Korean J Radiol.
2017 Jun;18(3):519-525. 10.3348/kjr.2017.18.3.519.
Effectiveness of Ambulatory Tru-Close Thoracic Vent for the Outpatient Management of Pneumothorax: A Prospective Pilot Study
- Affiliations
-
- 1Department of Radiology and Research Institute of Radiological Science, Gangnam Severance Hospital, Yonsei University Health System, Seoul 06273, Korea. doctorlkh@yuhs.ac
- 2Department of Cardiothoracic Surgery, Ajou University Hospital, Suwon 16499, Korea.
- 3Department of Cardiothoracic Surgery, Gangnam Severance Hospital, Yonsei University Health System, Seoul 06273, Korea.
- KMID: 2427307
- DOI: http://doi.org/10.3348/kjr.2017.18.3.519
Abstract
OBJECTIVE
This study aimed to assess the technical feasibility, procedural safety, and long-term therapeutic efficacy of a small-sized ambulatory thoracic vent (TV) device for the treatment of pneumothorax.
MATERIALS AND METHODS
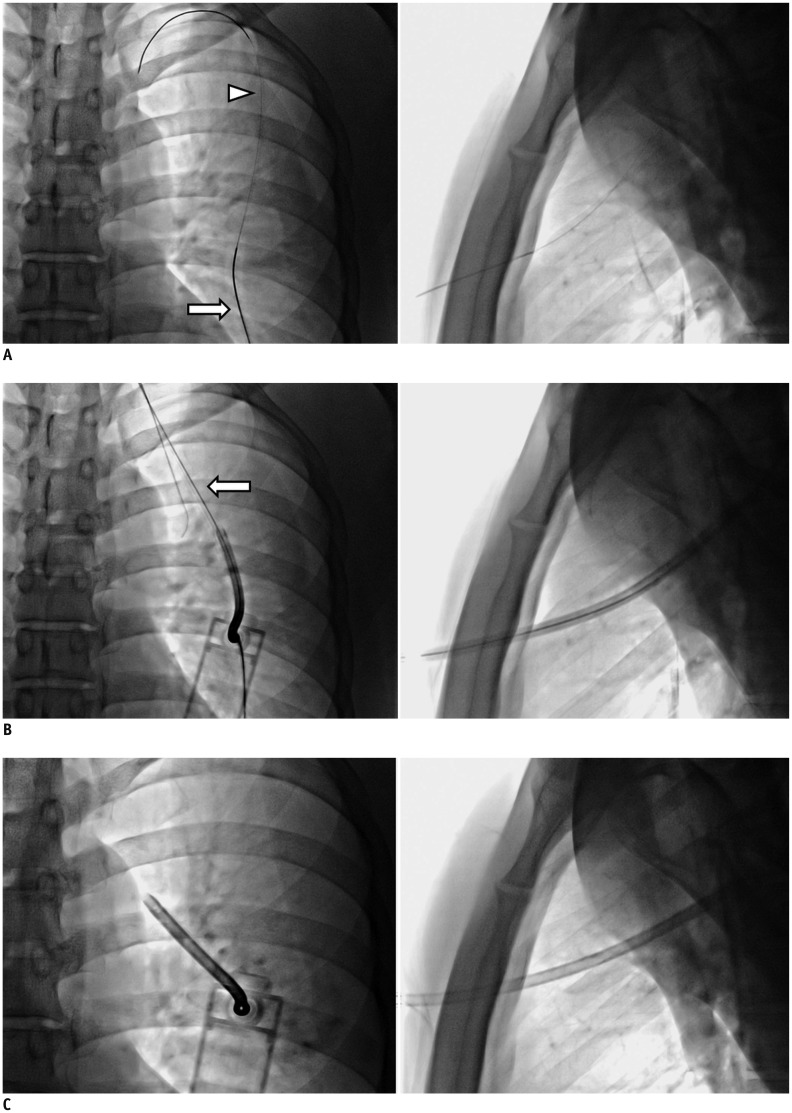
From November 2012 to July 2013, 18 consecutive patients (3 females, 15 males) aged 16-64 years (mean: 34.7 ± 14.9 years, median: 29 years) were enrolled prospectively. Of these, 15 patients had spontaneous pneumothorax and 3 had iatrogenic pneumothorax. A Tru-Close TV with a small-bore (11- or 13-Fr) catheter was inserted under bi-plane fluoroscopic assistance.
RESULTS
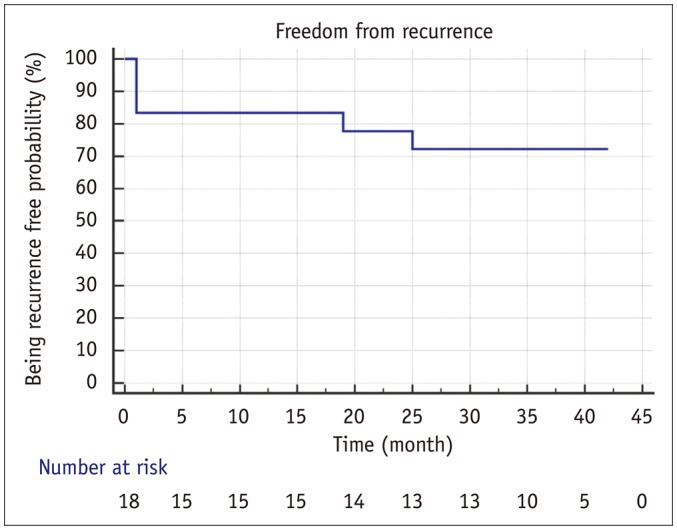
Technical success was achieved in all patients. Complete lung re-expansion was achieved at 24 hours in 88.9% of patients (16/18 patients). All patients tolerated the procedure and no major complications occurred. The patients' mean numeric pain intensity score was 2.4 (range: 0-5) in daily life activity during the TV treatment. All patients with spontaneous pneumothorax underwent outpatient follow-up. The mean time to TV removal was 4.7 (3-13) days. Early surgical conversion rate of 16.7% (3/18 patients) occurred in 2 patients with incomplete lung expansion and 1 patient with immediate pneumothorax recurrence post-TV removal; and late surgical conversion occurred in 2 of 18 patients (11.1%). The recurrence-free long-term success rate was 72.2% (13/18 patients) during a 3-year follow-up period from November 2012 to June 2016.
