J Korean Neuropsychiatr Assoc.
2018 Nov;57(4):276-286. 10.4306/jknpa.2018.57.4.276.
Is the Circadian Rhythm Dysregulation a Core Pathogenetic Mechanism of Bipolar Disorder?
- Affiliations
-
- 1Department of Psychiatry and Biomedical Sciences, Korea University College of Medicine, Korea University Chronobiology Institute, Seoul, Korea. leehjeong@korea.ac.kr
- KMID: 2426856
- DOI: http://doi.org/10.4306/jknpa.2018.57.4.276
Abstract
- Circadian rhythm is a periodic and continuous change in physiological, behavioral, and mental characteristics that occurs in most organisms on the Earth, because the Earth rotates in a 24-hour cycle. The circadian system regulates daily rhythms of physiology and behavior, such as the sleep/wake cycle, body temperature, hormonal secretion, and mood. The influence of circadian rhythm is very powerful, but limited research has addressed its effects. However, many recent studies have shown that circadian dysregulation may play an important role in the pathogenesis of bipolar disorder. This review study examined current and noteworthy studies, including the authors' own works, and proposes a possible clinical application of bipolar disorder based on evidence that circadian rhythm dysregulation in bipolar disorder may be a key pathogenetic mechanism.
Figure
Reference
-
1. Kraepelin E. Über Sprachstörungen im Traume. Leizpig: Engelmann;1906.2. Harvey AG. Sleep and circadian rhythms in bipolar disorder: seeking synchrony, harmony, and regulation. Am J Psychiatry. 2008; 165:820–829.
Article3. Ng TH, Chung KF, Ho FY, Yeung WF, Yung KP, Lam TH. Sleepwake disturbance in interepisode bipolar disorder and high-risk individuals: a systematic review and meta-analysis. Sleep Med Rev. 2015; 20:46–58.
Article4. Nobelprize.org [homepage on the Internet]. The Nobel Prize in Physiology or Medicine;2017. cited 2018 Oct 20. Available from: https://www.nobelprize.org/prizes/medicine/2017/summary.5. Linkowski P. Neuroendocrine profiles in mood disorders. Int J Neuropsychopharmacol. 2003; 6:191–197.
Article6. Murray G, Harvey A. Circadian rhythms and sleep in bipolar disorder. Bipolar Disord. 2010; 12:459–472.
Article7. Abreu T, Bragança M. The bipolarity of light and dark: a review on bipolar disorder and circadian cycles. J Affect Disord. 2015; 185:219–229.
Article8. Melo MC, Garcia RF, Linhares Neto VB, Sá MB, de Mesquita LM, de Araújo CF, et al. Sleep and circadian alterations in people at risk for bipolar disorder: a systematic review. J Psychiatr Res. 2016; 83:211–219.
Article9. Melo MC, Abreu RL, Linhares Neto VB, de Bruin PF, de Bruin VM. Chronotype and circadian rhythm in bipolar disorder: a systematic review. Sleep Med Rev. 2017; 34:46–58.
Article10. Alloy LB, Ng TH, Titone MK, Boland EM. Circadian rhythm dysregulation in bipolar spectrum disorders. Curr Psychiatry Rep. 2017; 19:21.
Article11. Paranjpe DA, Sharma VK. Evolution of temporal order in living organisms. J Circadian Rhythms. 2005; 3:7.
