Korean J Orthod.
2016 Nov;46(6):395-408. 10.4041/kjod.2016.46.6.395.
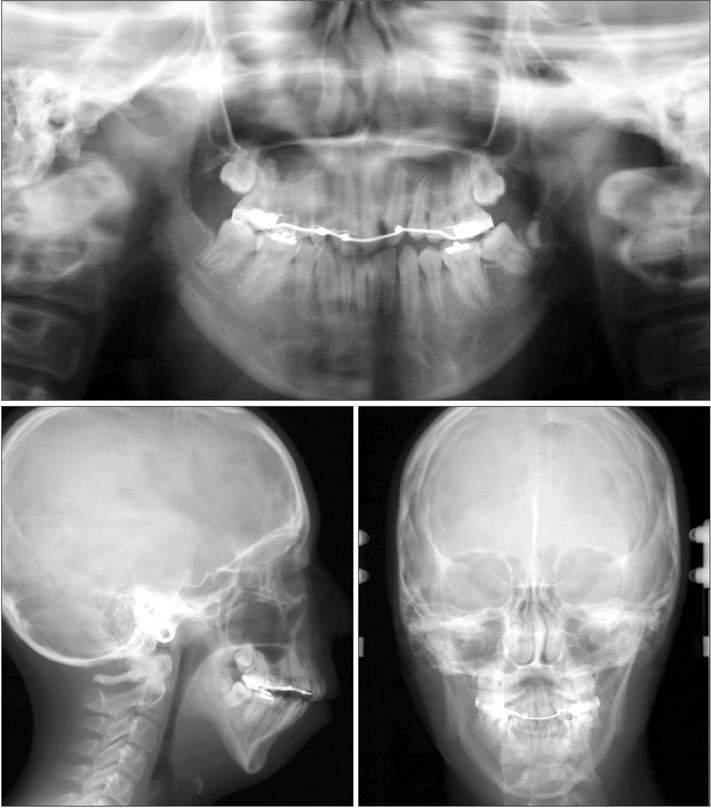
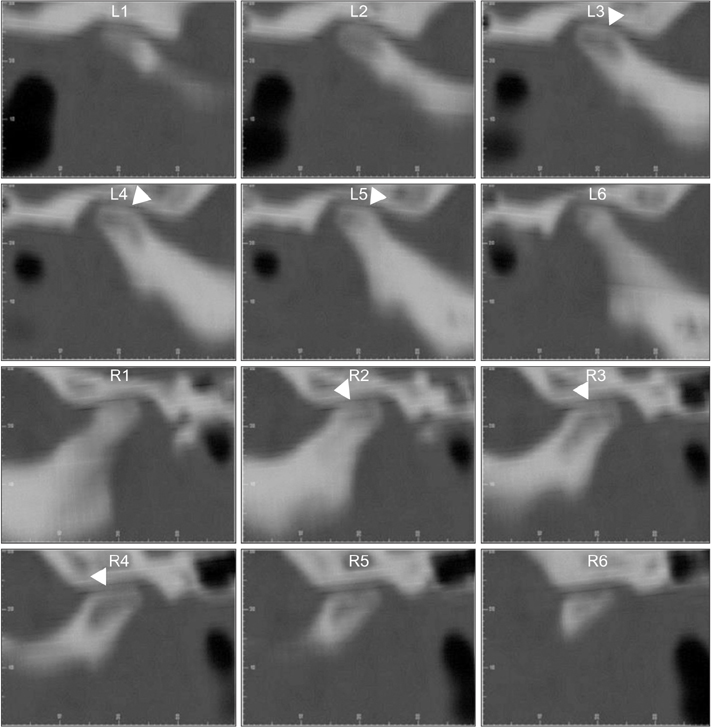
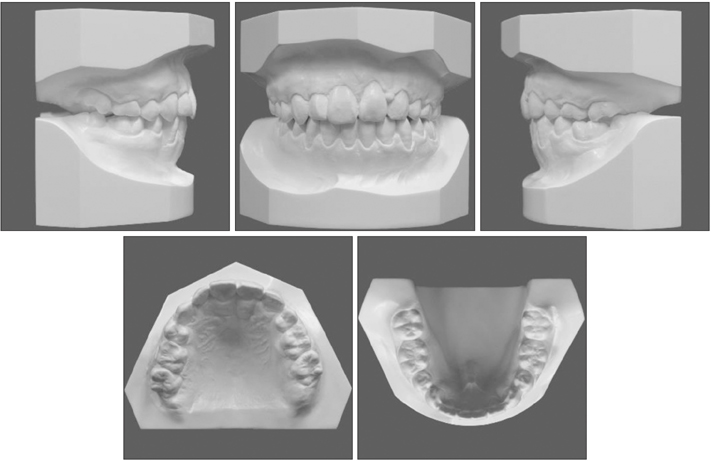
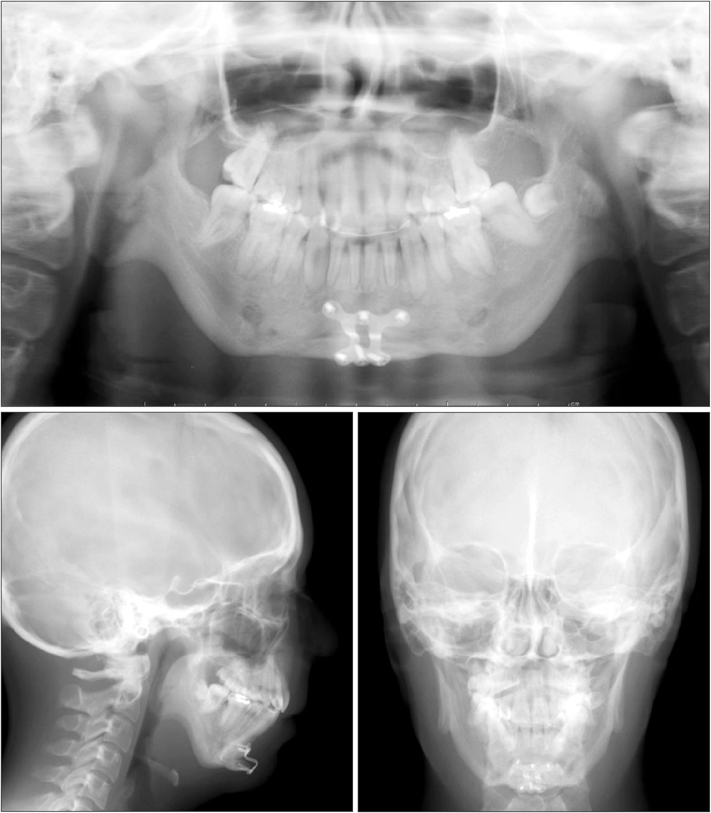
A case of severe mandibular retrognathism with bilateral condylar deformities treated with Le Fort I osteotomy and two advancement genioplasty procedures
- Affiliations
-
- 1Department of Orthodontics, Okayama University Hospital, Okayama, Japan. yanagita@md.okayama-u.ac.jp
- 2Department of Oral and Maxillofacial Reconstructive Surgery, Okayama University Graduate School of Medicine, Dentistry and Pharmaceutical Sciences, Okayama, Japan.
- 3Department of Orthodontics and Dentofacial Orthopedics, Graduate School of Dentistry, Osaka University, Osaka, Japan.
- 4Department of Orthodontics, Okayama University Graduate School of Medicine, Dentistry and Pharmaceutical Sciences, Okayama, Japan.
