Management of Low-Risk Papillary Thyroid Cancer
- Affiliations
-
- 1Department of Endocrinology and Metabolism, Instituto Nacional de Ciencias Médicas y Nutrición Salvador Zubirán, Mexico City, Mexico.
- 2Division of Endocrinology, Diabetes, Metabolism, and Nutrition, Mayo Clinic, Rochester, MN, USA. brito.juan@mayo.edu
- 3Knowledge and Evaluation Research Unit, Mayo Clinic, Rochester, MN, USA.
- KMID: 2420485
- DOI: http://doi.org/10.3803/EnM.2018.33.2.185
Abstract
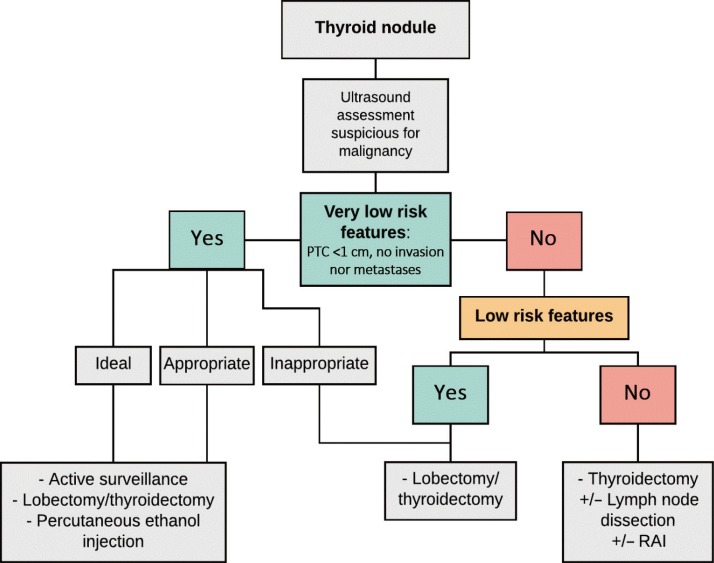
- The incidence of thyroid cancer has increased, mainly due to the incidental finding of low-risk papillary thyroid cancers (PTC). These malignancies grow slowly, and are unlikely to cause morbidity and mortality. New understanding about the prognosis of tumor features has led to reclassification of many tumors within the low-risk thyroid category, and to the development of a new one "very low-risk tumors." Alternative less aggressive approaches to therapy are now available including active surveillance and minimally invasive interventions. In this narrative review, we have summarized the available evidence for the management of low-risk PTC.
MeSH Terms
Figure
Cited by 3 articles
-
US-Guided Radiofrequency Ablation for Low-Risk Papillary Thyroid Microcarcinoma: Efficacy and Safety in a Large Population
Hyun Kyung Lim, Se Jin Cho, Jung Hwan Baek, Kang Dae Lee, Chang Woo Son, Jung Min Son, Seon Mi Baek
Korean J Radiol. 2019;20(12):1653-1661. doi: 10.3348/kjr.2019.0192.Clinical Outcomes after Early and Delayed Radioiodine Remnant Ablation in Patients with Low-Risk Papillary Thyroid Carcinoma: Propensity Score Matching Analysis
Jonghwa Ahn, Meihua Jin, Eyun Song, Min Ji Jeon, Tae Yong Kim, Jin-Sook Ryu, Won Bae Kim, Young Kee Shong, Ji Min Han, Won Gu Kim
Endocrinol Metab. 2020;35(4):830-837. doi: 10.3803/EnM.2020.747.Lactate Dehydrogenase A as a Potential New Biomarker for Thyroid Cancer
Eun Jeong Ban, Daham Kim, Jin Kyong Kim, Sang-Wook Kang, Jandee Lee, Jong Ju Jeong, Kee-Hyun Nam, Woong Youn Chung, Kunhong Kim
Endocrinol Metab. 2021;36(1):96-105. doi: 10.3803/EnM.2020.819.
Reference
-
1. Davies L, Welch HG. Current thyroid cancer trends in the United States. JAMA Otolaryngol Head Neck Surg. 2014; 140:317–322. PMID: 24557566.
Article2. Davies L, Morris LG, Haymart M, Chen AY, Goldenberg D, Morris J, et al. American Association of Clinical Endocrinologists and American College of Endocrinology disease state clinical review: the increasing incidence of thyroid cancer. Endocr Pract. 2015; 21:686–696. PMID: 26135963.
Article3. Vaccarella S, Dal Maso L, Laversanne M, Bray F, Plummer M, Franceschi S. The impact of diagnostic changes on the rise in thyroid cancer incidence: a population-based study in selected high-resource countries. Thyroid. 2015; 25:1127–1136. PMID: 26133012.
