J Neurocrit Care.
2018 Jun;11(1):47-53. 10.18700/jnc.180045.
Miliary Tuberculosis Mimicking Brain Metastasis from Renal Cell Carcinoma
- Affiliations
-
- 1Department of Pulmonary and Critical Care Medicine, Kangdong Sacred Heart Hospital, Hallym University College of Medicine, Seoul, Korea.
- 2Department of Neurology, Busan Paik Hospital, Inje University College of Medicine, Busan, Korea.
- 3Department of Neurology, Kangdong Sacred Heart Hospital, Hallym University College of Medicine, Seoul, Korea. brainyrk@gmail.com
- KMID: 2426214
- DOI: http://doi.org/10.18700/jnc.180045
Abstract
- BACKGROUND
Miliary tuberculosis (TB) can cause diagnostic confusion for clinicians because its radiological appearance can resemble that of metastatic cancer.
CASE REPORT
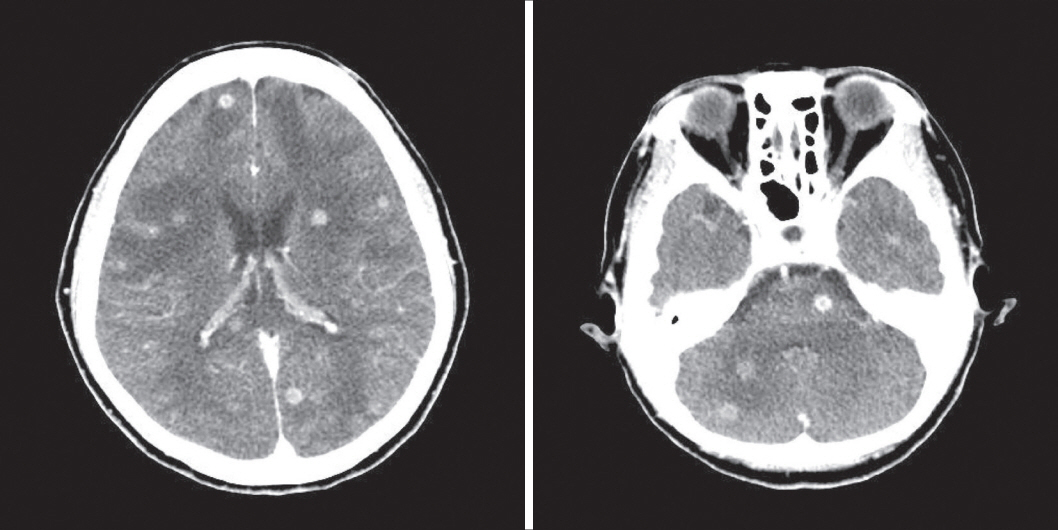
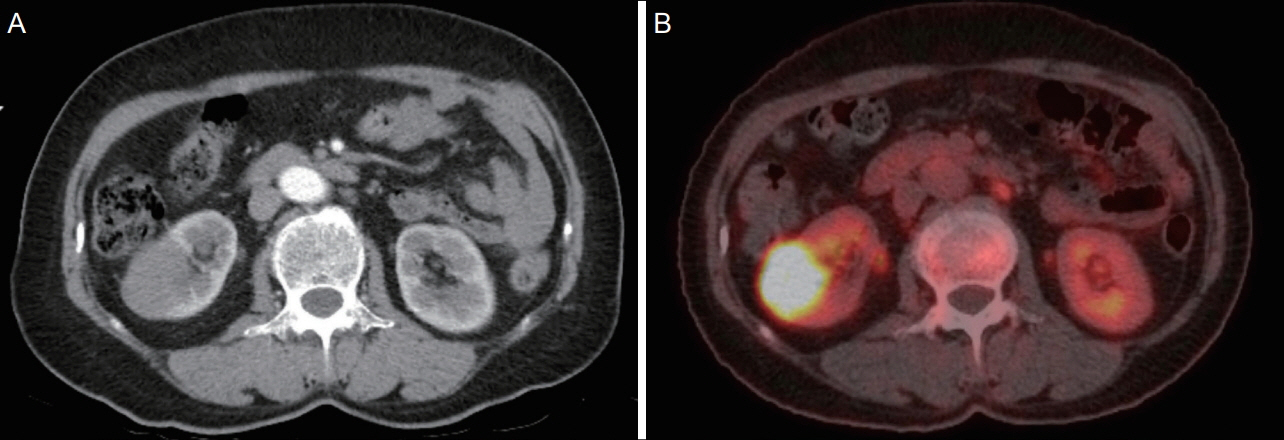
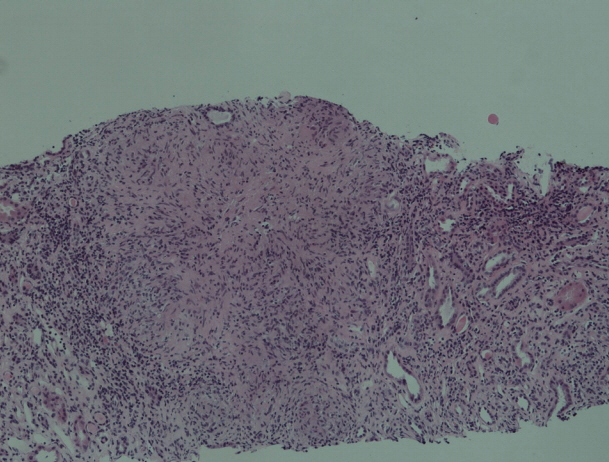
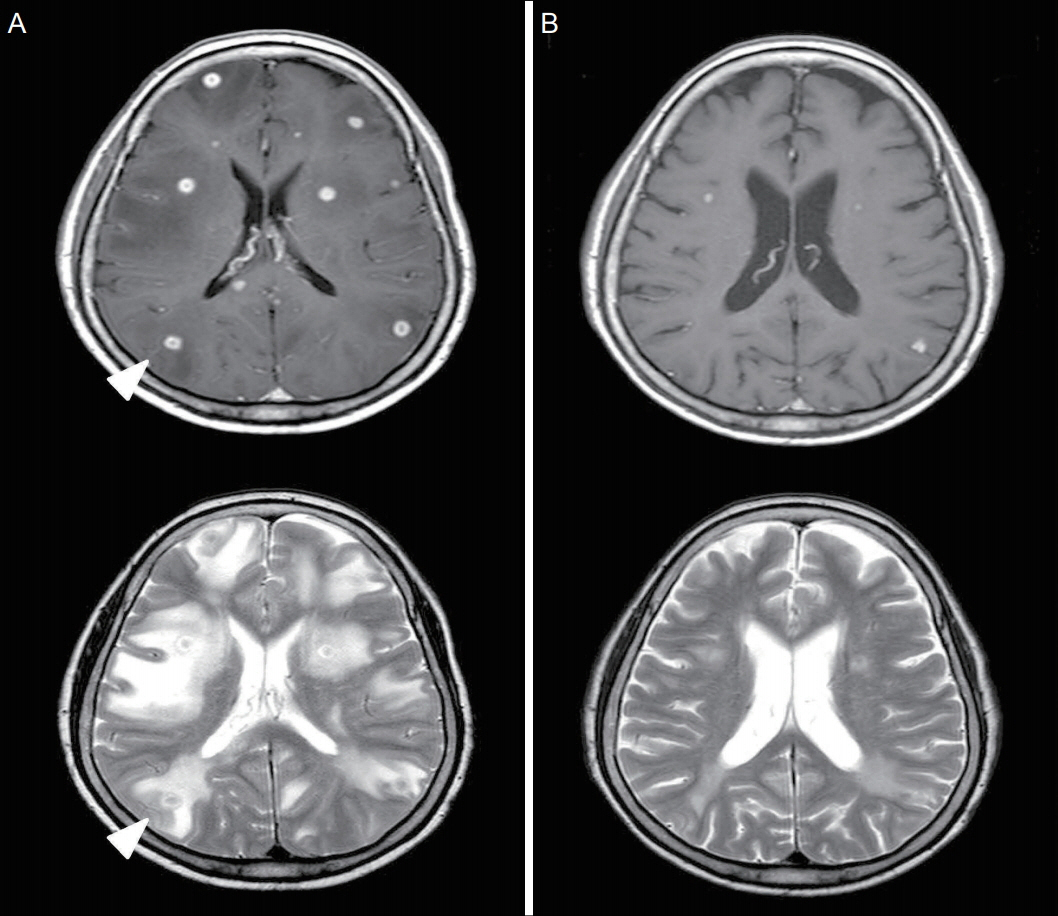
Here, we describe the case of a 72-yearold woman with miliary TB mimicking brain metastasis from renal cell carcinoma. The patient visited our clinic because of dysarthria and sluggish speech. A metastatic cancer such as renal cell carcinoma or brain tumor was suspected. However, the patient was diagnosed with miliary TB associated with multiple intracranial tuberculomas and a subsequent paradoxical response to anti-TB therapy.
