Cancer Res Treat.
2018 Oct;50(4):1214-1225. 10.4143/crt.2017.498.
Survival and Functional Outcome after Treatment for Primary Base of Tongue Cancer: A Comparison of Definitive Chemoradiotherapy versus Surgery Followed by Adjuvant Radiotherapy
- Affiliations
-
- 1Department of Radiation Oncology, Yonsei University College of Medicine, Seoul, Korea. CGLEE1023@yuhs.ac
- 2Department of Otorhinolaryngology, Yonsei University College of Medicine, Seoul, Korea.
- 3Department of Medical Oncology, Yonsei University College of Medicine, Seoul, Korea.
- 4Department of Radiation Oncology, University of Washington Medical Center, Seattle, WA, USA.
- KMID: 2424794
- DOI: http://doi.org/10.4143/crt.2017.498
Abstract
- PURPOSE
The purpose of this study was to compare the clinical and functional outcomes in patients with primary base of tongue (BOT) cancer who received definitive radiotherapy (RT) or surgery followed by radiotherapy (SRT).
MATERIALS AND METHODS
Between January 2002 and December 2016, 102 patients with stage I-IVB primary BOT cancer underwent either definitive RT (n=46) or SRT (n=56), and treatment outcomes were compared between two groups. The expression of p16 was also analyzed.
RESULTS
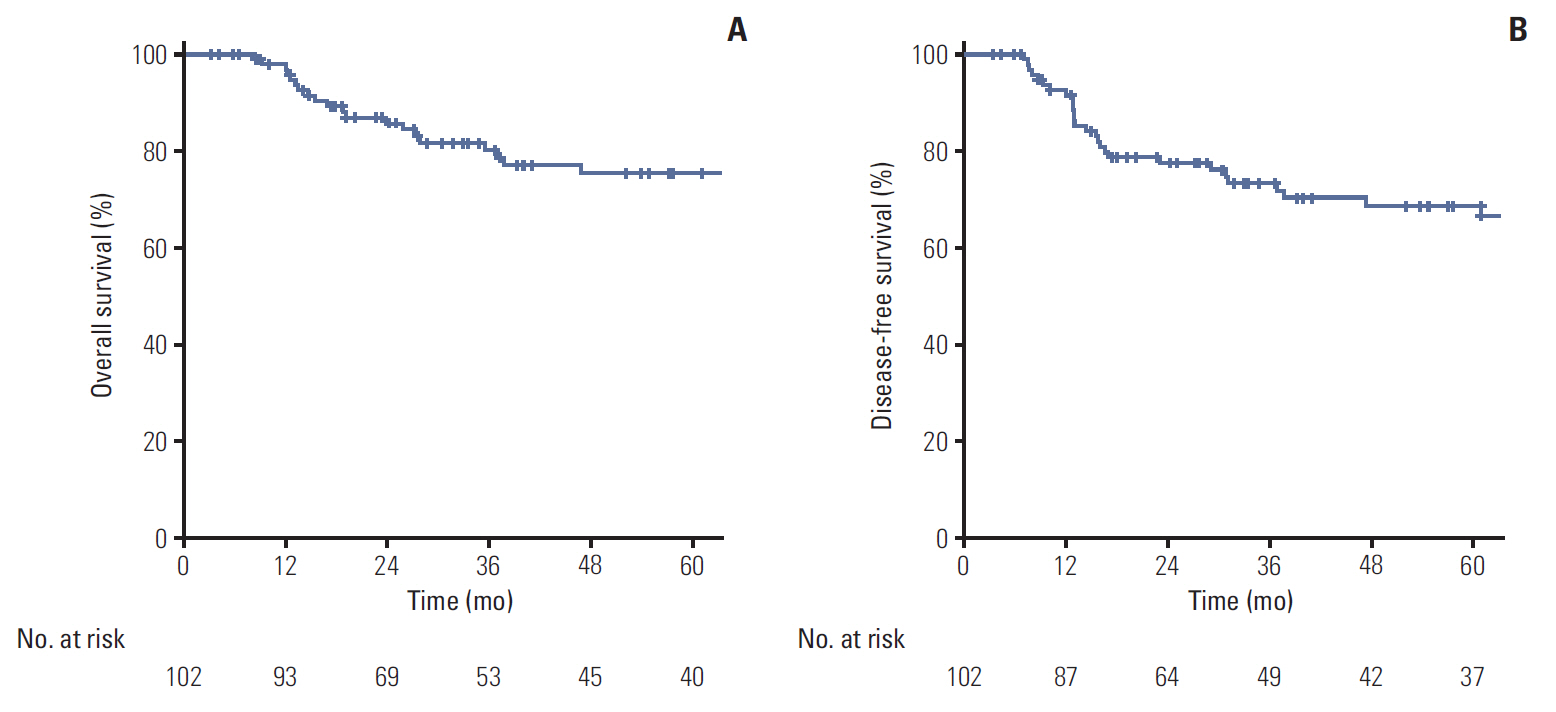
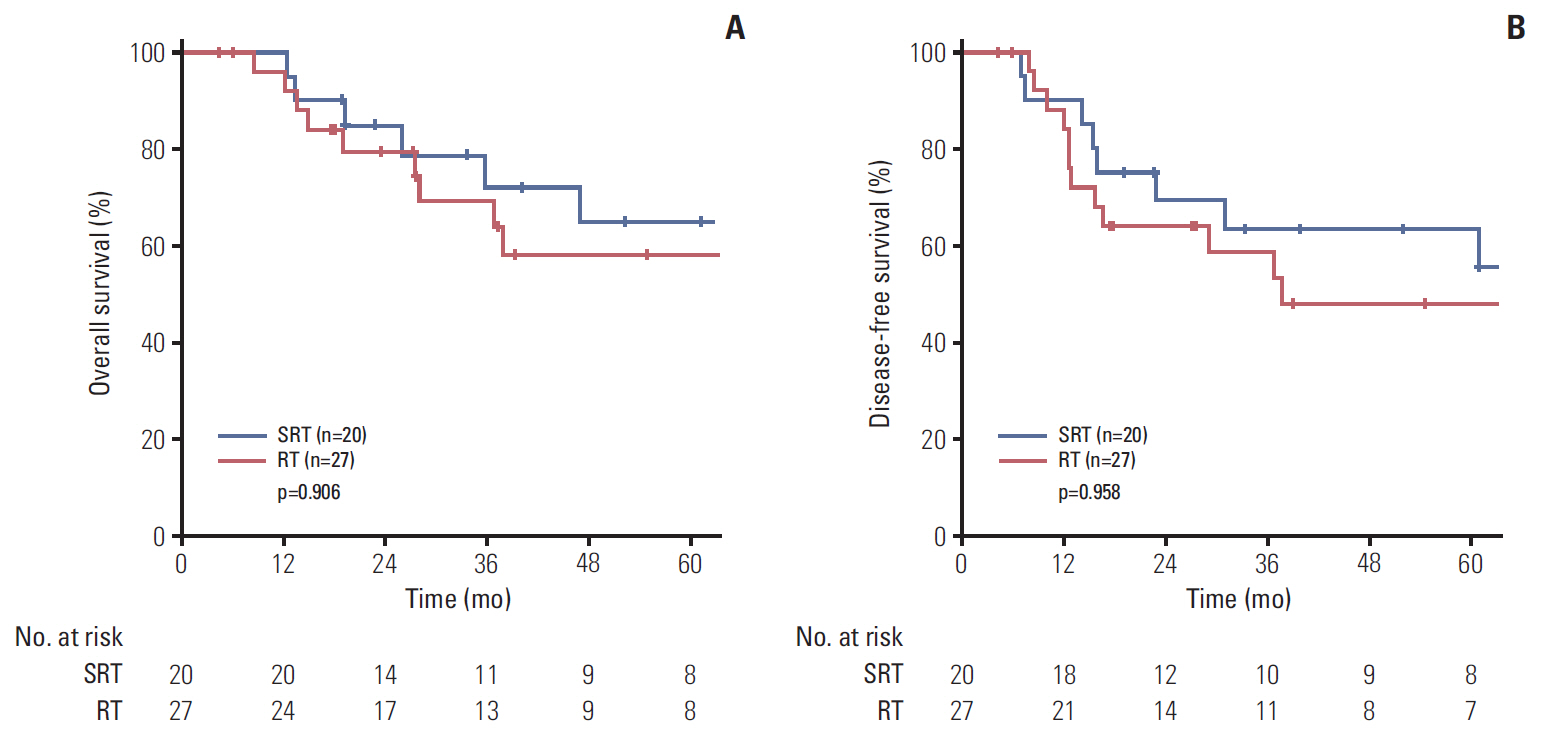
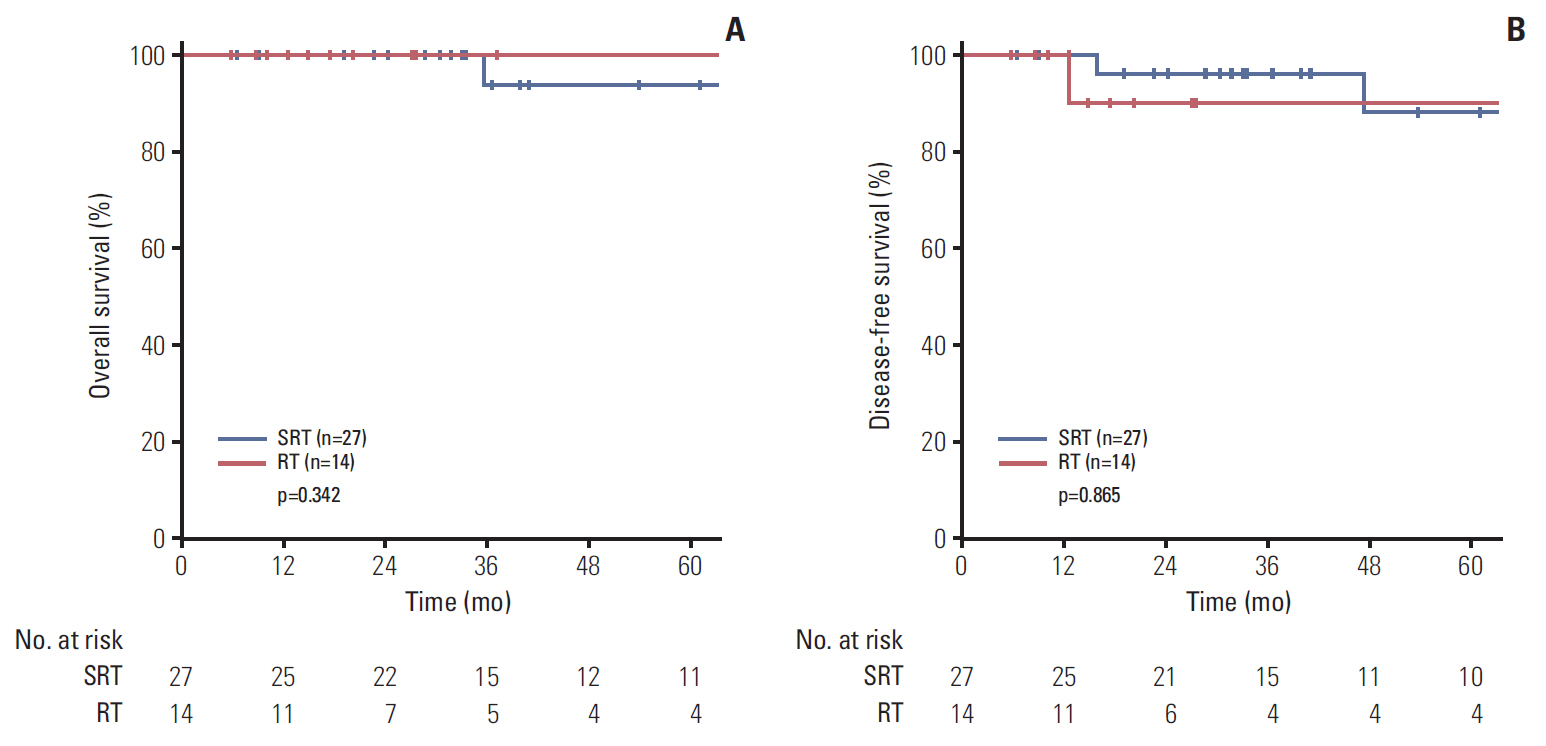
The RT group had more patients with advanced T stage (T3-4) disease (58.7% vs. 35.7%, p=0.021) and who received chemotherapy (91.3% vs. 37.5%, p < 0.001) than the SRT group. At a median follow up of 36.9 months (range, 3.3 to 181.5 months), the 5-year overall survival (OS) and disease-free survival (DFS) were 75.5% and 68.7%, respectively. With respect to treatment group, the 5-year OS and DFS in the RT and SRT groups did not differ significantly (OS, 68.7% vs. 80.5%, p=0.601; DFS, 63.1% vs. 73.1%, p=0.653). In multivariate analysis, OS differed significantly according to p16 expression (p16-negative vs. p16-positive; hazard ratio [HR], 0.145; 95% confidence interval [CI], 0.025 to 0.853; p=0.033). Regarding DFS, p16 expression (p16-negative vs. p16-positive; HR, 0.164; 95% CI, 0.045 to 0.598; p=0.006) showed a significant effect in multivariate analysis. Functional defects (late grade ≥ 3 dysphagia or voice alteration) were more frequently reported in the SRT than in the RT group (16.1% vs. 2.2%, p=0.021).