- KMID: 2426684
- DOI: http://doi.org/10.4041/kjod.2016.46.6.395
Abstract
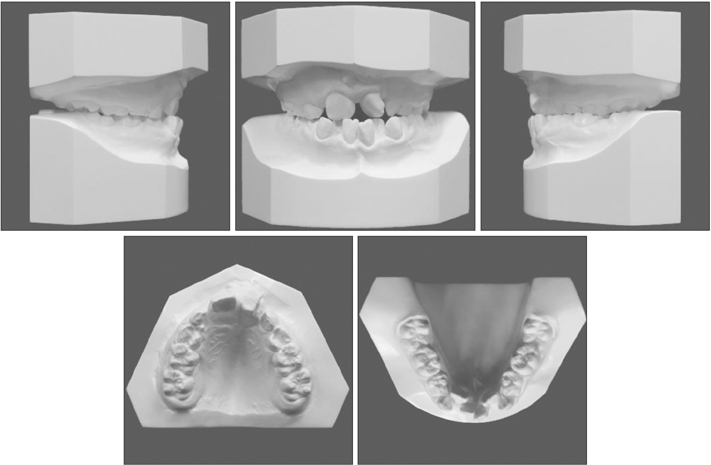
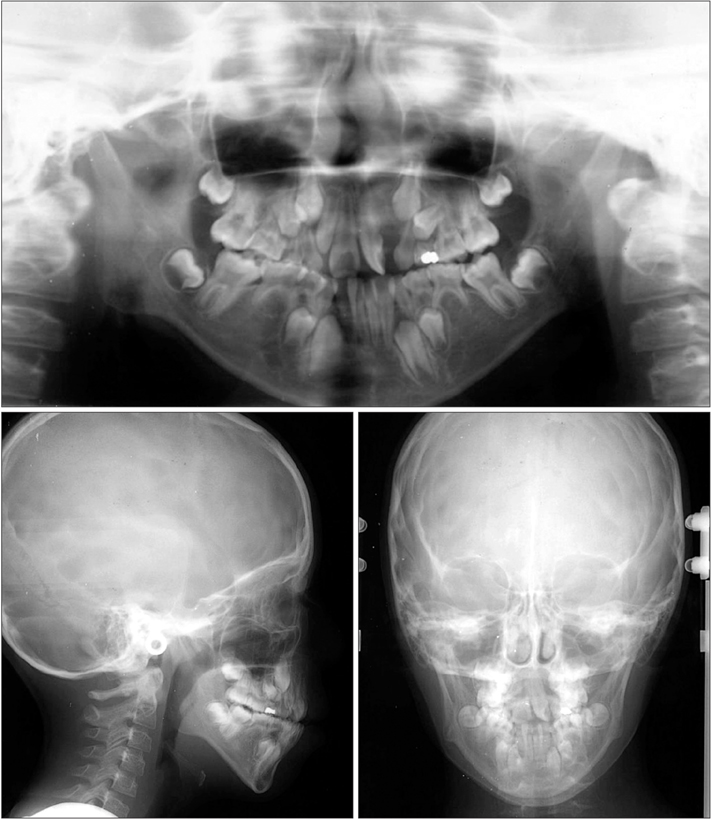
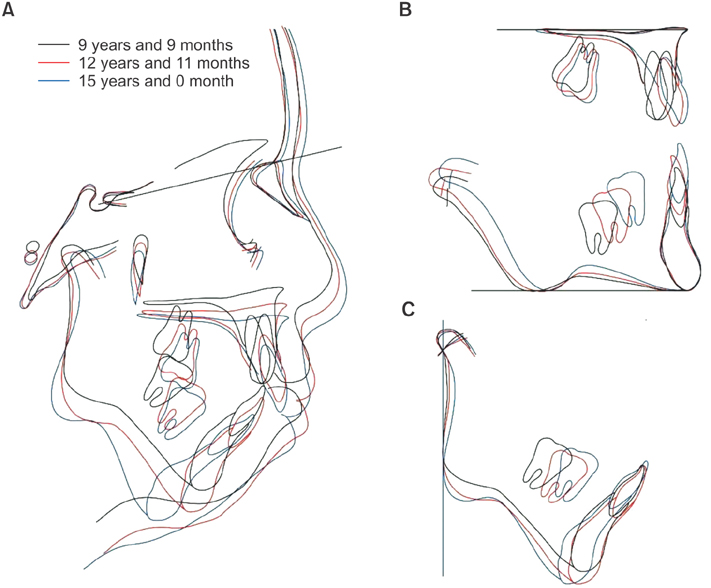
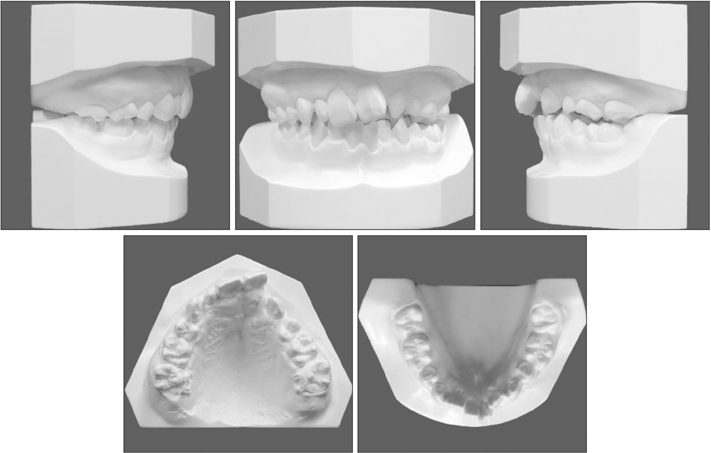
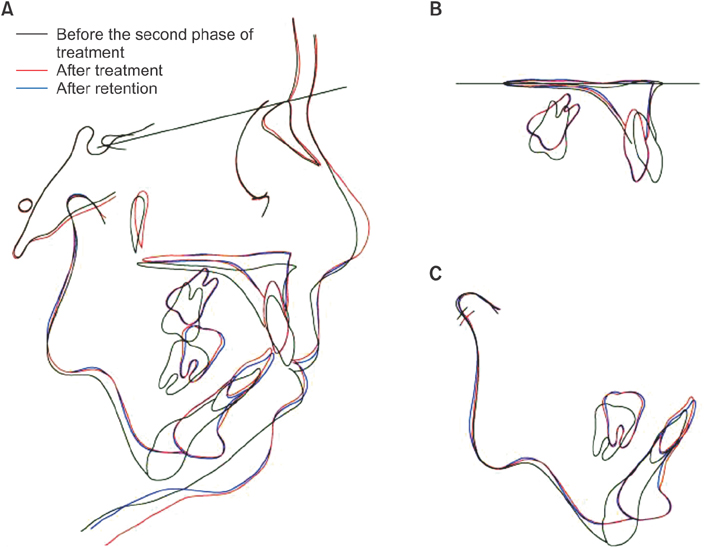
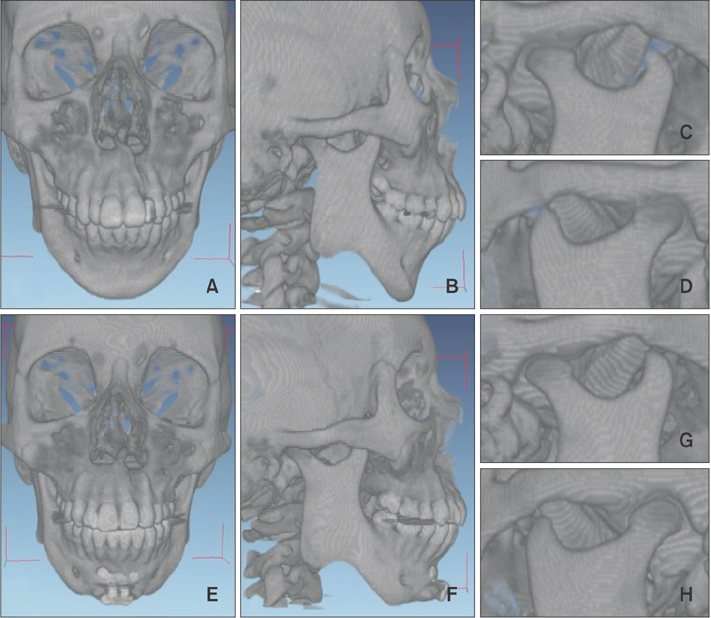
- We report a case involving a young female patient with severe mandibular retrognathism accompanied by mandibular condylar deformity that was effectively treated with Le Fort I osteotomy and two genioplasty procedures. At 9 years and 9 months of age, she was diagnosed with Angle Class III malocclusion, a skeletal Class II jaw relationship, an anterior crossbite, congenital absence of some teeth, and a left-sided cleft lip and palate. Although the anterior crossbite and narrow maxillary arch were corrected by interceptive orthodontic treatment, severe mandibular hypogrowth resulted in unexpectedly severe mandibular retrognathism after growth completion. Moreover, bilateral condylar deformities were observed, and we suspected progressive condylar resorption (PCR). There was a high risk of further condylar resorption with mandibular advancement surgery; therefore, Le Fort I