J Breast Cancer.
2010 Sep;13(3):257-266.
Mutation-Free Expression of c-Kit and PDGFRA in Phyllodes Tumors of the Breast
- Affiliations
-
- 1Department of Pathology, Research Institute for Medical Sciences, Chungnam National University School of Medicine, Daejeon, Korea. kssuh@cnu.ac.kr
- 2Department of Surgery, Chungnam National University School of Medicine, Daejeon, Korea.
- 3Department of Pathology, Catholic University Daejeon St. Mary's Hospital, Daejeon, Korea.
- 4Department of Pathology, Eulji Hospital, Daejeon, Korea.
Abstract
- PURPOSE
Phyllodes tumors (PTs) of the breast have been classified as benign, borderline, or malignant based on their histopathologic features. However, predicting clinical behavior based on these features has proven to be difficult given that local recurrence occurs in both benign and malignant PTs. Recurrence has been shown to mirror the histologic pattern of the primary tumor or to show dedifferentiation. The aim of this study was to assess the value of the histopathologic parameters, expression or mutation of c-Kit and platelet derived growth factor receptor alpha (PDGFRA) in predicting tumor recurrence.
METHODS
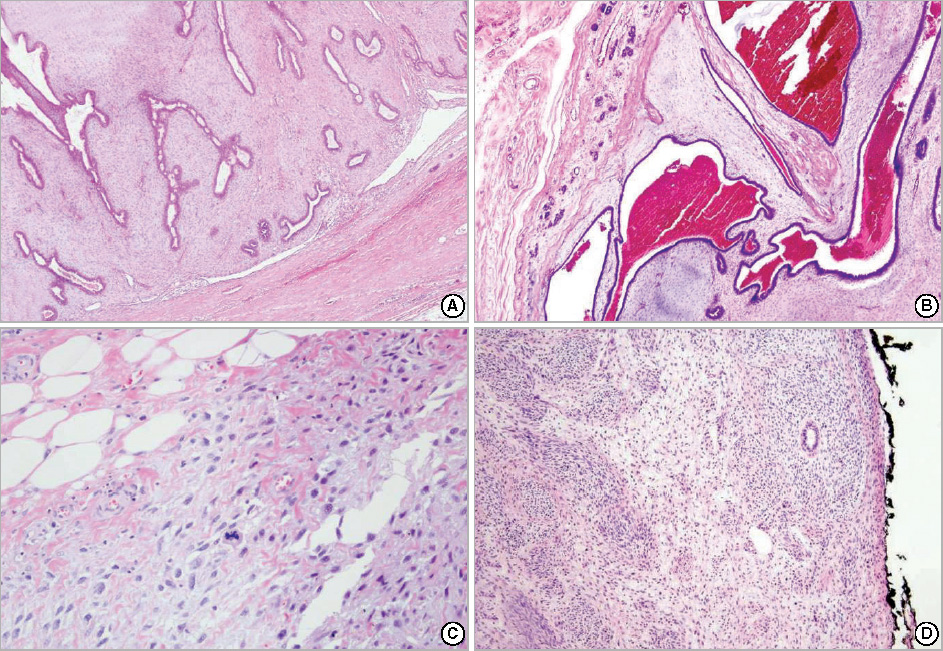
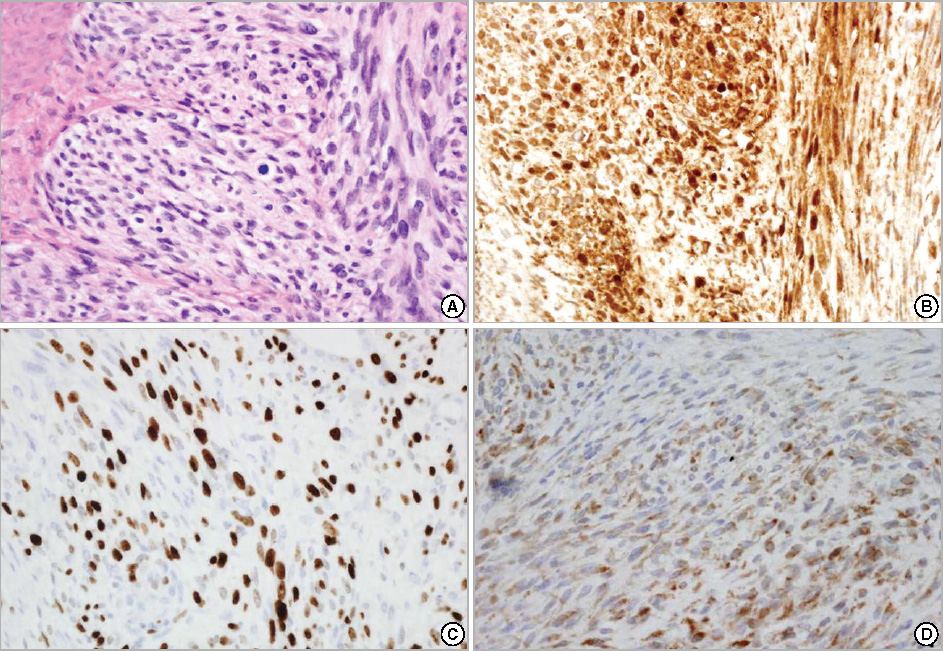
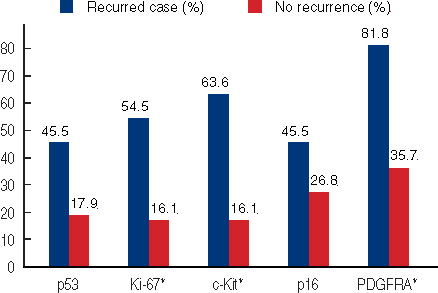
Representative areas from 39 benign, 16 borderline, and 12 malignant PTs were selected for construction of tissue microarrays. Immunohistochemical analyses for p53, Ki-67, c-Kit, and PDGFRA were performed and SSCP-PCR analysis was carried out to identify mutations in exons 9, 11, 13, and 17 of the c-Kit gene and exons 12 and 18 of the PDGFRA gene. Clinicopathologic features, including tumor recurrence and margin status, were also evaluated.
RESULTS
Of the 67 PTs, 11 cases (16.4%) recurred from 3 to 92 months following initial diagnosis (4 benign, 2 borderline, and 5 malignant). One benign PT case recurred as a borderline tumor and two borderline PT cases recurred as malignancies. Three patients died of malignant PT. No mutations of the c-Kit or PDGFRA genes were found and there was no statistically significant association of either p53 or p16 immunostaining with recurrent disease (p>0.05). However, histologic grade (p=0.033), margin status (p<0.001), Ki-67 (p=0.012), c-Kit (p=0.002), and PDGFRA (p=0.007) stromal immunopositivity were significantly correlated with recurrence.