CONCLUSION
Despite advanced disease, patients in the RT group showed comparable survival outcomes and better functional preservation than those in the SRT group.
MeSH Terms
Figure
Reference
-
References
1. Karakoyun-Celik O, Norris CM Jr, Tishler R, Mahadevan A, Clark JR, Goldberg S, et al. Definitive radiotherapy with interstitial implant boost for squamous cell carcinoma of the tongue base. Head Neck. 2005; 27:353–61.
Article2. Sessions DG, Lenox J, Spector GJ, Chao C, Chaudry OA. Analysis of treatment results for base of tongue cancer. Laryngoscope. 2003; 113:1252–61.
Article3. Machtay M, Perch S, Markiewicz D, Thaler E, Chalian A, Goldberg A, et al. Combined surgery and postoperative radiotherapy for carcinoma of the base of radiotherapy for carcinoma of the base of tongue: analysis of treatment outcome and prognostic value of margin status. Head Neck. 1997; 19:494–9.4. Fein DA, Lee WR, Amos WR, Hinerman RW, Parsons JT, Mendenhall WM, et al. Oropharyngeal carcinoma treated with radiotherapy: a 30-year experience. Int J Radiat Oncol Biol Phys. 1996; 34:289–96.
Article5. Lorincz BB, Jowett N, Knecht R. Decision management in transoral robotic surgery: Indications, individual patient selection, and role in the multidisciplinary treatment for head and neck cancer from a European perspective. Head Neck. 2016; 38 Suppl 1:E2190–6.
Article6. Kerr P, Myers CL, Butler J, Alessa M, Lambert P, Cooke AL. Prospective functional outcomes in sequential population based cohorts of stage III/ IV oropharyngeal carcinoma patients treated with 3D conformal vs. intensity modulated radiotherapy. J Otolaryngol Head Neck Surg. 2015; 44:17.
Article7. Mydlarz WK, Chan JY, Richmon JD. The role of surgery for HPV-associated head and neck cancer. Oral Oncol. 2015; 51:305–13.
Article8. Attner P, Du J, Nasman A, Hammarstedt L, Ramqvist T, Lindholm J, et al. The role of human papillomavirus in the increased incidence of base of tongue cancer. Int J Cancer. 2010; 126:2879–84.
Article9. Kanakamedala M, Giri S, Hamilton RD, Vijayakumar S. Outcome analysis of squamous cell carcinomas of oropharynx based on primary site that were treated with definitive intensity modulated radiation therapy concurrently with chemotherapy. Int J Radiat Oncol Biol Phys. 2016; 96:Abstr.
Article10. Mendenhall WM, Stringer SP, Amdur RJ, Hinerman RW, Moore-Higgs GJ, Cassisi NJ. Is radiation therapy a preferred alternative to surgery for squamous cell carcinoma of the base of tongue? J Clin Oncol. 2000; 18:35–42.11. Parsons JT, Mendenhall WM, Stringer SP, Amdur RJ, Hinerman RW, Villaret DB, et al. Squamous cell carcinoma of the oropharynx: surgery, radiation therapy, or both. Cancer. 2002; 94:2967–80.12. Mendenhall WM, Morris CG, Amdur RJ, Hinerman RW, Werning JW, Villaret DB. Definitive radiotherapy for squamous cell carcinoma of the base of tongue. Am J Clin Oncol. 2006; 29:32–9.
Article13. Brunin F, Mosseri V, Jaulerry C, Point D, Cosset JM, Rodriguez J. Cancer of the base of the tongue: past and future. Head Neck. 1999; 21:751–9.
Article14. Denis F, Garaud P, Bardet E, Alfonsi M, Sire C, Germain T, et al. Final results of the 94-01 French Head and Neck Oncology and Radiotherapy Group randomized trial comparing radiotherapy alone with concomitant radiochemotherapy in advanced-stage oropharynx carcinoma. J Clin Oncol. 2004; 22:69–76.