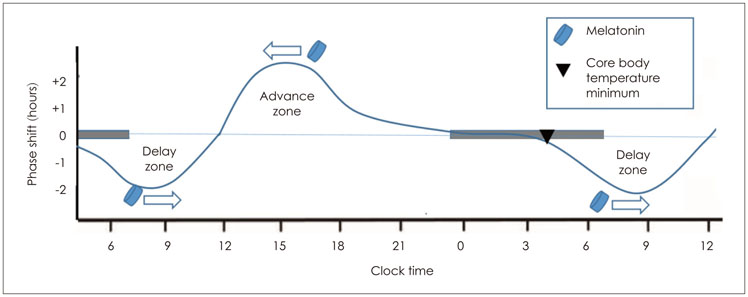
Article12. Wever RA. Characteristics of circadian rhythms in human functions. J Neural Transm Suppl. 1986; 21:323–373.13. Moore RY, Eichler VB. Loss of a circadian adrenal corticosterone rhythm following suprachiasmatic lesions in the rat. Brain Res. 1972; 42:201–206.
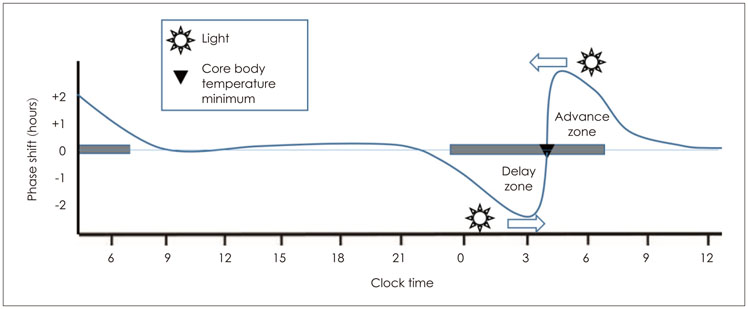
Article14. Ralph MR, Foster RG, Davis FC, Menaker M. Transplanted suprachiasmatic nucleus determines circadian period. Science. 1990; 247:975–978.
Article15. Silver R, LeSauter J, Tresco PA, Lehman MN. A diffusible coupling signal from the transplanted suprachiasmatic nucleus controlling circadian locomotor rhythms. Nature. 1996; 382:810–813.
Article16. Son GH, Chung S, Kim K. The adrenal peripheral clock: glucocorticoid and the circadian timing system. Front Neuroendocrinol. 2011; 32:451–465.
Article17. Mansour HA, Monk TH, Nimgaonkar VL. Circadian genes and bipolar disorder. Ann Med. 2005; 37:196–205.
Article18. Welsh DK, Logothetis DE, Meister M, Reppert SM. Individual neurons dissociated from rat suprachiasmatic nucleus express independently phased circadian firing rhythms. Neuron. 1995; 14:697–706.
Article19. Czeisler CA, Klerman EB. Circadian and sleep-dependent regulation of hormone release in humans. Recent Prog Horm Res. 1999; 54:97–130. discussion 130-132.20. Scheer FA, Hu K, Evoniuk H, Kelly EE, Malhotra A, Hilton MF, et al. Impact of the human circadian system, exercise, and their interaction on cardiovascular function. Proc Natl Acad Sci U S A. 2010; 107:20541–20546.
Article21. Balsalobre A, Brown SA, Marcacci L, Tronche F, Kellendonk C, Reichardt HM, et al. Resetting of circadian time in peripheral tissues by glucocorticoid signaling. Science. 2000; 289:2344–2347.
Article22. Burgess HJ, Revell VL, Molina TA, Eastman CI. Human phase response curves to three days of daily melatonin: 0.5 mg versus 3.0 mg. J Clin Endocrinol Metab. 2010; 95:3325–3331.
Article23. Khalsa SBS, Jewett ME, Cajochen C, Czeisler CA. A phase response curve to single bright light pulses in human subjects. J Physiol. 2003; 549:945–952.
Article24. Hudson JI, Lipinski JF, Frankenburg FR, Grochocinski VJ, Kupfer DJ. Electroencephalographic sleep in mania. Arch Gen Psychiatry. 1988; 45:267–273.
Article25. Hudson JI, Lipinski JF, Keck PE Jr, Aizley HG, Lukas SE, Rothschild AJ, et al. Polysomnographic characteristics of young manic patients. Comparison with unipolar depressed patients and normal control subjects. Arch Gen Psychiatry. 1992; 49:378–383.
