An outbreak of staphylococcal skin infections among river rafting guides. Am J Epidemiol. 1986; 124:969–976.
Article23. David MZ, Daum RS. Community-associated methicillin-resistant Staphylococcus aureus: epidemiology and clinical consequences of an emerging epidemic. Clin Microbiol Rev. 2010; 23:616–687.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Neonatal Infective Endocarditis without Cardiac Anomaly
- Fatal Peripheral Septic Thrombophlebitis Complicated with Infective Endocarditis due to Methicillin-resistant Staphylococcus aureus: A Case Report with Autopsy Findings
- A Case of Psoas Abscess Caused by Staphylococcus lugdunensis
- A Fatal Case of Infective Endocarditis Caused by Community-Associated Methicillin-Resistant Staphylococcus aureus ST72 in Korea
- A Case of Infective Endocarditis in an End-Stage Renal Disease Patient Caused by Candida famata