CONCLUSION
Even though positive or close margins were significantly associated with tumor recurrence, stromal c-Kit, PDGFRA positivity, and the Ki-67 index were useful for predicting recurrent PTs. Despite this, no c-Kit or PDGFRA mutations were found.
Keyword
MeSH Terms
Figure
Reference
-
1. O'Malley F, Pinder SE. Breast Pathology. 2006. Edinburgh: Churchill Livingstone Elsevier;118–124.2. Rowell MD, Perry RR, Hsiu JG, Barranco SC. Phyllodes tumors. Am J Surg. 1993. 165:376–379.
Article3. Jacklin RK, Ridgway PF, Ziprin P, Healy V, Hadjiminas D, Darzi A. Optimising preoperative diagnosis in phyllodes tumour of the breast. J Clin Pathol. 2006. 59:454–459.
Article4. Khan SA, Badve S. Phyllodes tumors of the breast. Curr Treat Options Oncol. 2001. 2:139–147.
Article5. Inoshita S. Phyllodes tumor (cystosarcoma phyllodes) of the breast. A clinicopathologic study of 45 cases. Acta Pathol Jpn. 1988. 38:21–33.
Article6. Bellocq JP, Margo G. Tavassoli FA, Devilee P, editors. Fibroepithelial tumours. World Health Organization Classification of Tumours. Pathology and Genetics of Tumours of the Breast and Female Genital Organs. 2003. Lyon: IARC Press;99–103.7. Chen CM, Chen CJ, Chang CL, Shyu JS, Hsieh HF, Harn HJ. CD34, CD117, and actin expression in phyllodes tumor of the breast. J Surg Res. 2000. 94:84–91.
Article8. Sawyer EJ, Poulsom R, Hunt FT, Jeffery R, Elia G, Ellis IO, et al. Malignant phyllodes tumours show stromal overexpression of c-myc and c-kit. J Pathol. 2003. 200:59–64.
Article9. Tse GM, Putti TC, Lui PC, Lo AW, Scolyer RA, Law BK, et al. Increased c-kit (CD117) expression in malignant mammary phyllodes tumors. Mod Pathol. 2004. 17:827–831.
Article10. Tan PH, Jayabaskar T, Yip G, Tan Y, Hilmy M, Selvarajan S, et al. p53 and c-kit (CD117) protein expression as prognostic indicators in breast phyllodes tumors: a tissue microarray study. Mod Pathol. 2005. 18:1527–1534.