Article26. Gershon A, Thompson WK, Eidelman P, McGlinchey EL, Kaplan KA, Harvey AG. Restless pillow, ruffled mind: sleep and affect coupling in interepisode bipolar disorder. J Abnorm Psychol. 2012; 121:863–873.
Article27. Harvey AG, Schmidt DA, Scarnà A, Semler CN, Goodwin GM. Sleep-related functioning in euthymic patients with bipolar disorder, patients with insomnia, and subjects without sleep problems. Am J Psychiatry. 2005; 162:50–57.
Article28. Rocha PM, Neves FS, Corrêa H. Significant sleep disturbances in euthymic bipolar patients. Compr Psychiatry. 2013; 54:1003–1008.
Article29. Steinan MK, Morken G, Lagerberg TV, Melle I, Andreassen OA, Vaaler AE, et al. Delayed sleep phase: an important circadian subtype of sleep disturbance in bipolar disorders. J Affect Disord. 2016; 191:156–163.
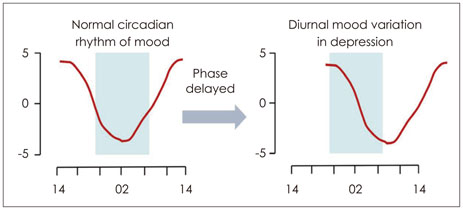
Article30. Lee HJ, Son GH, Geum D. Circadian rhythm hypotheses of mixed features, antidepressant treatment resistance, and manic switching in bipolar disorder. Psychiatry Investig. 2013; 10:225–232.
Article31. Takaesu Y. Circadian rhythm in bipolar disorder: a review of the literature. Psychiatry Clin Neurosci. 2018; 72:673–682.
Article32. Lee HJ, Rex KM, Nievergelt CM, Kelsoe JR, Kripke DF. Delayed sleep phase syndrome is related to seasonal affective disorder. J Affect Disord. 2011; 133:573–579.
Article33. Boudebesse C, Lajnef M, Geoffroy PA, Bellivier F, Nieto I, Gard S, et al. Chronotypes of bipolar patients in remission: validation of the French version of the circadian type inventory in the FACE-BD sample. Chronobiol Int. 2013; 30:1042–1049.
Article34. Ahn YM, Chang J, Joo YH, Kim SC, Lee KY, Kim YS. Chronotype distribution in bipolar I disorder and schizophrenia in a Korean sample. Bipolar Disord. 2008; 10:271–275.
Article35. Baek JH, Kim JS, Kim MJ, Ryu S, Lee K, Ha K, et al. Lifetime characteristics of evening-preference and irregular bed-rise time are associated with lifetime seasonal variation of mood and behavior: comparison between individuals with bipolar disorder and healthy controls. Behav Sleep Med. 2016; 14:155–168.
Article36. Wood J, Birmaher B, Axelson D, Ehmann M, Kalas C, Monk K, et al. Replicable differences in preferred circadian phase between bipolar disorder patients and control individuals. Psychiatry Res. 2009; 166:201–209.
Article37. Giglio LM, Magalhães PV, Andersen ML, Walz JC, Jakobson L, Kapczinski F. Circadian preference in bipolar disorder. Sleep Breath. 2010; 14:153–155.
Article38. Seleem MA, Merranko JA, Goldstein TR, Goldstein BI, Axelson DA, Brent DA, et al. The longitudinal course of sleep timing and circadian preferences in adults with bipolar disorder. Bipolar Disord. 2015; 17:392–402.
Article39. Claustrat B, Brun J, Chazot G. The basic physiology and pathophysiology of melatonin. Sleep Med Rev. 2005; 9:11–24.
Article40. Nováková M, Praško J, Látalová K, Sládek M, Sumová A. The circadian system of patients with bipolar disorder differs in episodes of mania and depression. Bipolar Disord. 2015; 17:303–314.