osteotomy with two genioplasty procedures was performed to achieve counterclockwise rotation of the mandible and avoid ingravescence of the condylar deformities. The total duration of active treatment was 42 months. The maxilla was impacted by 7.0 mm and 5.0 mm in the incisor and molar regions, respectively, while the pogonion was advanced by 18.0 mm. This significantly resolved both skeletal disharmony and malocclusion. Furthermore, the hyoid bone was advanced, the pharyngeal airway space was increased, and the morphology of the mandibular condyle was maintained. At the 30-month follow-up examination, the patient exhibited a satisfactory facial profile. The findings from our case suggest that severe mandibular retrognathism with condylar deformities can be effectively treated without surgical mandibular advancement, thus decreasing the risk of PCR.
MeSH Terms
Figure
Reference
-
1. Proffit WR, Phillips C, Douvartzidis N. A comparison of outcomes of orthodontic and surgical-orthodontic treatment of Class II malocclusion in adults. Am J Orthod Dentofacial Orthop. 1992; 101:556–565.
Article2. Mihalik CA, Proffit WR, Phillips C. Long-term follow-up of Class II adults treated with orthodontic camouflage: a comparison with orthognathic surgery outcomes. Am J Orthod Dentofacial Orthop. 2003; 123:266–278.
Article3. Muto T, Yamazaki A, Takeda S. A cephalometric evaluation of the pharyngeal airway space in patients with mandibular retrognathia and prognathia, and normal subjects. Int J Oral Maxillofac Surg. 2008; 37:228–231.
Article4. Achilleos S, Krogstad O, Lyberg T. Surgical mandibular advancement and changes in uvuloglossopharyngeal morphology and head posture: a short- and long-term cephalometric study in males. Eur J Orthod. 2000; 22:367–381.
Article5. Proffit WR, Turvey TA, Phillips C. The hierarchy of stability and predictability in orthognathic surgery with rigid fixation: an update and extension. Head Face Med. 2007; 3:21.
Article6. Schreuder WH, Jansma J, Bierman MW, Vissink A. Distraction osteogenesis versus bilateral sagittal split osteotomy for advancement of the retrognathic mandible: a review of the literature. Int J Oral Maxillofac Surg. 2007; 36:103–110.
Article7. Baas EM, Pijpe J, de Lange J. Long term stability of mandibular advancement procedures: bilateral sagittal split osteotomy versus distraction osteogenesis. Int J Oral Maxillofac Surg. 2012; 41:137–141.
