Ann Rehabil Med.
2018 Aug;42(4):560-568. 10.5535/arm.2018.42.4.560.
Association of Brain Lesions and Videofluoroscopic Dysphagia Scale Parameters on Patients With Acute Cerebral Infarctions
- Affiliations
-
- 1Department of Rehabilitation Medicine, Dong-Eui Medical Center, Busan, Korea.
- 2Department of Physical Medicine and Rehabilitation, Kosin University College of Medicine, Busan, Korea. jhjpmr@naver.com
- KMID: 2420048
- DOI: http://doi.org/10.5535/arm.2018.42.4.560
Abstract
OBJECTIVE
To investigate the characteristics and risk factors of dysphagia using the videofluoroscopic dysphagia scale (VDS) with a videofluoroscopic swallowing study (VFSS) in patients with acute cerebral infarctions.
METHODS
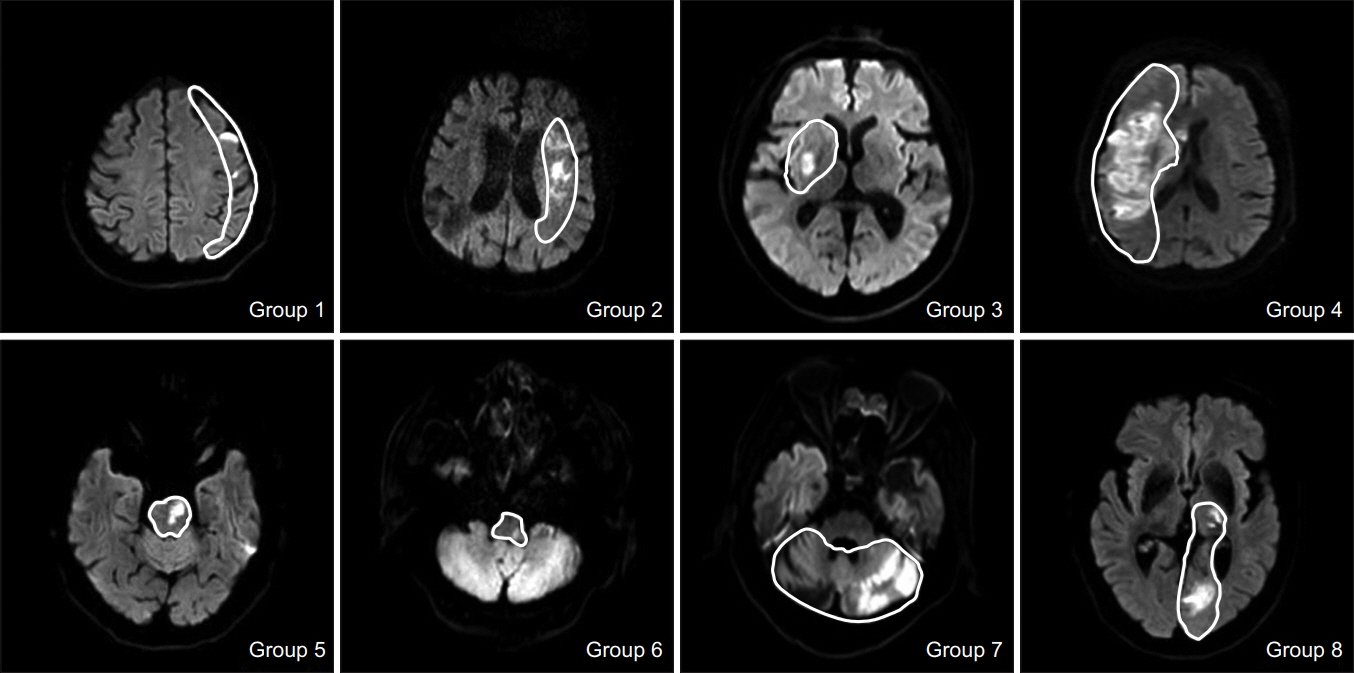
In this retrospective study, the baseline VFSS in 275 stroke patients was analyzed. We divided patients into 8 groups according to lesion areas commonly observed on brain magnetic resonance imaging. Dysphagia characteristics and severity were evaluated using the VDS. We also analyzed the relationship between clinical and functional parameters based on medical records and VDS scores.
RESULTS
In comparison studies of lesions associated with swallowing dysfunction, several groups with significant differences were identified. Apraxia was more closely associated with cortical middle cerebral artery territory lesions. Vallecular and pyriform sinus residue was more common with lesions in the medulla or pons. In addition, the results for the Korean version of the Modified Barthel Index (K-MBI), a functional assessment tool, corresponded to those in the quantitative evaluation of swallowing dysfunctions.
CONCLUSION
A large cohort of patients with cerebral infarction was evaluated to determine the association between brain lesions and swallowing dysfunction. The results can be used to establish a specific treatment plan. In addition, the characteristic factors associated with swallowing dysfunctions were also confirmed.
MeSH Terms
Figure
Cited by 1 articles
-
Correlation of Swallowing Function With Bilateral Diaphragmatic Movement in Hemiplegic Stroke Patients
Ra Yu Yun, Ho Eun Park, Ji Won Hong, Yong Beom Shin, Jin A Yoon
Ann Rehabil Med. 2019;43(2):156-162. doi: 10.5535/arm.2019.43.2.156.