Article41. Lewy AJ. Circadian misalignment in mood disturbances. Curr Psychiatry Rep. 2009; 11:459–465.
Article42. Nurnberger JI Jr, Adkins S, Lahiri DK, Mayeda A, Hu K, Lewy A, et al. Melatonin suppression by light in euthymic bipolar and unipolar patients. Arch Gen Psychiatry. 2000; 57:572–579.
Article43. Dallaspezia S, Benedetti F. Melatonin, circadian rhythms, and the clock genes in bipolar disorder. Curr Psychiatry Rep. 2009; 11:488–493.
Article44. Robillard R, Naismith SL, Rogers NL, Scott EM, Ip TK, Hermens DF, et al. Sleep-wake cycle and melatonin rhythms in adolescents and young adults with mood disorders: comparison of unipolar and bipolar phenotypes. Eur Psychiatry. 2013; 28:412–416.
Article45. Kennedy SH, Kutcher SP, Ralevski E, Brown GM. Nocturnal melatonin and 24-hour 6-sulphatoxymelatonin levels in various phases of bipolar affective disorder. Psychiatry Res. 1996; 63:219–222.
Article46. Moon JH, Cho CH, Son GH, Geum D, Chung S, Kim H, et al. Advanced circadian phase in mania and delayed circadian phase in mixed mania and depression returned to normal after treatment of bipolar disorder. EBioMedicine. 2016; 11:285–295.
Article47. Benedetti F, Serretti A, Colombo C, Barbini B, Lorenzi C, Campori E, et al. Influence of CLOCK gene polymorphism on circadian mood fluctuation and illness recurrence in bipolar depression. Am J Med Genet B Neuropsychiatr Genet. 2003; 123B:23–26.48. Nievergelt CM, Kripke DF, Barrett TB, Burg E, Remick RA, Sadovnick AD, et al. Suggestive evidence for association of the circadian genes PERIOD3 and ARNTL with bipolar disorder. Am J Med Genet B Neuropsychiatr Genet. 2006; 141B:234–241.49. Mansour HA, Wood J, Logue T, Chowdari KV, Dayal M, Kupfer DJ, et al. Association study of eight circadian genes with bipolar I disorder, schizoaffective disorder and schizophrenia. Genes Brain Behav. 2006; 5:150–157.
Article50. Nievergelt CM, Kripke DF, Remick RA, Sadovnick AD, McElroy SL, Keck PE Jr, et al. Examination of the clock gene cryptochrome 1 in bipolar disorder: mutational analysis and absence of evidence for linkage or association. Psychiatr Genet. 2005; 15:45–52.
Article51. Benedetti F, Bernasconi A, Lorenzi C, Pontiggia A, Serretti A, Colombo C, et al. A single nucleotide polymorphism in glycogen synthase kinase 3-beta promoter gene influences onset of illness in patients affected by bipolar disorder. Neurosci Lett. 2004; 355:37–40.
Article52. Benedetti F, Serretti A, Colombo C, Lorenzi C, Tubazio V, Smeraldi E. A glycogen synthase kinase 3-beta promoter gene single nucleotide polymorphism is associated with age at onset and response to total sleep deprivation in bipolar depression. Neurosci Lett. 2004; 368:123–126.
Article53. Kaladchibachi SA, Doble B, Anthopoulos N, Woodgett JR, Manoukian AS. Glycogen synthase kinase 3, circadian rhythms, and bipolar disorder: a molecular link in the therapeutic action of lithium. J Circadian Rhythms. 2007; 5:3.
Article54. O'Brien WT, Klein PS. Validating GSK3 as an in vivo target of lithium action. Biochem Soc Trans. 2009; 37:1133–1138.55. Lee KY, Ahn YM, Joo EJ, Jeong SH, Chang JS, Kim SC, et al. No association of two common SNPs at position -1727 A/T, -50 C/T of GSK-3 beta polymorphisms with schizophrenia and bipolar disorder of Korean population. Neurosci Lett. 2006; 395:175–178.