Article8. Hoppenreijs TJ, Stoelinga PJ, Grace KL, Robben CM. Long-term evaluation of patients with progressive condylar resorption following orthognathic surgery. Int J Oral Maxillofac Surg. 1999; 28:411–418.
Article9. Arnett GW, Milam SB, Gottesman L. Progressive mandibular retrusion-idiopathic condylar resorption. Part II. Am J Orthod Dentofacial Orthop. 1996; 110:117–127.
Article10. Cutbirth M, Van Sickels JE, Thrash WJ. Condylar resorption after bicortical screw fixation of mandibular advancement. J Oral Maxillofac Surg. 1998; 56:178–182. discussion 183.
Article11. Kobayashi T, Izumi N, Kojima T, Sakagami N, Saito I, Saito C. Progressive condylar resorption after mandibular advancement. Br J Oral Maxillofac Surg. 2012; 50:176–180.
Article12. Wada K, Matsushita K, Shimazaki S, Miwa Y, Hasuike Y, Susami R. An evaluation of a new case analysis of a lateral cephalometric roentgenogram. J Kanazawa Med Univ. 1981; 6:60–70.13. van Strijen PJ, Breuning KH, Becking AG, Tuinzing DB. Condylar resorption following distraction osteogenesis: a case report. J Oral Maxillofac Surg. 2001; 59:1104–1107. discussion 1107-8.
Article14. Wolford LM, Cardenas L. Idiopathic condylar resorption: diagnosis, treatment protocol, and outcomes. Am J Orthod Dentofacial Orthop. 1999; 116:667–677.
Article15. Hoppenreijs TJ, Freihofer HP, Stoelinga PJ, Tuinzing DB, van't Hof MA. Condylar remodelling and resorption after Le Fort I and bimaxillary osteotomies in patients with anterior open bite. A clinical and radiological study. Int J Oral Maxillofac Surg. 1998; 27:81–91.
Article16. Hayes RJ, Sarver DM, Jacobson A. The quantification of soft tissue cervicomental changes after mandibular advancement surgery. Am J Orthod Dentofacial Orthop. 1994; 105:383–391.
Article17. Kezirian EJ, Goldberg AN. Hypopharyngeal surgery in obstructive sleep apnea: an evidence-based medicine review. Arch Otolaryngol Head Neck Surg. 2006; 132:206–213.18. Hendler B, Silverstein K, Giannakopoulos H, Costello BJ. Mortised genioplasty in the treatment of obstructive sleep apnea: an historical perspective and modification of design. Sleep Breath. 2001; 5:173–180.
Article19. Nagler RM, Laufer D. Genioglossal advancement--a simple surgical procedure for sleep apnea. Case report and literature review. Eur Surg Res. 2002; 34:373–377.
Article20. Teittinen M, Tuovinen V, Tammela L, Schätzle M, Peltomäki T. Long-term stability of anterior open bite closure corrected by surgical-orthodontic treatment. Eur J Orthod. 2012; 34:238–243.
Article21. Pagnoni M, Amodeo G, Fadda MT, Brauner E, Guarino G, Virciglio P, et al. Juvenile idiopathic/rheumatoid arthritis and orthognatic surgery without mandibular osteotomies in the remittent phase. J Craniofac Surg. 2013; 24:1940–1945.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A case report of surgical correction of mandibular prognathism with midfacial deficiency using Le Fort III osteotomy
- Comparison of Postoperative Stability between Distraction Osteogenesis and Bilateral Sagittal Split Ramus Osteotomy in Mandibular Retrognathism
- Surgical Management of Atypical Apert Syndrome Patient Using Combined Cranial and Maxillofacial Surgery
- Combined orthodontic-surgical treatment for Class III patient with midfacial deficiency and mandibular prognathism
- Le Fort I osteotomy as treatment for traumatic class III malocclusion caused by Le Fort III fracture: A case report