CT Quantification of Lungs and Airways in Normal Korean Subjects
- Affiliations
-
- 1Department of Radiology, Chungnam National University Hospital, Chungnam National University School of Medicine, Daejeon 35015, Korea.
- 2Department of Radiology, Research Institute of Clinical Medicine of Chonbuk National University-Biomedical Research Institute of Chonbuk National University Hospital, Chonbuk National University Medical School, Institute of Medical Science, Jeonju 54907, Korea. gyjin@jbnu.ac.kr
- 3Department of Radiology, Research Institute of Clinical Medicine of Chonbuk National University-Biomedical Research Institute of Chonbuk National University Hospital, Jeonju 54907, Korea.
- KMID: 2427243
- DOI: http://doi.org/10.3348/kjr.2017.18.4.739
Abstract
OBJECTIVE
To measure and compare the quantitative parameters of the lungs and airways in Korean never-smokers and current or former smokers ("ever-smokers").
MATERIALS AND METHODS
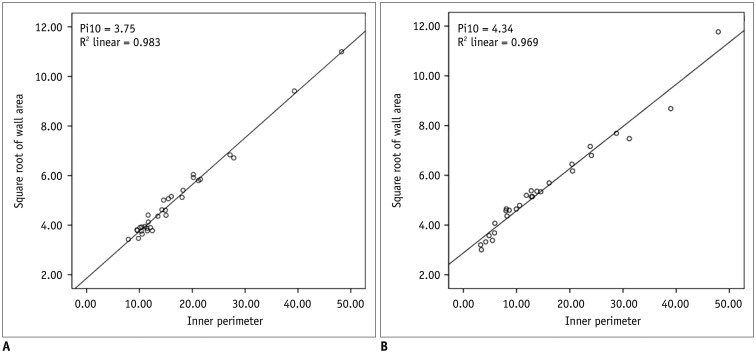
Never-smokers (n = 119) and ever-smokers (n = 45) who had normal spirometry and visually normal chest computed tomography (CT) results were retrospectively enrolled in this study. For quantitative CT analyses, the low attenuation area (LAA) of LAA(I-950), LAA(E-856), CT attenuation value at the 15th percentile, mean lung attenuation (MLA), bronchial wall thickness of inner perimeter of a 10 mm diameter airway (Pi10), total lung capacity (TLC(CT)), and functional residual capacity (FRC(CT)) were calculated based on inspiratory and expiratory CT images. To compare the results between groups according to age, sex, and smoking history, independent t test, one way ANOVA, correlation test, and simple and multiple regression analyses were performed.
RESULTS
The values of attenuation parameters and volume on inspiratory and expiratory quantitative computed tomography (QCT) were significantly different between males and females (p < 0.001). The MLA and the 15th percentile value on inspiratory QCT were significantly lower in the ever-smoker group than in the never-smoker group (p < 0.05). On expiratory QCT, all lung attenuation parameters were significantly different according to the age range (p < 0.05). Pi10 in ever-smokers was significantly correlated with forced expiratory volume in 1 second/forced vital capacity (r = −0.455, p = 0.003). In simple and multivariate regression analyses, TLC(CT), FRC(CT), and age showed significant associations with lung attenuation (p < 0.05), and only TLC(CT) was significantly associated with inspiratory Pi10.
CONCLUSION
In Korean subjects with normal spirometry and visually normal chest CT, there may be significant differences in QCT parameters according to sex, age, and smoking history.
Keyword
MeSH Terms
Figure
Cited by 5 articles
-
Impact of Model-Based Iterative Reconstruction on the Correlation between Computed Tomography Quantification of a Low Lung Attenuation Area and Airway Measurements and Pulmonary Function Test Results in Normal Subjects
Da Jung Kim, Cherry Kim, Chol Shin, Seung Ku Lee, Chang Sub Ko, Ki Yeol Lee
Korean J Radiol. 2018;19(6):1187-1195. doi: 10.3348/kjr.2018.19.6.1187.Age of Data in Contemporary Research Articles Published in Representative General Radiology Journals
Ji Hun Kang, Dong Hwan Kim, Seong Ho Park, Jung Hwan Baek
Korean J Radiol. 2018;19(6):1172-1178. doi: 10.3348/kjr.2018.19.6.1172.Comparison of Filtered Back Projection, Hybrid Iterative Reconstruction, Model-Based Iterative Reconstruction, and Virtual Monoenergetic Reconstruction Images at Both Low- and Standard-Dose Settings in Measurement of Emphysema Volume and Airway Wall Thickness: A CT Phantom Study
Cherry Kim, Ki Yeol Lee, Chol Shin, Eun-Young Kang, Yu-Whan Oh, Moin Ha, Chang Sub Ko, Jaehyung Cha
Korean J Radiol. 2018;19(4):809-817. doi: 10.3348/kjr.2018.19.4.809.Structural and Functional Features on Quantitative Chest Computed Tomography in the Korean Asian versus the White American Healthy Non-Smokers
Hyun Bin Cho, Kum Ju Chae, Gong Yong Jin, Jiwoong Choi, Ching-Long Lin, Eric A. Hoffman, Sally E. Wenzel, Mario Castro, Sean B. Fain, Nizar N. Jarjour, Mark L. Schiebler, R. Graham Barr, Nadia Hansel, Christopher B. Cooper, Eric C. Kleerup, MeiLan K. Han, Prescott G. Woodruff, Richard E. Kanner, Eugene R. Bleecker, Stephen P. Peters, Wendy C. Moore, Chang Hyun Lee, Sanghun Choi,
Korean J Radiol. 2019;20(7):1236-1245. doi: 10.3348/kjr.2019.0083.Prediction of Treatment Response in Patients with Chronic Obstructive Pulmonary Disease by Determination of Airway Dimensions with Baseline Computed Tomography
Hyo Jung Park, Sang Min Lee, Jooae Choe, Sang Min Lee, Namkug Kim, Jae Seung Lee, Yeon-Mok Oh, Joon Beom Seo
Korean J Radiol. 2019;20(2):304-312. doi: 10.3348/kjr.2018.0204.
