Yonsei Med J.
2016 Nov;57(6):1361-1369. 10.3349/ymj.2016.57.6.1361.
Hypoalbuminemia, Low Base Excess Values, and Tachypnea Predict 28-Day Mortality in Severe Sepsis and Septic Shock Patients in the Emergency Department
- Affiliations
-
- 1Department of Emergency Medicine, Yonsei University College of Medicine, Seoul, Korea. pys905@yuhs.ac
- 2Institute for Disaster Relief and Medical Safety Net, Yonsei University College of Medicine, Seoul, Korea.
- 3Department of Biostatistics, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 2427153
- DOI: http://doi.org/10.3349/ymj.2016.57.6.1361
Abstract
- PURPOSE
The objective of this study was to develop a new nomogram that can predict 28-day mortality in severe sepsis and/or septic shock patients using a combination of several biomarkers that are inexpensive and readily available in most emergency departments, with and without scoring systems.
MATERIALS AND METHODS
We enrolled 561 patients who were admitted to an emergency department (ED) and received early goal-directed therapy for severe sepsis or septic shock. We collected demographic data, initial vital signs, and laboratory data sampled at the time of ED admission. Patients were randomly assigned to a training set or validation set. For the training set, we generated models using independent variables associated with 28-day mortality by multivariate analysis, and developed a new nomogram for the prediction of 28-day mortality. Thereafter, the diagnostic accuracy of the nomogram was tested using the validation set.
RESULTS
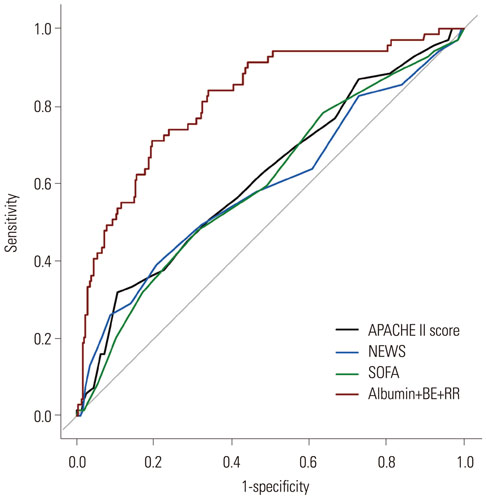
The prediction model that included albumin, base excess, and respiratory rate demonstrated the largest area under the receiver operating characteristic curve (AUC) value of 0.8173 [95% confidence interval (CI), 0.7605-0.8741]. The logistic analysis revealed that a conventional scoring system was not associated with 28-day mortality. In the validation set, the discrimination of a newly developed nomogram was also good, with an AUC value of 0.7537 (95% CI, 0.6563-0.8512).
CONCLUSION
Our new nomogram is valuable in predicting the 28-day mortality of patients with severe sepsis and/or septic shock in the emergency department. Moreover, our readily available nomogram is superior to conventional scoring systems in predicting mortality.
Keyword
MeSH Terms
Figure
Reference
-
1. Zimmerman JE, Kramer AA, Knaus WA. Changes in hospital mortality for United States intensive care unit admissions from 1988 to 2012. Crit Care. 2013; 17:R81.
Article2. Angus DC, van der Poll T. Severe sepsis and septic shock. N Engl J Med. 2013; 369:840–851.
Article3. Miller RR 3rd, Dong L, Nelson NC, Brown SM, Kuttler KG, Probst DR, et al. Multicenter implementation of a severe sepsis and septic shock treatment bundle. Am J Respir Crit Care Med. 2013; 188:77–82.
Article4. Kaukonen KM, Bailey M, Suzuki S, Pilcher D, Bellomo R. Mortality related to severe sepsis and septic shock among critically ill patients in Australia and New Zealand, 2000-2012. JAMA. 2014; 311:1308–1316.
Article5. Martin GS, Mannino DM, Eaton S, Moss M. The epidemiology of sepsis in the United States from 1979 through 2000. N Engl J Med. 2003; 348:1546–1554.