Article56. Baum AE, Akula N, Cabanero M, Cardona I, Corona W, Klemens B, et al. A genomewide association study implicates diacylglycerol kinase eta (DGKH) and several other genes in the etiology of bipolar disorder. Mol Psychiatry. 2008; 13:197–207.
Article57. Ferreira MA, O'Donovan MC, Meng YA, Jones IR, Ruderfer DM, Jones L, et al. Collaborative genome-wide association analysis supports a role for ANK3 and CACNA1C in bipolar disorder. Nat Genet. 2008; 40:1056–1058.
Article58. Stahl E, Forstner A, McQuillin A, Ripke S, Ophoff R, Scott L, et al. Genomewide association study identifies 30 loci associated with bipolar disorder. bioRxiv. 2017; 173062.59. Ikeda M, Takahashi A, Kamatani Y, Okahisa Y, Kunugi H, Mori N, et al. A genome-wide association study identifies two novel susceptibility loci and trans population polygenicity associated with bipolar disorder. Mol Psychiatry. 2018; 23:639–647.
Article60. Schizophrenia Working. Biological insights from 108 schizophrenia-associated genetic loci. Nature. 2014; 511:421–427.
Article61. Visscher PM, Wray NR, Zhang Q, Sklar P, McCarthy MI, Brown MA, et al. 10 years of GWAS discovery: biology, function, and translation. Am J Hum Genet. 2017; 101:5–22.
Article62. Sekar A, Bialas AR, de Rivera H, Davis A, Hammond TR, Kamitaki N, et al. Schizophrenia risk from complex variation of complement component 4. Nature. 2016; 530:177–183.
Article63. Yamanaka Y, Hashimoto S, Masubuchi S, Natsubori A, Nishide SY, Honma S, et al. Differential regulation of circadian melatonin rhythm and sleepwake cycle by bright lights and nonphotic time cues in humans. Am J Physiol Regul Integr Comp Physiol. 2014; 307:R546–R557.
Article64. Ehlers CL, Frank E, Kupfer DJ. Social zeitgebers and biological rhythms. A unified approach to understanding the etiology of depression. Arch Gen Psychiatry. 1988; 45:948–952.65. Jones SH, Hare DJ, Evershed K. Actigraphic assessment of circadian activity and sleep patterns in bipolar disorder. Bipolar Disord. 2005; 7:176–186.
Article66. Bauer M, Grof P, Rasgon N, Bschor T, Glenn T, Whybrow PC. Temporal relation between sleep and mood in patients with bipolar disorder. Bipolar Disord. 2006; 8:160–167.
Article67. Kim SH, Park HG, Jeong SH, Kang UG, Ahn YM, Kim YS. Electroconvulsive seizure alters the expression and daily oscillation of circadian genes in the rat frontal cortex. Psychiatry Investig. 2018; 15:717–726.
Article68. Duncan WC Jr, Slonena E, Hejazi NS, Brutsche N, Yu KC, Park L, et al. Motor-activity markers of circadian timekeeping are related to ketamine's rapid antidepressant properties. Biol Psychiatry. 2017; 82:361–369.
Article69. Orozco-Solis R, Montellier E, Aguilar-Arnal L, Sato S, Vawter MP, Bunney BG, et al. A circadian genomic signature common to ketamine and sleep deprivation in the anterior cingulate cortex. Biol Psychiatry. 2017; 82:351–360.
Article70. Cho CH, Lee HJ. Why do mania and suicide occur most often in the spring? Psychiatry Investig. 2018; 15:232–234.