Reference
-
1. Stockley RA, Mannino D, Barnes PJ. Burden and pathogenesis of chronic obstructive pulmonary disease. Proc Am Thorac Soc. 2009; 6:524–526. PMID: 19741261.
Article2. Roy K, Smith J, Kolsum U, Borrill Z, Vestbo J, Singh D. COPD phenotype description using principal components analysis. Respir Res. 2009; 10:41. PMID: 19480658.
Article3. Bergin C, Müller N, Nichols DM, Lillington G, Hogg JC, Mullen B, et al. The diagnosis of emphysema. A computed tomographic-pathologic correlation. Am Rev Respir Dis. 1986; 133:541–546. PMID: 3963623.4. Hackx M, Bankier AA, Gevenois PA. Chronic obstructive pulmonary disease: CT quantification of airways disease. Radiology. 2012; 265:34–48. PMID: 22993219.
Article5. Lynch DA, Al-Qaisi MA. Quantitative computed tomography in chronic obstructive pulmonary disease. J Thorac Imaging. 2013; 28:284–290. PMID: 23748651.
Article6. Lee YK, Oh YM, Lee JH, Kim EK, Lee JH, Kim N, et al. Quantitative assessment of emphysema, air trapping, and airway thickening on computed tomography. Lung. 2008; 186:157–165. PMID: 18351420.
Article7. Burrows B. An overview of obstructive lung diseases. Med Clin North Am. 1981; 65:455–471. PMID: 7242173.
Article8. Fletcher C, Peto R. The natural history of chronic airflow obstruction. Br Med J. 1977; 1:1645–1648. PMID: 871704.
Article9. Niewoehner DE, Kleinerman J, Rice DB. Pathologic changes in the peripheral airways of young cigarette smokers. N Engl J Med. 1974; 291:755–758. PMID: 4414996.
Article10. Zach JA, Newell JD Jr, Schroeder J, Murphy JR, Curran-Everett D, Hoffman EA, et al. Quantitative computed tomography of the lungs and airways in healthy nonsmoking adults. Invest Radiol. 2012; 47:596–602. PMID: 22836310.
Article11. Regan EA, Lynch DA, Curran-Everett D, Curtis JL, Austin JH, Grenier PA, et al. Clinical and radiologic disease in smokers with normal spirometry. JAMA Intern Med. 2015; 175:1539–1549. PMID: 26098755.
Article12. Gevenois PA, Scillia P, de Maertelaer V, Michils A, De Vuyst P, Yernault JC. The effects of age, sex, lung size, and hyperinflation on CT lung densitometry. AJR Am J Roentgenol. 1996; 167:1169–1173. PMID: 8911175.
Article13. Irion KL, Marchiori E, Hochhegger B, Porto Nda S, Moreira Jda S, Anselmi CE, et al. CT quantification of emphysema in young subjects with no recognizable chest disease. AJR Am J Roentgenol. 2009; 192:W90–W96. PMID: 19234245.
Article14. Regan EA, Hokanson JE, Murphy JR, Make B, Lynch DA, Beaty TH, et al. Genetic epidemiology of COPD (COPDGene) study design. COPD. 2010; 7:32–43. PMID: 20214461.
Article15. Grydeland TB, Thorsen E, Dirksen A, Jensen R, Coxson HO, Pillai SG, et al. Quantitative CT measures of emphysema and airway wall thickness are related to D(L)CO. Respir Med. 2011; 105:343–351. PMID: 21074394.
Article16. Gevenois PA, de Maertelaer V, De Vuyst P, Zanen J, Yernault JC. Comparison of computed density and macroscopic morphometry in pulmonary emphysema. Am J Respir Crit Care Med. 1995; 152:653–657. PMID: 7633722.
Article17. Tschirren J, Hoffman EA, McLennan G, Sonka M. Segmentation and quantitative analysis of intrathoracic airway trees from computed tomography images. Proc Am Thorac Soc. 2005; 2:484–487. PMID: 16352753.
Article18. Palágyi K, Tschirren J, Hoffman EA, Sonka M. Quantitative analysis of pulmonary airway tree structures. Comput Biol Med. 2006; 36:974–996. PMID: 16076463.
Article19. Zhang L, Hoffman EA, Reinhardt JM. Atlas-driven lung lobe segmentation in volumetric X-ray CT images. IEEE Trans Med Imaging. 2006; 25:1–16. PMID: 16398410.
Article20. Hoffman EA, Simon BA, McLennan G. State of the art. A structural and functional assessment of the lung via multidetector-row computed tomography: phenotyping chronic obstructive pulmonary disease. Proc Am Thorac Soc. 2006; 3:519–532. PMID: 16921136.
Article21. Standardization of spirometry, 1994 update. American Thoracic Society. Am J Respir Crit Care Med. 1995; 152:1107–1136. PMID: 7663792.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Impact of Model-Based Iterative Reconstruction on the Correlation between Computed Tomography Quantification of a Low Lung Attenuation Area and Airway Measurements and Pulmonary Function Test Results in Normal Subjects
- CT Findings of Central Airway Lesions Causing Airway Stenosis-Visualization and Quantification: A Pictorial Essay
- CT Quantification of Central Airway in Tracheobronchomalacia
- Objective in Vivo Quantification of Emphysema by Thin-Section CT: Correlation with Physiologic Findings
- Pulmonary Manifestations of Fat Embolism on Thin-section CT: A Case Report