Investig Clin Urol.
2016 Sep;57(5):357-363. 10.4111/icu.2016.57.5.357.
Phosphodiesterase type 5 inhibitor administered immediately after radical prostatectomy temporarily increases the need for incontinence pads, but improves final continence status
- Affiliations
-
- 1Department of Urology, Tohoku University Graduate School of Medicine, Sendai, Japan. kaiho@uro.med.tohoku.ac.jp
- KMID: 2427015
- DOI: http://doi.org/10.4111/icu.2016.57.5.357
Abstract
- PURPOSE
To evaluate the effects of phosphodiesterase type 5 inhibitor (PDE5i) on urinary continence recovery after bilateral nerve-sparing radical prostatectomy (BNSRP).
MATERIALS AND METHODS
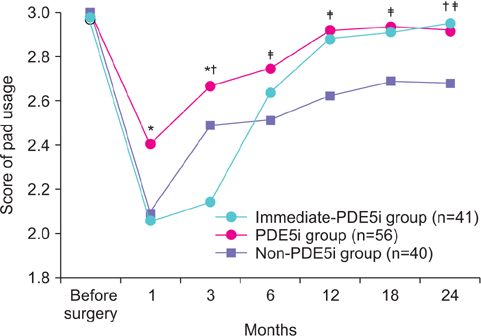
Between 2002 and 2012, 137 of 154 consecutive patients who underwent BNSRP in our institution retrospectively divided into 3 groups that included patients taking PDE5i immediately after surgery (immediate PDE5i group, n=41), patients starting PDE5i at an outpatient clinic after discharge (PDE5i group, n=56), and patients taking no medication (non-PDE5i group, n=40). Using self-administered questionnaires, the proportion of patients who did not require incontinence pads (pad-free patients) was calculated preoperatively and at 1, 3, 6, 12, 18, and 24 months after BNSRP. Severity of incontinence was determined based on the pad numbers and then compared among the 3 groups.
RESULTS
Proportions of pad-free patients and severity of incontinence initially deteriorated in all of the groups to the lowest values soon after undergoing BNSRP, with gradual improvement noted thereafter. The deterioration was most prominent in the immediate PDE5i group. As compared to the non-PDE5i group, both the PDE5i and immediate PDE5i groups exhibited a better final continence status.
CONCLUSIONS
PDE5i improves final continence status. However, administration of PDE5i immediately after surgery causes a distinct temporary deterioration in urinary incontinence.
Keyword
MeSH Terms
-
Aged
Drug Administration Schedule
Drug Evaluation/methods
Follow-Up Studies
Humans
Incontinence Pads/*utilization
Male
Middle Aged
Phosphodiesterase 5 Inhibitors/*administration & dosage/adverse effects/therapeutic use
Postoperative Care/methods
Prostatectomy/*adverse effects/methods
Recovery of Function/drug effects
Retrospective Studies
Severity of Illness Index
Urinary Incontinence/etiology/physiopathology/*prevention & control
Urination/drug effects
Phosphodiesterase 5 Inhibitors
Figure
Reference
-
1. Kaiho Y, Mitsuzuka K, Yamada S, Saito H, Adachi H, Yamashita S, et al. Urinary straining contributes to inguinal hernia after radical retropubic prostatectomy. Int J Urol. 2016; 23:478–483.2. Kaiho Y, Yamashita S, Arai Y. Optimization of sexual function outcome after radical prostatectomy using phosphodiesterase type 5 inhibitors. Int J Urol. 2013; 20:285–289.3. Namiki S, Kaiho Y, Mitsuzuka K, Saito H, Yamada S, Nakagawa H, et al. Long-term quality of life after radical prostatectomy: 8-year longitudinal study in Japan. Int J Urol. 2014; 21:1220–1226.4. Litwin MS, Lubeck DP, Henning JM, Carroll PR. Differences in urologist and patient assessments of health related quality of life in men with prostate cancer: results of the CaPSURE database. J Urol. 1998; 159:1988–1992.5. Ferrini MG, Davila HH, Kovanecz I, Sanchez SP, Gonzalez-Cadavid NF, Rajfer J. Vardenafil prevents fibrosis and loss of corporal smooth muscle that occurs after bilateral cavernosal nerve resection in the rat. Urology. 