Article6. Wang HE, Shapiro NI, Angus DC, Yealy DM. National estimates of severe sepsis in United States emergency departments. Crit Care Med. 2007; 35:1928–1936.
Article7. Marshall JC, Reinhart K. International Sepsis Forum. Biomarkers of sepsis. Crit Care Med. 2009; 37:2290–2298.
Article8. Annane D, Bellissant E, Cavaillon JM. Septic shock. Lancet. 2005; 365:63–78.
Article9. Dupuy AM, Philippart F, Péan Y, Lasocki S, Charles PE, Chalumeau M, et al. Role of biomarkers in the management of antibiotic therapy: an expert panel review: I - currently available biomarkers for clinical use in acute infections. Ann Intensive Care. 2013; 3:22.
Article10. Jones AE, Saak K, Kline JA. Performance of the Mortality in Emergency Department Sepsis score for predicting hospital mortality among patients with severe sepsis and septic shock. Am J Emerg Med. 2008; 26:689–692.
Article11. Zhao Y, Li C, Jia Y. Evaluation of the Mortality in Emergency Department Sepsis score combined with procalcitonin in septic patients. Am J Emerg Med. 2013; 31:1086–1091.
Article12. Pierrakos C, Vincent JL. Sepsis biomarkers: a review. Crit Care. 2010; 14:R15.
Article13. O'Keefe SC, Marshall FF, Issa MM, Harmon MP, Petros JA. Thrombocytosis is associated with a significant increase in the cancer specific death rate after radical nephrectomy. J Urol. 2002; 168(4 Pt 1):1378–1380.14. Silvestre J, Póvoa P, Coelho L, Almeida E, Moreira P, Fernandes A, et al. Is C-reactive protein a good prognostic marker in septic patients? Intensive Care Med. 2009; 35:909–913.
Article15. Samraj RS, Zingarelli B, Wong HR. Role of biomarkers in sepsis care. Shock. 2013; 40:358–365.
Article16. Lee CC, Chen SY, Tsai CL, Wu SC, Chiang WC, Wang JL, et al. Prognostic value of mortality in emergency department sepsis score, procalcitonin, and C-reactive protein in patients with sepsis at the emergency department. Shock. 2008; 29:322–327.
Article17. Iasonos A, Schrag D, Raj GV, Panageas KS. How to build and interpret a nomogram for cancer prognosis. J Clin Oncol. 2008; 26:1364–1370.
Article18. Moshage HJ, Janssen JA, Franssen JH, Hafkenscheid JC, Yap SH. Study of the molecular mechanism of decreased liver synthesis of albumin in inflammation. J Clin Invest. 1987; 79:1635–1641.
Article19. Franch-Arcas G. The meaning of hypoalbuminaemia in clinical practice. Clin Nutr. 2001; 20:265–269.
Article20. Nicholson JP, Wolmarans MR, Park GR. The role of albumin in critical illness. Br J Anaesth. 2000; 85:599–610.
Article21. Emerson TE Jr. Unique features of albumin: a brief review. Crit Care Med. 1989; 17:690–694.22. Lee JH, Kim J, Kim K, Jo YH, Rhee J, Kim TY, et al. Albumin and C-reactive protein have prognostic significance in patients with community-acquired pneumonia. J Crit Care. 2011; 26:287–294.
Article23. Artero A, Zaragoza R, Camarena JJ, Sancho S, González R, Nogueira JM. Prognostic factors of mortality in patients with community-acquired bloodstream infection with severe sepsis and septic shock. J Crit Care. 2010; 25:276–281.
Article24. Vincent JL, Dubois MJ, Navickis RJ, Wilkes MM. Hypoalbuminemia in acute illness: is there a rationale for intervention? A meta-analysis of cohort studies and controlled trials. Ann Surg. 2003; 237:319–334.25. Siggaard-Andersen O, Fogh-Andersen N. Base excess or buffer base (strong ion difference) as measure of a non-respiratory acid-base disturbance. Acta Anaesthesiol Scand Suppl. 1995; 107:123–128.