CONCLUSION
Clinicians should be aware that miliary TB can mimic metastatic cancer even in older people, especially in TB-endemic regions.
MeSH Terms
Figure
Reference
-
1. Centers for Disease Control and Prevention. Reported tuberculosis in the United States, 2012 [online]. Available at: https://www.cdc.gov/tb/. Accessed at April 5, 2018.2. Greschus S, Kuchelmeister K, Oeynhausen S, Fischer HP, Urbach H. Cerebral tuberculoma mimicking brain tumor. Clin Neuroradiol. 2014; 24:389–93.
Article3. Sharma SK, Mohan A, Sharma A, Mitra DK. Miliary tuberculosis: new insights into an old disease. Lancet Infect Dis. 2005; 5:415–30.
Article4. Ko KT, Na DJ, Han SH, Jung SS, Moon KM, Kim DJ, et al. Unusual presentation of miliary tuberculosis. Tuberc Respir Dis. 2007; 63:67–71.
Article5. Sharma SK, Mohan A, Sharma A. Challenges in the diagnosis & treatment of miliary tuberculosis. Indian J Med Res. 2012; 135:703–30.6. Burk JR, Viroslav J, Bynum LJ. Miliary tuberculosis diagnosed by fibreoptic bronchoscopy and transbronchial biopsy. Tubercle. 1978; 59:107–9.
Article7. Wasay M. Central nervous system tuberculosis and paradoxical response. South Med J. 2006; 99:331–2.
Article8. Breen RA, Smith CJ, Bettinson H, Dart S, Bannister B, Johnson MA, et al. Paradoxical reactions during tuberculosis treatment in patients with and without HIV co-infection. Thorax. 2004; 59:704–7.
Article9. Cheng VC, Yam WC, Woo PC, Lau SK, Hung IF, Wong SP, et al. Risk factors for development of paradoxical response during antituberculosis therapy in HIV-negative patients. Eur J Clin Microbiol Infect Dis. 2003; 22:597–602.
Article10. Singh AK, Malhotra HS, Garg RK, Jain A, Kumar N, Kohli N, et al. Paradoxical reaction in tuberculous meningitis: presentation, predictors and impact on prognosis. BMC Infect Dis. 2016; 16:306.
Article11. Garg RK, Sinha MK. Multiple ring-enhancing lesions of the brain. J Postgrad Med. 2010; 56:307–16.
Article12. Rock RB, Olin M, Baker CA, Molitor TW, Peterson PK. Central nervous system tuberculosis: pathogenesis and clinical aspects. Clin Microbiol Rev. 2008; 21:243–61. table of contents.
Article13. Baker CA, Cartwright CP, Williams DN, Nelson SM, Peterson PK. Early detection of central nervous system tuberculosis with the gen-probe nucleic Acid amplification assay: utility in an inner city hospital. Clin Infect Dis. 2002; 35:339–42.
Article14. Lin JJ, Harn HJ, Hsu YD, Tsao WL, Lee HS, Lee WH. Rapid diagnosis of tuberculous meningitis by polymerase chain reaction assay of cerebrospinal fluid. J Neurol. 1995; 242:147–52.
Article15. Möller-Hartmann W, Herminghaus S, Krings T, Marquardt G, Lanfermann H, Pilatus U, et al. Clinical application of proton magnetic resonance spectroscopy in the diagnosis of intracranial mass lesions. Neuroradiology. 2002; 44:371–81.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Miliary Tuberculosis and Multiple Intracranial Tuberculoma : A Case Report
- A Case of Subcutaneous Tissue Metastasis of Renal Cell Carcinoma
- A Case of Metastatic Tuberculosis Abscess Associated with Miliary Tuberculosis
- A Case of Cervical Adenocarcinoma with Pulmonary Metastasis Resembling Miliary Tuberculosis
- Comparison of High-resolution CT Findings between Miliary Metastases and Miliary Tuberculosis