2006; 68:429–435.6. Mulhall JP, Muller A, Donohue JF, Mullerad M, Kobylarz K, Paduch DA, et al. The functional and structural consequences of cavernous nerve injury are ameliorated by sildenafil citrate. J Sex Med. 2008; 5:1126–1136.7. Patel HR, Ilo D, Shah N, Cuzin B, Chadwick D, Andrianne R, et al. Effects of tadalafil treatment after bilateral nerve-sparing radical prostatectomy: quality of life, psychosocial outcomes, and treatment satisfaction results from a randomized, placebo-controlled phase IV study. BMC Urol. 2015; 15:31.8. Canat L, Guner B, Gürbuz C, Atıs G, Caskurlu T. Effects of three-times-per-week versus on-demand tadalafil treatment on erectile function and continence recovery following bilateral nerve sparing radical prostatectomy: results of a prospective, randomized, and single-center study. Kaohsiung J Med Sci. 2015; 31:90–95.9. Lin G, Huang YC, Wang G, Lue TF, Lin CS. Prominent expression of phosphodiesterase 5 in striated muscle of the rat urethra and levator ani. J Urol. 2010; 184:769–774.10. Werkstrom V, Svensson A, Andersson KE, Hedlund P. Phosphodiesterase 5 in the female pig and human urethra: morphological and functional aspects. BJU Int. 2006; 98:414–423.11. Gacci M, Ierardi A, Rose AD, Tazzioli S, Scapaticci E, Filippi S, et al. Vardenafil can improve continence recovery after bilateral nerve sparing prostatectomy: results of a randomized, double blind, placebo-controlled pilot study. J Sex Med. 2010; 7(1 Pt 1):234–243.12. Gandaglia G, Albersen M, Suardi N, Gallina A, Abdollah F, Castiglione F, et al. Postoperative phosphodiesterase type 5 inhibitor administration increases the rate of urinary continence recovery after bilateral nerve-sparing radical prostatectomy. Int J Urol. 2013; 20:413–419.13. Izumi H, Kaiho Y, Miyazato M, Kawamorita N, Nakagawa H, Arai Y. Effects of phosphodiesterase type 5 inhibitor, tadalafil, on continence reflex in rats. Int Urogynecol J. 2014; 25:1721–1727.14. Soh J, Kaiho Y, Kikuchi E, Oya M, Yoshioka K, Nakagami Y, et al. Characteristics and management of erectile dysfunction after various treatments for prostate cancer. Int J Urol. 2010; 17:689–697.15. Litwin MS, Hays RD, Fink A, Ganz PA, Leake B, Brook RH. The UCLA Prostate Cancer Index: development, reliability, and validity of a health-related quality of life measure. Med Care. 1998; 36:1002–1012.16. Wei JT, Dunn RL, Litwin MS, Sandler HM, Sanda MG. Development and validation of the expanded prostate cancer index composite (EPIC) for comprehensive assessment of health-related quality of life in men with prostate cancer. Urology. 2000; 56:899–905.17. Fukuhara S, Ware JE Jr, Kosinski M, Wada S, Gandek B. Psychometric and clinical tests of validity of the Japanese SF-36 Health Survey. J Clin Epidemiol. 1998; 51:1045–1053.18. Kakehi Y, Kamoto T, Ogawa O, Arai Y, Litwin MS, Suzukamo Y, et al. Development of Japanese version of the UCLA Prostate Cancer Index: a pilot validation study. Int J Clin Oncol. 2002; 7:306–311.19. Mulhall JP, Parker M, Waters BW, Flanigan R. The timing of penile rehabilitation after bilateral nerve-sparing radical prostatectomy affects the recovery of erectile function. BJU Int. 2010; 105:37–41.20. Salonia A, Castagna G, Capogrosso P, Castiglione F, Briganti A, Montorsi F. Prevention and management of post prostatectomy erectile dysfunction. Transl Androl Urol. 2015; 4:421–437.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effect of Posterior Urethral Reconstruction (PUR) in Early Recovery of Urinary Continence after Robotic-Assisted Radical Prostatectomy
- Discrepancies in Perception of Urinary Incontinence between Patient and Physician after Robotic Radical Prostatectomy
- Impact of a Retrotrigonal Layer Backup Stitch on Post-Prostatectomy Incontinence
- Association between cystographic anastomotic urinary leakage following retropubic radical prostatectomy and early urinary incontinence
- Effect of Extracorporeal Magnetic Innervation (ExMI) Pelvic Floor Therapy on Urinary Incontinence after Radical Prostatectomy