Article15. Hinerman RW, Parsons JT, Mendenhall WM, Stringer SP, Cassisi NJ, Million RR. External beam irradiation alone or combined with neck dissection for base of tongue carcinoma: an alternative to primary surgery. Laryngoscope. 1994; 104:1466–70.16. Lawson JD, Otto K, Chen A, Shin DM, Davis L, Johnstone PA. Concurrent platinum-based chemotherapy and simultaneous modulated accelerated radiation therapy for locally advanced squamous cell carcinoma of the tongue base. Head Neck. 2008; 30:327–35.
Article17. Steiner W, Fierek O, Ambrosch P, Hommerich CP, Kron M. Transoral laser microsurgery for squamous cell carcinoma of the base of the tongue. Arch Otolaryngol Head Neck Surg. 2003; 129:36–43.
Article18. van Loon JW, Smeele LE, Hilgers FJ, van den Brekel MW. Outcome of transoral robotic surgery for stage I-II oropharyngeal cancer. Eur Arch Otorhinolaryngol. 2015; 272:175–83.
Article19. Shi A, Zhu G, Wu H, Yu R, Li F, Xu B. Analysis of clinical and dosimetric factors associated with severe acute radiation pneumonitis in patients with locally advanced non-small cell lung cancer treated with concurrent chemotherapy and intensity-modulated radiotherapy. Radiat Oncol. 2010; 5:35.
Article20. Marur S, D'Souza G, Westra WH, Forastiere AA. HPV-associated head and neck cancer: a virus-related cancer epidemic. Lancet Oncol. 2010; 11:781–9.
Article21. Reimers N, Kasper HU, Weissenborn SJ, Stutzer H, Preuss SF, Hoffmann TK, et al. Combined analysis of HPV-DNA, p16 and EGFR expression to predict prognosis in oropharyngeal cancer. Int J Cancer. 2007; 120:1731–8.
Article22. Pytynia KB, Dahlstrom KR, Sturgis EM. Epidemiology of HPV-associated oropharyngeal cancer. Oral Oncol. 2014; 50:380–6.
Article23. Licitra L, Perrone F, Bossi P, Suardi S, Mariani L, Artusi R, et al. High-risk human papillomavirus affects prognosis in patients with surgically treated oropharyngeal squamous cell carcinoma. J Clin Oncol. 2006; 24:5630–6.
Article24. Fischer CA, Zlobec I, Green E, Probst S, Storck C, Lugli A, et al. Is the improved prognosis of p16 positive oropharyngeal squamous cell carcinoma dependent of the treatment modality? Int J Cancer. 2010; 126:1256–62.
Article25. Peltenburg LT. Radiosensitivity of tumor cells: oncogenes and apoptosis. Q J Nucl Med. 2000; 44:355–64.26. Adelstein DJ, Li Y, Adams GL, Wagner H Jr, Kish JA, Ensley JF, et al. An intergroup phase III comparison of standard radiation therapy and two schedules of concurrent chemoradiotherapy in patients with unresectable squamous cell head and neck cancer. J Clin Oncol. 2003; 21:92–8.
Article27. Forastiere AA, Goepfert H, Maor M, Pajak TF, Weber R, Morrison W, et al. Concurrent chemotherapy and radiotherapy for organ preservation in advanced laryngeal cancer. N Engl J Med. 2003; 349:2091–8.
Article28. Cooper JS, Pajak TF, Forastiere AA, Jacobs J, Campbell BH, Saxman SB, et al. Postoperative concurrent radiotherapy and chemotherapy for high-risk squamous-cell carcinoma of the head and neck. N Engl J Med. 2004; 350:1937–44.
Article29. Bernier J, Domenge C, Ozsahin M, Matuszewska K, Lefebvre JL, Greiner RH, et al. Postoperative irradiation with or without concomitant chemotherapy for locally advanced head and neck cancer. N Engl J Med. 2004; 350:1945–52.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Radiation Therapy in Pancreatic Cancer
- Short-course hypofractionated radiochemotherapy for unresectable locally advanced cancer of the base of tongue: palliation only? A case report and short review of the literature
- Radiotherapy for prostate cancer
- Definitive Chemoradiotherapy Versus Surgery Followed by Adjuvant Radiotherapy in Resectable Stage III/IV Hypopharyngeal Cancer
- Treatment Outcome of Locally Advanced Non-small Cell Lung Cancer