Article26. Chaudry IH. Cellular mechanisms in shock and ischemia and their correction. Am J Physiol. 1983; 245:R117–R134.
Article27. Mecher C, Rackow EC, Astiz ME, Weil MH. Unaccounted for anion in metabolic acidosis during severe sepsis in humans. Crit Care Med. 1991; 19:705–711.
Article28. Noritomi DT, Soriano FG, Kellum JA, Cappi SB, Biselli PJ, Libório AB, et al. Metabolic acidosis in patients with severe sepsis and septic shock: a longitudinal quantitative study. Crit Care Med. 2009; 37:2733–2739.
Article29. Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: a severity of disease classification system. Crit Care Med. 1985; 13:818–829.30. Howell MD, Talmor D, Schuetz P, Hunziker S, Jones AE, Shapiro NI. Proof of principle: the predisposition, infection, response, organ failure sepsis staging system. Crit Care Med. 2011; 39:322–327.
Article31. Davis JW, Kaups KL, Parks SN. Base deficit is superior to pH in evaluating clearance of acidosis after traumatic shock. J Trauma. 1998; 44:114–118.
Article32. Sankoff JD, Goyal M, Gaieski DF, Deitch K, Davis CB, Sabel AL, et al. Validation of the Mortality in Emergency Department Sepsis (MEDS) score in patients with the systemic inflammatory response syndrome (SIRS). Crit Care Med. 2008; 36:421–426.
Article33. Nguyen HB, Van Ginkel C, Batech M, Banta J, Corbett SW. Comparison of predisposition, insult/infection, response, and organ dysfunction, acute physiology and chronic health evaluation II, and mortality in emergency department sepsis in patients meeting criteria for early goal-directed therapy and the severe sepsis resuscitation bundle. J Crit Care. 2012; 27:362–369.
Article34. Wilhelm J, Hettwer S, Hammer D, Schürmann M, Christoph A, Amoury M, et al. Outcome prediction using clinical scores and biomarkers in patients with presumed severe infection in the emergency department. Med Klin Intensivmed Notfmed. 2012; 107:558–563.
Article35. Rivers E, Nguyen B, Havstad S, Ressler J, Muzzin A, Knoblich B, et al. Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med. 2001; 345:1368–1377.
Article36. Thomas-Rueddel DO, Poidinger B, Weiss M, Bach F, Dey K, Häberle H, et al. Hyperlactatemia is an independent predictor of mortality and denotes distinct subtypes of severe sepsis and septic shock. J Crit Care. 2015; 30:439.e1–439.e6.
Article37. Sivayoham N, Rhodes A, Cecconi M. The MISSED score, a new scoring system to predict mortality in severe sepsis in the emergency department: a derivation and validation study. Eur J Emerg Med. 2014; 21:30–36.38. Nguyen HB, Lynch EL, Mou JA, Lyon K, Wittlake WA, Corbett SW. The utility of a quality improvement bundle in bridging the gap between research and standard care in the management of severe sepsis and septic shock in the emergency department. Acad Emerg Med. 2007; 14:1079–1086.
Article39. Jiang LB, Zhang M, Jiang SY, Ma YF. Early goal-directed resuscitation for patients with severe sepsis and septic shock: a meta-analysis and trial sequential analysis. Scand J Trauma Resusc Emerg Med. 2016; 24:23.
Article40. Mouncey PR, Osborn TM, Power GS, Harrison DA, Sadique MZ, Grieve RD, et al. Trial of early, goal-directed resuscitation for septic shock. N Engl J Med. 2015; 372:1301–1311.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Validation of Immature Granulocyte as a Predictor for the 28-Day Mortality in Patients with Severe Sepsis and Septic Shock
- Prognostic Importance of Hypoalbuminemia in Patients with Severe Sepsis and Septic Shock
- Sepsis, Severe Sepsis and Septic Shock in the Elderly
- Mortality among adult patients with sepsis and septic shock in Korea: a systematic review and meta-analysis
- Recent Evidences of Sepsis Treatment