Intest Res.
2017 Apr;15(2):195-202. 10.5217/ir.2017.15.2.195.
Patients with computed tomography-proven acute diverticulitis require follow-up to exclude colorectal cancer
- Affiliations
-
- 1Department of General Surgery, Sandwell & West Birmingham Hospitals NHS Trust, Sandwell General Hospital, West Bromwich, UK.
- 2Nurse Consultant and Clinical Lead for Endoscopy at City Hospital Endoscopy Unit, Sandwell & West Birmingham Hospitals NHS Trust, Birmingham City Hospital, Birmingham, UK.
- 3Department of Gastroenterology, Sandwell & West Birmingham Hospitals NHS Trust, Sandwell General Hospital, West Bromwich, UK.
- 4Department of General Surgery, University Hospitals Coventry & Warwickshire NHS Trust, Walsgrave, UK. stephen.ward7@nhs.net
- KMID: 2425161
- DOI: http://doi.org/10.5217/ir.2017.15.2.195
Abstract
- BACKGROUND/AIMS
Traditionally, patients with acute diverticulitis undergo follow-up endoscopy to exclude colorectal cancer (CRC). However, its usefulness has been debated in this era of high-resolution computed tomography (CT) diagnosis. We assessed the frequency and outcome of endoscopic follow-up for patients with CT-proven acute diverticulitis, according to the confidence in the CT diagnosis.
METHODS
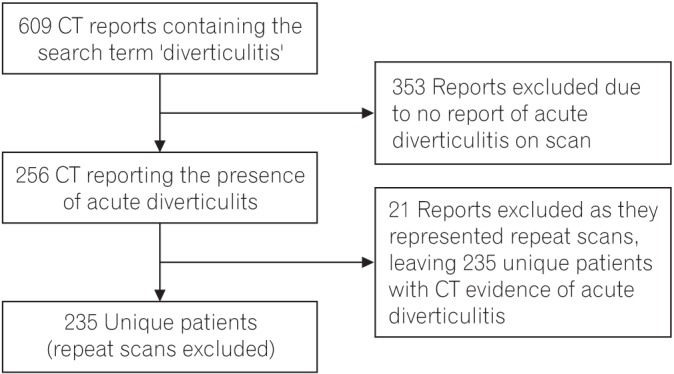
Records of patients with CT-proven acute diverticulitis between October 2007 and March 2014 at Sandwell & West Birmingham Hospitals NHS Trust were retrieved. The National Cancer Registry confirmed the cases of CRC. Endoscopy quality indicators were compared between these patients and other patients undergoing the same endoscopic examination over the same period.
RESULTS
We identified 235 patients with CT-proven acute diverticulitis, of which, 187 were managed conservatively. The CT report was confident of the diagnosis of acute diverticulitis in 75% cases. Five of the 235 patients were subsequently diagnosed with CRC (2.1%). Three cases of CRC were detected in the 187 patients managed conservatively (1.6%). Forty-eight percent of the conservatively managed patients underwent follow-up endoscopy; one case of CRC was identified. Endoscopies were often incomplete and caused more discomfort for patients with diverticulitis compared with controls.
CONCLUSIONS
CRC was diagnosed in patients with CT-proven diverticulitis at a higher rate than in screened asymptomatic populations, necessitating follow-up. CT reports contained statements regarding diagnostic uncertainty in 25% cases, associated with an increased risk of CRC. Follow-up endoscopy in patients with CT-proven diverticulitis is associated with increased discomfort and high rates of incompletion. The use of other follow-up modalities should be considered.
Keyword
MeSH Terms
Figure
Reference
-
1. Hughes LE. Postmortem survey of diverticular disease of the colon: I. diverticulosis and diverticulitis. Gut. 1969; 10:336–344. PMID: 5771665.
Article2. Matrana MR, Margolin DA. Epidemiology and pathophysiology of diverticular disease. Clin Colon Rectal Surg. 2009; 22:141–146. PMID: 20676256.
Article3. Fozard JB, Armitage NC, Schofield JB, Jones OM. Association of Coloproctology of Great Britain and Ireland. ACPGBI position statement on elective resection for diverticulitis. Colorectal Dis. 2011; 13(Suppl 3):1–11.
Article4. Colinic diverticular disease: commissioning guide. Royal College of Surgeons Web site. Accessed February 23, 2017. https://www.rcseng.ac.uk/library-and-publications/college-publications/docs/colinic-diverticular-disease/.5. Sai VF, Velayos F, Neuhaus J, Westphalen AC. Colonoscopy after CT diagnosis of diverticulitis to exclude colon cancer: a systematic literature review. Radiology. 2012; 263:383–390. PMID: 22517956.