Article71. Jon DI, Yoon BH, Jung HY, Ha KS, Shin YC, Bahk WM. A validation study of the Korean version mood disorder questionnaire (K-MDQ). J Korean Neuropsychiatr Assoc. 2005; 44:583–590.72. Cho CH, Moon JH, Yoon HK, Kang SG, Geum D, Son GH, et al. Molecular circadian rhythm shift due to bright light exposure before bedtime is related to subthreshold bipolarity. Sci Rep. 2016; 6:31846.
Article73. Robillard R, Naismith SL, Rogers NL, Ip TK, Hermens DF, Scott EM, et al. Delayed sleep phase in young people with unipolar or bipolar affective disorders. J Affect Disord. 2013; 145:260–263.
Article74. Inoue T, Inagaki Y, Kimura T, Shirakawa O. Prevalence and predictors of bipolar disorders in patients with a major depressive episode: the Japanese epidemiological trial with latest measure of bipolar disorder (JET-LMBP). J Affect Disord. 2015; 174:535–541.
Article75. Cho CH, Jung SY, Kapczinski F, Rosa AR, Lee HJ. Validation of the Korean version of the biological rhythms interview of assessment in neuropsychiatry. Psychiatry Investig In press;2018.76. Duarte Faria A, Cardoso Tde A, Campos Mondin T, Souza LD, Magalhaes PV, Patrick Zeni C, et al. Biological rhythms in bipolar and depressive disorders: a community study with drug-naïve young adults. J Affect Disord. 2015; 186:145–148.
Article77. Takaesu Y, Inoue Y, Ono K, Murakoshi A, Futenma K, Komada Y, et al. Circadian rhythm sleep-wake disorders as predictors for bipolar disorder in patients with remitted mood disorders. J Affect Disord. 2017; 220:57–61.
Article78. Alloy LB, Boland EM, Ng TH, Whitehouse WG, Abramson LY. Low social rhythm regularity predicts first onset of bipolar spectrum disorders among at-risk individuals with reward hypersensitivity. J Abnorm Psychol. 2015; 124:944–952.
Article79. Shen GH, Alloy LB, Abramson LY, Sylvia LG. Social rhythm regularity and the onset of affective episodes in bipolar spectrum individuals. Bipolar Disord. 2008; 10:520–529.
Article80. Ng TH, Chung KF, Ng TK, Lee CT, Chan MS. Correlates and prognostic relevance of sleep irregularity in interepisode bipolar disorder. Compr Psychiatry. 2016; 69:155–162.
Article81. Vadnie CA, McClung CA. Circadian rhythm disturbances in mood disorders: insights into the role of the suprachiasmatic nucleus. Neural Plast. 2017; 2017:1504507.
Article82. Kripke DF, Mullaney DJ, Atkinson M, Wolf S. Circadian rhythm disorders in manic-depressives. Biol Psychiatry. 1978; 13:335–351.83. Hirota T, Lewis WG, Liu AC, Lee JW, Schultz PG, Kay SA. A chemical biology approach reveals period shortening of the mammalian circadian clock by specific inhibition of GSK-3beta. Proc Natl Acad Sci U S A. 2008; 105:20746–20751.
Article84. Bersani G, Garavini A. Melatonin add-on in manic patients with treatment resistant insomnia. Prog Neuropsychopharmacol Biol Psychiatry. 2000; 24:185–191.
Article85. Leproult R, Van Onderbergen A, L'hermite-Balériaux M, Van Cauter E, Copinschi G. Phase-shifts of 24-h rhythms of hormonal release and body temperature following early evening administration of the melatonin agonist agomelatine in healthy older men. Clin Endocrinol (Oxf). 2005; 63:298–304.
Article86. Fornaro M, McCarthy MJ, De Berardis D, De Pasquale C, Tabaton M, Martino M, et al. Adjunctive agomelatine therapy in the treatment of acute bipolar II depression: a preliminary open label study. Neuropsychiatr Dis Treat. 2013; 9:243–251.
