Allergy Asthma Respir Dis.
2018 Nov;6(6):290-294. 10.4168/aard.2018.6.6.290.
Clinical presentation of croup in children according to causative viruses
- Affiliations
-
- 1Department of Pediatrics, Keimyung University Dongsan Medical Center, Daegu, Korea. bbbbb0825@hanmail.net
- KMID: 2427487
- DOI: http://doi.org/10.4168/aard.2018.6.6.290
Abstract
- PURPOSE
We evaluated the clinical features of croup in children according to viral etiology.
METHODS
This study enrolled pediatric patients with croup, who showed positive results on respiratory virus reverse transcriptase polymerase chain reaction performed between January 2012 and December 2017. We retrospectively reviewed the medical records.
RESULTS
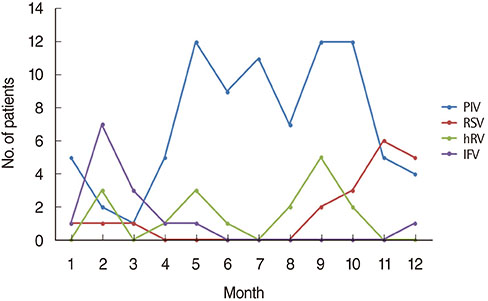
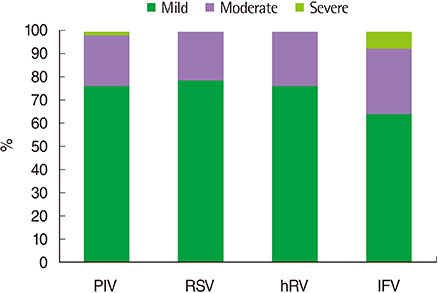
A total of 179 patients (119 boys and 60 girls) were enrolled with the mean age of 18.9±14.7 months. The viruses commonly identified were parainfluenza, respiratory syncytial virus, rhinovirus, and influenza. Among these 4 viruses, patients with rhinovirus infection showed significantly shorter fever and admission durations. Patients with parainfluenza infection showed significantly lower incidences of epinephrine nebulization and patients with influenza infections showed significantly higher incidences of steroid treatment.
CONCLUSION
Clinical manifestations of croup differ according to causative viruses. Further studies should be conducted to evaluate the severity and prognosis of croup according to viral etiology.
Keyword
MeSH Terms
Figure
Reference
-
1. Johnson DW. Croup. BMJ Clin Evid. 2014; 2014.2. Bjornson CL, Johnson DW. Croup in children. CMAJ. 2013; 185:1317–1323.
Article3. Marx A, Török TJ, Holman RC, Clarke MJ, Anderson LJ. Pediatric hospitalizations for croup (laryngotracheobronchitis): biennial increases associated with human parainfluenza virus 1 epidemics. J Infect Dis. 1997; 176:1423–1427.
Article4. Zoorob R, Sidani M, Murray J. Croup: an overview. Am Fam Physician. 2011; 83:1067–1073.5. Denny FW, Murphy TF, Clyde WA Jr, Collier AM, Henderson FW. Croup: an 11-year study in a pediatric practice. Pediatrics. 1983; 71:871–876.
Article6. Williams JV, Harris PA, Tollefson SJ, Halburnt-Rush LL, Pingsterhaus JM, Edwards KM, et al. Human metapneumovirus and lower respiratory tract disease in otherwise healthy infants and children. N Engl J Med. 2004; 350:443–450.
Article7. Jeon IS, Cho WJ, Lee J, Kim HM. Epidemiology and clinical severity of the hospitalized children with viral croup. Pediatr Infect Vaccine. 2018; 25:8–16.
Article8. Miller EK, Gebretsadik T, Carroll KN, Dupont WD, Mohamed YA, Morin LL, et al. Viral etiologies of infant bronchiolitis, croup and upper respiratory illness during 4 consecutive years. Pediatr Infect Dis J. 2013; 32:950–955.
Article9. Sung JY, Lee HJ, Eun BW, Kim SH, Lee SY, Lee JY, et al. Role of human coronavirus NL63 in hospitalized children with croup. Pediatr Infect Dis J. 2010; 29:822–826.
Article10. Kim EJ, Nam H, Sun YH, Tchah H, Ryoo E, Cho HK, et al. Comparison of etiology and clinical presentation between children with laryngotracheobronchopneumonitis and croup. Allergy Asthma Respir Dis. 2017; 5:274–279.
Article11. Peltola V, Heikkinen T, Ruuskanen O. Clinical courses of croup caused by influenza and parainfluenza viruses. Pediatr Infect Dis J. 2002; 21:76–78.
Article12. Rihkanen H, Rönkkö E, Nieminen T, Komsi KL, Räty R, Saxen H, et al. Respiratory viruses in laryngeal croup of young children. J Pediatr. 2008; 152:661–665.
Article13. Yang WC, Lee J, Chen CY, Chang YJ, Wu HP. Westley score and clinical factors in predicting the outcome of croup in the pediatric emergency department. Pediatr Pulmonol. 2017; 52:1329–1334.
Article14. Westley CR, Cotton EK, Brooks JG. Nebulized racemic epinephrine by IPPB for the treatment of croup: a double-blind study. Am J Dis Child. 1978; 132:484–487.
Article15. Henrickson KJ, Hoover S, Kehl KS, Hua W. National disease burden of respiratory viruses detected in children by polymerase chain reaction. Pediatr Infect Dis J. 2004; 23:1 Suppl. S11–S18.
Article16. Pawełczyk M, Kowalski ML. The role of human parainfluenza virus infections in the immunopathology of the respiratory tract. Curr Allergy Asthma Rep. 2017; 17:16.
Article17. Kim SH, Huh JH, Bae SY, Kim JS, Yoon SY, Lim CS, et al. Epidemiology of respiratory viral infection in 2004-2006. Korean J Lab Med. 2006; 26:351–357.
Article18. Choi E, Ha KS, Song DJ, Lee JH, Lee KC. Clinical and laboratory profiles of hospitalized children with acute respiratory virus infection. Korean J Pediatr. 2018; 61:180–186.
Article19. Bjornson CL, Johnson DW. Croup in the paediatric emergency department. Paediatr Child Health. 2007; 12:473–477.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of etiology and clinical presentation between children with laryngotracheobronchopneumonitis and croup
- Clinical features of croups caused by severe acute respiratory syndrome coronavirus 2 and by other respiratory viruses: analysis in a tertiary hospital in Jinju, Korea during the period of dominance of the Omicron variant (B.1.1.529)
- Seasonality and etiology of croup in pediatric patients hospitalized with lower respiratory tract infections: A long-term study between 2009 and 2017
- Epidemiology and Clinical Severity of the Hospitalized Children with Viral Croup
- An Epidemiological Study of Acute Viral Lower Respiratory Tract Infections in Hospitalized Children from 2002 to 2006 in Seoul, Korea