Article6. Schmilovitz-Weiss H, Yalunin E, Boaz M, et al. Does a colonoscopy after acute diverticulitis affect its management? A single center experience. J Clin Gastroenterol. 2012; 46:317–320. PMID: 22186742.7. Page AA, Khan A, Rajaratnam S, Carroll N, Hall NR, Davies RJ. Is follow-up endoscopy necessary after successful medical treatment of CT-proven acute diverticulitis? Gut. 2011; 60(Suppl 1):A72.8. Sharma PV, Eglinton T, Hider P, Frizelle F. Systematic review and meta-analysis of the role of routine colonic evaluation after radiologically confirmed acute diverticulitis. Ann Surg. 2014; 259:263–272. PMID: 24169174.
Article9. Lau KC, Spilsbury K, Farooque Y, et al. Is colonoscopy still mandatory after a CT diagnosis of left-sided diverticulitis: can colorectal cancer be confidently excluded? Dis Colon Rectum. 2011; 54:1265–1270. PMID: 21904141.
Article10. Rao PM, Rhea JT, Novelline RA, et al. Helical CT with only colonic contrast material for diagnosing diverticulitis: prospective evaluation of 150 patients. AJR Am J Roentgenol. 1998; 170:1445–1449. PMID: 9609151.11. Westwood DA, Eglinton TW, Frizelle FA. Routine colonoscopy following acute uncomplicated diverticulitis. Br J Surg. 2011; 98:1630–1634. PMID: 21713756.
Article12. Lahat A, Yanai H, Sakhnini E, Menachem Y, Bar-Meir S. Role of colonoscopy in patients with persistent acute diverticulitis. World J Gastroenterol. 2008; 14:2763–2766. PMID: 18461662.
Article13. Elmi A, Hedgire SS, Pargaonkar V, Cao K, McDermott S, Harisinghani M. Is early colonoscopy beneficial in patients with CTdiagnosed diverticulitis? AJR Am J Roentgenol. 2013; 200:1269–1274. PMID: 23701063.
Article14. van de Wall BJ, Reuling EM, Consten EC, et al. Endoscopic evaluation of the colon after an episode of diverticulitis: a call for a more selective approach. Int J Colorectal Dis. 2012; 27:1145–1150. PMID: 22407442.
Article15. Sallinen V, Mentula P, Leppäniemi A. Risk of colon cancer after computed tomography-diagnosed acute diverticulitis: is routine colonoscopy necessary? Surg Endosc. 2014; 28:961–966. PMID: 24178863.
Article16. Daniels L, Ünlü Ç, de Wijkerslooth TR, et al. Yield of colonoscopy after recent CT-proven uncomplicated acute diverticulitis: a comparative cohort study. Surg Endosc. 2015; 29:2605–2613. PMID: 25472747.
Article17. Brar MS, Roxin G, Yaffe PB, Stanger J, MacLean AR, Buie WD. Colonoscopy following nonoperative management of uncomplicated diverticulitis may not be warranted. Dis Colon Rectum. 2013; 56:1259–1264. PMID: 24105001.
Article18. Niv Y, Hazazi R, Levi Z, Fraser G. Screening colonoscopy for colorectal cancer in asymptomatic people: a meta-analysis. Dig Dis Sci. 2008; 53:3049–3054. PMID: 18463980.
Article19. Goh V, Halligan S, Taylor SA, Burling D, Bassett P, Bartram CI. Differentiation between diverticulitis and colorectal cancer: quantitative CT perfusion measurements versus morphologic criteria--initial experience. Radiology. 2007; 242:456–462. PMID: 17255417.
Article20. Destigter KK, Keating DP. Imaging update: acute colonic diverticulitis. Clin Colon Rectal Surg. 2009; 22:147–155. PMID: 20676257.21. Dafnis G, Granath F, Påhlman L, Ekbom A, Blomqvist P. Patient factors influencing the completion rate in colonoscopy. Dig Liver Dis. 2005; 37:113–118. PMID: 15733524.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Is Colonoscopy Necessary after Computed Tomography Diagnosis of Acute Diverticulitis?
- Colon Cancer After Acute Diverticulitis Treatment
- Diagnosis and Treatment of Colon Diverticulitis
- Acute diverticulitis of the terminal ileum: ultrasonography and CT findings
- Risk Factors for Severe Diverticulitis in Computed Tomography-Confirmed Acute Diverticulitis in Korea