Article4. Vaccarella S, Franceschi S, Bray F, Wild CP, Plummer M, Dal Maso L. Worldwide thyroid-cancer epidemic? The increasing impact of overdiagnosis. N Engl J Med. 2016; 375:614–617. PMID: 27532827.
Article5. Guth S, Theune U, Aberle J, Galach A, Bamberger CM. Very high prevalence of thyroid nodules detected by high frequency (13 MHz) ultrasound examination. Eur J Clin Invest. 2009; 39:699–706. PMID: 19601965.6. Dal Maso L, Panato C, Franceschi S, Serraino D, Buzzoni C, Busco S, et al. The impact of overdiagnosis on thyroid cancer epidemic in Italy, 1998-2012. Eur J Cancer. 2018; 94:6–15. PMID: 29502036.7. Haugen BR, Alexander EK, Bible KC, Doherty GM, Mandel SJ, Nikiforov YE, et al. 2015 American Thyroid Association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: the American Thyroid Association guidelines task force on thyroid nodules and differentiated thyroid cancer. Thyroid. 2016; 26:1–133. PMID: 26462967.
Article8. Tarasova VD, Tuttle RM. Current management of low risk differentiated thyroid cancer and papillary microcarcinoma. Clin Oncol (R Coll Radiol). 2017; 29:290–297. PMID: 28087101.
Article9. Tuttle RM, Haugen B, Perrier ND. Updated American Joint Committee on cancer/tumor-node-metastasis staging system for differentiated and anaplastic thyroid cancer (eighth edition): what changed and why? Thyroid. 2017; 27:751–756. PMID: 28463585.
Article10. Arora N, Turbendian HK, Scognamiglio T, Wagner PL, Goldsmith SJ, Zarnegar R, et al. Extrathyroidal extension is not all equal: implications of macroscopic versus microscopic extent in papillary thyroid carcinoma. Surgery. 2008; 144:942–947. PMID: 19041001.
Article11. Hay ID, Johnson TR, Thompson GB, Sebo TJ, Reinalda MS. Minimal extrathyroid extension in papillary thyroid carcinoma does not result in increased rates of either cause-specific mortality or postoperative tumor recurrence. Surgery. 2016; 159:11–19. PMID: 26514317.
Article12. Jin BJ, Kim MK, Ji YB, Song CM, Park JH, Tae K. Characteristics and significance of minimal and maximal extrathyroidal extension in papillary thyroid carcinoma. Oral Oncol. 2015; 51:759–763. PMID: 26093388.
Article13. Nixon IJ, Ganly I, Patel S, Palmer FL, Whitcher MM, Tuttle RM, et al. The impact of microscopic extrathyroid extension on outcome in patients with clinical T1 and T2 well-differentiated thyroid cancer. Surgery. 2011; 150:1242–1249. PMID: 22136847.
Article14. Nikiforov YE, Seethala RR, Tallini G, Baloch ZW, Basolo F, Thompson LD, et al. Nomenclature revision for encapsulated follicular variant of papillary thyroid carcinoma: a paradigm shift to reduce overtreatment of indolent tumors. JAMA Oncol. 2016; 2:1023–1029. PMID: 27078145.15. Hodak S, Tuttle RM, Maytal G, Nikiforov YE, Randolph G. Changing the cancer diagnosis: the case of follicular variant of papillary thyroid cancer-primum non nocere and NIFTP. Thyroid. 2016; 26:869–871. PMID: 27184034.
Article16. Thompson LD. Ninety-four cases of encapsulated follicular variant of papillary thyroid carcinoma: a name change to noninvasive follicular thyroid neoplasm with papillary-like nuclear features would help prevent overtreatment. Mod Pathol. 2016; 29:698–707. PMID: 27102347.
Article17. Xu B, Tallini G, Ghossein RA. Noninvasive follicular thyroid neoplasm with papillary-like nuclear features: historical context, diagnosis, and future challenges. Endocr Pathol. 2017; 28:128–138. PMID: 28361392.18. Xu B, Tallini G, Scognamiglio T, Roman BR, Tuttle RM, Ghossein RA. Outcome of large noninvasive follicular thyroid neoplasm with papillary-like nuclear features. Thyroid. 2017; 27:512–517. PMID: 28136139.
Article19. Lloyd RV, Asa SL, LiVolsi VA, Sadow PM, Tischler AS, Ghossein RA, et al. The evolving diagnosis of noninvasive follicular thyroid neoplasm with papillary-like nuclear features (NIFTP). Hum Pathol. 2018; 74:1–4. PMID: 29339178.
Article20. American Thyroid Association (ATA) Guidelines Taskforce on Thyroid Nodules and Differentiated Thyroid Cancer. Cooper DS, Doherty GM, Haugen BR, Kloos RT, Lee SL, et al. Revised American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid. 2009; 19:1167–1214. PMID: 19860577.