Article11. Esposito NN, Mohan D, Brufsky A, Lin Y, Kapali M, Dabbs DJ. Phyllodes tumor: a clinicopathologic and immunohistochemical study of 30 cases. Arch Pathol Lab Med. 2006. 130:1516–1521.
Article12. Carvalho I, Milanezi F, Martins A, Reis RM, Schmitt F. Overexpression of platelet-derived growth factor receptor alpha in breast cancer is associated with tumour progression. Breast Cancer Res. 2005. 7:R788–R795.13. Sarlomo-Rikala M, Kovatich AJ, Barusevicius A, Miettinen M. CD117: a sensitive marker for gastrointestinal stromal tumors that is more specific than CD34. Mod Pathol. 1998. 11:728–734.14. Miettinen M, Monihan JM, Sarlomo-Rikala M, Kovatich AJ, Carr NJ, Emory TS, et al. Gastrointestinal stromal tumors/smooth muscle tumors (GISTs) primary in the omentum and mesentery: clinicopathologic and immunohistochemical study of 26 cases. Am J Surg Pathol. 1999. 23:1109–1118.
Article15. Miettinen M, Sobin LH, Sarlomo-Rikala M. Immunohistochemical spectrum of GISTs at different sites and their differential diagnosis with a reference to CD117 (KIT). Mod Pathol. 2000. 13:1134–1142.
Article16. Carvalho S, Silva AO, Milanezi F, Ricardo S, Leitão D, Amendoeira I, et al. c-KIT and PDGFRA in breast phyllodes tumours: overexpression without mutations? J Clin Pathol. 2004. 57:1075–1079.
Article17. Wardelmann E, Neidt I, Bierhoff E, Speidel N, Manegold C, Fischer HP, et al. c-kit mutations in gastrointestinal stromal tumors occur preferentially in the spindle rather than in the epithelioid cell variant. Mod Pathol. 2002. 15:125–136.
Article18. Yamamoto H, Oda Y, Kawaguchi K, Nakamura N, Takahira T, Tamiya S, et al. c-kit and PDGFRA mutations in extragastrointestinal stromal tumor (gastrointestinal stromal tumor of the soft tissue). Am J Surg Pahtol. 2004. 28:479–488.
Article19. Moinfar F. Essentials of Diagnostic Breast Pathology: A Practical Approach. 2007. Berlin: Springer-Verlag;321–323.20. Grimes MM. Cystosarcoma phyllodes of the breast: histologic features, flow cytometric analysis, and clinical correlations. Mod Pathol. 1992. 5:232–239.21. Kleer CG, Giordano TJ, Braun T. Pathologic, immunohistochemical, and molecular features of benign and malignant phyllodes tumors of the breast. Mod Pathol. 2001. 14:185–190.
Article22. Lee HS, Kim HA, Shin DS, Kim YH, Chung SY, Jin MS, et al. Risk factors for recurrence after surgical treatment of a malignant phyllodes tumor of the breast. J Breast Cancer. 2007. 10:248–253.
Article23. Song JY, Yoon HK. Immunohistochemical phenotypes of phyllodes tumor of the breast. Korean J Pathol. 2008. 42:151–156.24. Kocová L, Skálová A, Fakan F, Rousarová M. Phyllodes tumour of the breast: immunohistochemical study of 37 tumours using MIB1 antibody. Pathol Res Pract. 1998. 194:97–104.
Article25. Millar EK, Beretov J, Marr P, Sarris M, Clarke RA, Kearsley JH, et al. Malignant phyllodes tumours of the breast display increased stromal p53 protein expression. Histopathology. 1999. 34:491–496.
Article26. Feakins RM, Mulcahy HE, Nickols CD, Wells CA. p53 expression in phyllodes tumours is associated with histological features of malignancy but does not predict outcome. Histopathology. 1999. 35:162–169.
Article27. Tse GM, Putti TC, Kung FY, Scolyer RA, Law BK, Lau TS, et al. Increased p53 protein expression in malignant mammary phyllodes tumors. Mod Pathol. 2002. 15:734–740.
Article28. Paulsson J, Sjöblom T, Micke P, Pontén F, Landberg G, Heldin CH, et al. Prognostic significance of stromal platelet-derived growth factor beta-receptor expression in human breast cancer. Am J Pathol. 2009. 175:334–341.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Gastrointestinal stromal tumor with KIT mutation in neurofibromatosis type 1
- KIT/PDGFRA Expression and Mutation in Testicular Seminoma and Ovarian Dysgerminoma
- Expression of DOG1, PDGFRA, and p16 in Gastrointestinal Stromal Tumors
- Patterns of p53 expression in phyllodes tumors of the breast: an immunohistochemical study
- Mutation Analysis of Genes Related to Gastrointestinal Stromal Tumors