Article87. Calabrese JR, Guelfi JD, Perdrizet-Chevallier C;. Agomelatine adjunctive therapy for acute bipolar depression: preliminary open data. Bipolar Disord. 2007; 9:628–635.
Article88. Yatham LN, Vieta E, Goodwin GM, Bourin M, de Bodinat C, Laredo J, et al. Agomelatine or placebo as adjunctive therapy to a mood stabiliser in bipolar I depression: randomised double-blind placebo controlled trial. Br J Psychiatry. 2016; 208:78–86.
Article89. Norris ER, Burke K, Correll JR, Zemanek KJ, Lerman J, Primelo RA, et al. A double-blind, randomized, placebo-controlled trial of adjunctive ramelteon for the treatment of insomnia and mood stability in patients with euthymic bipolar disorder. J Affect Disord. 2013; 144:141–147.
Article90. Terman M, Terman JS. Light therapy for seasonal and nonseasonal depression: efficacy, protocol, safety, and side effects. CNS Spectr. 2005; 10:647–663. quiz 672.
Article91. Benedetti F, Riccaboni R, Locatelli C, Poletti S, Dallaspezia S, Colombo C. Rapid treatment response of suicidal symptoms to lithium, sleep deprivation, and light therapy (chronotherapeutics) in drug-resistant bipolar depression. J Clin Psychiatry. 2014; 75:133–140.
Article92. Sit DK, McGowan J, Wiltrout C, Diler RS, Dills JJ, Luther J, et al. Adjunctive bright light therapy for bipolar depression: a randomized double-blind placebo-controlled trial. Am J Psychiatry. 2018; 175:131–139.
Article93. Wehr TA, Turner EH, Shimada JM, Lowe CH, Barker C, Leibenluft E. Treatment of rapidly cycling bipolar patient by using extended bed rest and darkness to stabilize the timing and duration of sleep. Biol Psychiatry. 1998; 43:822–828.
Article94. Wirz-Justice A, Quinto C, Cajochen C, Werth E, Hock C. A rapid-cycling bipolar patient treated with long nights, bedrest, and light. Biol Psychiatry. 1999; 45:1075–1077.
Article95. Barbini B, Benedetti F, Colombo C, Dotoli D, Bernasconi A, Cigala-Fulgosi M, et al. Dark therapy for mania: a pilot study. Bipolar Disord. 2005; 7:98–101.
Article96. Henriksen TE, Skrede S, Fasmer OB, Schoeyen H, Leskauskaite I, Bjørke-Bertheussen J, et al. Blue-blocking glasses as additive treatment for mania: a randomized placebo-controlled trial. Bipolar Disord. 2016; 18:221–232.
Article97. Frank E, Kupfer DJ, Thase ME, Mallinger AG, Swartz HA, Fagiolini AM, et al. Two-year outcomes for interpersonal and social rhythm therapy in individuals with bipolar I disorder. Arch Gen Psychiatry. 2005; 62:996–1004.
Article98. Frank E, Swartz HA, Boland E. Interpersonal and social rhythm therapy: an intervention addressing rhythm dysregulation in bipolar disorder. Dialogues Clin Neurosci. 2007; 9:325–332.
Article99. Harvey AG, Soehner AM, Kaplan KA, Hein K, Lee J, Kanady J, et al. Treating insomnia improves mood state, sleep, and functioning in bipolar disorder: a pilot randomized controlled trial. J Consult Clin Psychol. 2015; 83:564–577.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Bipolar Disorder, Circadian Rhythm and Clock Genes
- Circadian Rhythm Hypotheses of Mixed Features, Antidepressant Treatment Resistance, and Manic Switching in Bipolar Disorder
- Sleep Disorders in Bipolar Disorders: A Narrative Review on Circadian Rhythm Disturbances and Sleep Apnoea
- Melatonin in Psychiatric Disorders
- Is Advancing Circadian Rhythm the Mechanism of Antidepressants?