Article21. Miyauchi A, Ito Y, Oda H. Insights into the management of papillary microcarcinoma of the thyroid. Thyroid. 2018; 28:23–31. PMID: 28629253.
Article22. Ito Y, Miyauchi A, Kihara M, Higashiyama T, Kobayashi K, Miya A. Patient age is significantly related to the progression of papillary microcarcinoma of the thyroid under observation. Thyroid. 2014; 24:27–34. PMID: 24001104.
Article23. Ito Y, Kudo T, Kobayashi K, Miya A, Ichihara K, Miyauchi A. Prognostic factors for recurrence of papillary thyroid carcinoma in the lymph nodes, lung, and bone: analysis of 5,768 patients with average 10-year follow-up. World J Surg. 2012; 36:1274–1278. PMID: 22270990.
Article24. Sugitani I, Toda K, Yamada K, Yamamoto N, Ikenaga M, Fujimoto Y. Three distinctly different kinds of papillary thyroid microcarcinoma should be recognized: our treatment strategies and outcomes. World J Surg. 2010; 34:1222–1231. PMID: 20066418.
Article25. Ito Y, Uruno T, Nakano K, Takamura Y, Miya A, Kobayashi K, et al. An observation trial without surgical treatment in patients with papillary microcarcinoma of the thyroid. Thyroid. 2003; 13:381–387. PMID: 12804106.
Article26. Ito Y, Miyauchi A, Inoue H, Fukushima M, Kihara M, Higashiyama T, et al. An observational trial for papillary thyroid microcarcinoma in Japanese patients. World J Surg. 2010; 34:28–35. PMID: 20020290.
Article27. Brito JP, Ito Y, Miyauchi A, Tuttle RM. A clinical framework to facilitate risk stratification when considering an active surveillance alternative to immediate biopsy and surgery in papillary microcarcinoma. Thyroid. 2016; 26:144–149. PMID: 26414743.
Article28. Tuttle RM, Fagin JA, Minkowitz G, Wong RJ, Roman B, Patel S, et al. Natural history and tumor volume kinetics of papillary thyroid cancers during active surveillance. JAMA Otolaryngol Head Neck Surg. 2017; 143:1015–1020. PMID: 28859191.
Article29. Nixon IJ, Ganly I, Patel SG, Palmer FL, Whitcher MM, Tuttle RM, et al. Thyroid lobectomy for treatment of well differentiated intrathyroid malignancy. Surgery. 2012; 151:571–579. PMID: 22001636.
Article30. Matsuzu K, Sugino K, Masudo K, Nagahama M, Kitagawa W, Shibuya H, et al. Thyroid lobectomy for papillary thyroid cancer: long-term follow-up study of 1,088 cases. World J Surg. 2014; 38:68–79. PMID: 24081532.
Article31. Dionigi G, Chai YJ, Tufano RP, Anuwong A, Kim HY. Transoral endoscopic thyroidectomy via a vestibular approach: why and how? Endocrine. 2018; 59:275–279. PMID: 29039144.
Article32. Adam MA, Thomas S, Youngwirth L, Hyslop T, Reed SD, Scheri RP, et al. Is there a minimum number of thyroidectomies a surgeon should perform to optimize patient outcomes? Ann Surg. 2017; 265:402–407. PMID: 28059969.
Article33. Al-Qurayshi Z, Robins R, Hauch A, Randolph GW, Kandil E. Association of surgeon volume with outcomes and cost savings following thyroidectomy: a national forecast. JAMA Otolaryngol Head Neck Surg. 2016; 142:32–39. PMID: 26561736.34. Youngwirth LM, Adam MA, Scheri RP, Roman SA, Sosa JA. Patients treated at low-volume centers have higher rates of incomplete resection and compromised outcomes: analysis of 31,129 patients with papillary thyroid cancer. Ann Surg Oncol. 2016; 23:403–409. PMID: 26416710.
Article35. Farkas EA, King TA, Bolton JS, Fuhrman GM. A comparison of total thyroidectomy and lobectomy in the treatment of dominant thyroid nodules. Am Surg. 2002; 68:678–682. PMID: 12206601.36. Mancino AT, Kim LT. Chapter 17, Role of radioactive iodine for remnant ablation in patients with papillary thyroid cancer. Management of differentiated thyroid cancer. Cham: Springer;2017. p. 205–222.37. Dean DS, Hay ID. Prognostic indicators in differentiated thyroid carcinoma. Cancer Control. 2000; 7:229–239. PMID: 10832109.
Article38. Hay ID, Bergstralh EJ, Goellner JR, Ebersold JR, Grant CS. Predicting outcome in papillary thyroid carcinoma: development of a reliable prognostic scoring system in a cohort of 1,779 patients surgically treated at one institution during 1940 through 1989. Surgery. 1993; 114:1050–1057. PMID: 8256208.39. Hay ID. Management of patients with low-risk papillary thyroid carcinoma. Endocr Pract. 2007; 13:521–533. PMID: 17872355.