CONCLUSION
TV application was a simple, safe, and technically feasible procedure in an outpatient clinic, with an acceptable long-term recurrence-free rate. Thus, TV could be useful for the immediate treatment of pneumothorax.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Age of Data in Contemporary Research Articles Published in Representative General Radiology Journals
Ji Hun Kang, Dong Hwan Kim, Seong Ho Park, Jung Hwan Baek
Korean J Radiol. 2018;19(6):1172-1178. doi: 10.3348/kjr.2018.19.6.1172.
Reference
-
1. Melton LJ 3rd, Hepper NG, Offord KP. Incidence of spontaneous pneumothorax in Olmsted County, Minnesota: 1950 to 1974. Am Rev Respir Dis. 1979; 120:1379–1382. PMID: 517861.2. Baumann MH, Strange C, Heffner JE, Light R, Kirby TJ, Klein J, et al. Management of spontaneous pneumothorax: an American College of Chest Physicians Delphi consensus statement. Chest. 2001; 119:590–602. PMID: 11171742.3. Henry M, Arnold T, Harvey J. Pleural Diseases Group. Standards of Care Committee. British Thoracic Society. BTS guidelines for the management of spontaneous pneumothorax. Thorax. 2003; 58(Suppl 2):ii39–ii52. PMID: 12728149.
Article4. Dernevik L, Roberts D, Hamraz B, Nordstrand-Myntevik M. Management of pneumothorax with a mini-drain in ambulatory and hospitalized patients. Scand Cardiovasc J. 2003; 37:172–176. PMID: 12881149.
Article5. Röggla M, Wagner A, Brunner C, Röggla G. The management of pneumothorax with the thoracic vent versus conventional intercostal tube drainage. Wien Klin Wochenschr. 1996; 108:330–333. PMID: 8767986.6. Tsuchiya T, Sano A. Outpatient treatment of pneumothorax with a thoracic vent: economic benefit. Respiration. 2015; 90:33–39. PMID: 25997413.
Article7. Samelson SL, Goldberg EM, Ferguson MK. The thoracic vent. Clinical experience with a new device for treating simple pneumothorax. Chest. 1991; 100:880–882. PMID: 1889296.8. Collins CD, Lopez A, Mathie A, Wood V, Jackson JE, Roddie ME. Quantification of pneumothorax size on chest radiographs using interpleural distances: regression analysis based on volume measurements from helical CT. AJR Am J Roentgenol. 1995; 165:1127–1130. PMID: 7572489.
Article9. Heimlich HJ. Valve drainage of the pleural cavity. Dis Chest. 1968; 53:282–287. PMID: 5640897.
Article10. Mariani PJ, Sharma S. Iatrogenic tension pneumothorax complicating outpatient Heimlich valve chest drainage. J Emerg Med. 1994; 12:477–479. PMID: 7963393.
Article11. Crocker HL, Ruffin RE. Patient-induced complications of a Heimlich flutter valve. Chest. 1998; 113:838–839. PMID: 9515868.
Article12. Kobayashi Y. [Two cases of pneumothorax using the thoracic vent (TV) on an outpatient basis]. Nihon Kokyuki Gakkai Zasshi. 2001; 39:256–259. PMID: 11481824.13. Sano A, Tsuchiya T, Nagano M. Outpatient drainage therapy with a thoracic vent for traumatic pneumothorax due to bull attack. Korean J Thorac Cardiovasc Surg. 2014; 47:563–565. PMID: 25551083.
Article14. Sato N, Abe K, Ishibashi N, Imai T. [Effectiveness of portable thoracic drainage kit for outpatient treatment of spontaneous pneumothorax]. Kyobu Geka. 2016; 69:418–422. PMID: 27246123.15. Yotsumoto T, Sano A, Sato Y. [Spontaneous pneumothorax during pregnancy successfully managed with a thoracic vent before surgical therapy; report of a case]. Kyobu Geka. 2015; 68:1031–1033. PMID: 26555922.16. Martin T, Fontana G, Olak J, Ferguson M. Use of pleural catheter for the management of simple pneumothorax. Chest. 1996; 110:1169–1172. PMID: 8915215.17. Jones AE, Knoepp LF, Oxley DD. Bronchopleural fistula resulting from the use of a thoracic vent: a case report and review. Chest. 1998; 114:1781–1784. PMID: 9872222.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Outpatient Drainage Therapy with a Thoracic Vent for Traumatic Pneumothorax due to Bull Attack
- Outpatient Treatment for Pneumothorax Using a Portable Small-Bore Chest Tube: A Clinical Report
- Outpatient Chest Tube Management with Using a Panda Pneumothorax Set with a Heimlich Valve
- Iatrogenic Pneumothorax after Thoracic Paravertebral Block: A report of 2 cases
- A comparative study on physical properties of orthodontic stainless steel wires