Article40. Lamartina L, Durante C, Filetti S, Cooper DS. Low-risk differentiated thyroid cancer and radioiodine remnant ablation: a systematic review of the literature. J Clin Endocrinol Metab. 2015; 100:1748–1761. PMID: 25679996.
Article41. Sacks W, Fung CH, Chang JT, Waxman A, Braunstein GD. The effectiveness of radioactive iodine for treatment of low-risk thyroid cancer: a systematic analysis of the peer-reviewed literature from 1966 to April 2008. Thyroid. 2010; 20:1235–1245. PMID: 21062195.
Article42. Janovsky CC, Maciel RM, Camacho CP, Padovani RP, Nakabashi CC, Yang JH, et al. A prospective study showing an excellent response of patients with low-risk differentiated thyroid cancer who did not undergo radioiodine remnant ablation after total thyroidectomy. Eur Thyroid J. 2016; 5:44–49. PMID: 27099838.
Article43. Hay ID, Lee R, Morris J, Stan M, Castro M, Fatourechi V, et al. Ultrasound-guided percutaneous ethanol ablation for selected patients with papillary thyroid microcarcinoma: a novel, effective and well tolerated alternative to neck surgery or observation. In : 87th Annual Meeting of the American Thyroid Association; 2017 Oct 18–22; Victoria, BC.44. Gazelle GS, Goldberg SN, Solbiati L, Livraghi T. Tumor ablation with radio-frequency energy. Radiology. 2000; 217:633–646. PMID: 11110923.
Article45. Cervelli R, Mazzeo S, De Napoli L, Boccuzzi A, Pontillo-Contillo B, Materazzi G, et al. Radiofrequency ablation in the treatment of benign thyroid nodules: an efficient and safe alternative to surgery. J Vasc Interv Radiol. 2017; 28:1400–1408. PMID: 28844832.
Article46. Cheng Z, Che Y, Yu S, Wang S, Teng D, Xu H, et al. US-guided percutaneous radiofrequency versus microwave ablation for benign thyroid nodules: a prospective multicenter study. Sci Rep. 2017; 7:9554. PMID: 28842651.
Article47. Radzina M, Cantisani V, Rauda M, Nielsen MB, Ewertsen C, D'Ambrosio F, et al. Update on the role of ultrasound guided radiofrequency ablation for thyroid nodule treatment. Int J Surg. 2017; 41(Suppl 1):S82–S93. PMID: 28506420.
Article48. Cesareo R, Palermo A, Pasqualini V, Cianni R, Gaspa G, Manfrini S, et al. Radiofrequency ablation for the management of thyroid nodules: a critical appraisal of the literature. Clin Endocrinol (Oxf). 2017; 87:639–648. PMID: 28718950.
Article49. Zhao Q, Tian G, Kong D, Jiang T. Meta-analysis of radiofrequency ablation for treating the local recurrence of thyroid cancers. J Endocrinol Invest. 2016; 39:909–916. PMID: 26980591.
Article50. Jeong SY, Baek JH, Choi YJ, Chung SR, Sung TY, Kim WG, et al. Radiofrequency ablation of primary thyroid carcinoma: efficacy according to the types of thyroid carcinoma. Int J Hyperthermia. 2018; 1. 24. [Epub]. DOI: 10.1080/02656736.2018.1427288.
Article51. Sun J, Liu X, Zhang Q, Hong Y, Song B, Teng X, et al. Papillary thyroid carcinoma treated with radiofrequency ablation in a patient with hypertrophic cardiomyopathy: a case report. Korean J Radiol. 2016; 17:558–561. PMID: 27390548.
Article52. Zhang M, Luo Y, Zhang Y, Tang J. Efficacy and safety of ultrasound-guided radiofrequency ablation for treating low-risk papillary thyroid microcarcinoma: a prospective study. Thyroid. 2016; 26:1581–1587. PMID: 27445090.
Article53. Papini E, Guglielmi R, Gharib H, Misischi I, Graziano F, Chianelli M, et al. Ultrasound-guided laser ablation of incidental papillary thyroid microcarcinoma: a potential therapeutic approach in patients at surgical risk. Thyroid. 2011; 21:917–920. PMID: 21595556.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Review of Active Surveillance of Papillary Thyroid Microcarcinoma
- A Closer Look at Papillary Thyroid Carcinoma
- Active Surveillance as an Effective Management Option for Low-Risk Papillary Thyroid Microcarcinoma
- Study Protocol of Expanded Multicenter Prospective Cohort Study of Active Surveillance on Papillary Thyroid Microcarcinoma (MAeSTro-EXP)
- Current Guidelines for Fine Needle Aspiration of Thyroid Nodules