Reference
-
1. Martino R, Foley N, Bhogal S, Diamant N, Speechley M, Teasell R. Dysphagia after stroke: incidence, diagnosis, and pulmonary complications. Stroke. 2005; 36:2756–63.2. Han TR, Paik NJ, Park JW, Kwon BS. The prediction of persistent dysphagia beyond six months after stroke. Dysphagia. 2008; 23:59–64.
Article3. Han H, Shin G, Jun A, Park T, Ko D, Choi E, et al. The relation between the presence of aspiration or penetration and the clinical indicators of dysphagia in poststroke survivors. Ann Rehabil Med. 2016; 40:88–94.
Article4. Suntrup S, Kemmling A, Warnecke T, Hamacher C, Oelenberg S, Niederstadt T, et al. The impact of lesion location on dysphagia incidence, pattern and complications in acute stroke. Part 1: dysphagia incidence, severity and aspiration. Eur J Neurol. 2015; 22:832–8.
Article5. Steinhagen V, Grossmann A, Benecke R, Walter U. Swallowing disturbance pattern relates to brain lesion location in acute stroke patients. Stroke. 2009; 40:1903–6.
Article6. Kim DK. Post-stroke dysphagia: incidence, complications and pattern relates to brain lesion. Brain Neurorehabil. 2009; 2:91–7.
Article7. Lee CK, Kim JA. Pattern of post-stroke swallowing disorder according to the brain lesion. J Korean Acad Rehabil Med. 2001; 25:193–201.8. Dehaghani SE, Yadegari F, Asgari A, Chitsaz A, Karami M. Brain regions involved in swallowing: Evidence from stroke patients in a cross-sectional study. J Res Med Sci. 2016; 21:45.
Article9. Jeon WH, Park GW, Lee JH, Jeong HJ, Sim YJ. Association between location of brain lesion and clinical factors and findings of videofluoroscopic swallowing study in subacute stroke patients. Brain Neurorehabil. 2014; 7:54–60.
Article10. Kim BR, Moon WJ, Kim H, Jung E, Lee J. Association of dysphagia with supratentorial lesions in patients with middle cerebral artery stroke. Ann Rehabil Med. 2016; 40:637–46.
Article11. Jang S, Yang HE, Yang HS, Kim DH. Lesion characteristics of chronic dysphagia in patients with supratentorial stroke. Ann Rehabil Med. 2017; 41:225–30.
Article12. Moon HI, Pyun SB, Kwon HK. Correlation between location of brain lesion and cognitive function and findings of videofluoroscopic swallowing study. Ann Rehabil Med. 2012; 36:347–55.
Article13. Logemann JA. Evaluation and treatment of swallowing disorders. 2nd ed. Austin: Pro-Ed;1998.14. Michou E, Hamdy S. Cortical input in control of swallowing. Curr Opin Otolaryngol Head Neck Surg. 2009; 17:166–71.
Article15. Hamdy S, Mikulis DJ, Crawley A, Xue S, Lau H, Henry S, et al. Cortical activation during human volitional swallowing: an event-related fMRI study. Am J Physiol. 1999; 277:G219–25.16. DePippo KL, Holas MA, Reding MJ. The Burke dysphagia screening test: validation of its use in patients with stroke. Arch Phys Med Rehabil. 1994; 75:1284–6.
Article17. Gottlieb D, Kipnis M, Sister E, Vardi Y, Brill S. Validation of the 50 ml3 drinking test for evaluation of poststroke dysphagia. Disabil Rehabil. 1996; 18:529–32.18. Chua KS, Kong KH. Functional outcome in brain stem stroke patients after rehabilitation. Arch Phys Med Rehabil. 1996; 77:194–7.
Article19. Falsetti P, Acciai C, Palilla R, Bosi M, Carpinteri F, Zingarelli A, et al. Oropharyngeal dysphagia after stroke: incidence, diagnosis, and clinical predictors in patients admitted to a neurorehabilitation unit. J Stroke Cerebrovasc Dis. 2009; 18:329–35.
Article20. Langdon PC, Lee AH, Binns CW. Dysphagia in acute ischaemic stroke: severity, recovery and relationship to stroke subtype. J Clin Neurosci. 2007; 14:630–4.
Article21. Broadley S, Croser D, Cottrell J, Creevy M, Teo E, Yiu D, et al. Predictors of prolonged dysphagia following acute stroke. J Clin Neurosci. 2003; 10:300–5.
Article22. Paciaroni M, Mazzotta G, Corea F, Caso V, Venti M, Milia P, et al. Dysphagia following Stroke. Eur Neurol. 2004; 51:162–7.
Article23. Leonard R, Kendall K. Dysphagia assessment and treatment planning. 2nd ed. San Diego: Plural Publishing;2008. p. 1–34.24. Daniels SK, Foundas AL. Lesion localization in acute stroke patients with risk of aspiration. J Neuroimaging. 1999; 9:91–8.25. Robbins J, Levine RL, Maser A, Rosenbek JC, Kempster GB. Swallowing after unilateral stroke of the cerebral cortex. Arch Phys Med Rehabil. 1993; 74:1295–300.
Article26. Broadley S, Cheek A, Salonikis S, Whitham E, Chong V, Cardone D, et al. Predicting prolonged dysphagia in acute stroke: the Royal Adelaide Prognostic Index for Dysphagic Stroke (RAPIDS). Dysphagia. 2005; 20:303–10.
Article27. Toscano M, Cecconi E, Capiluppi E, Vigano A, Bertora P, Campiglio L, et al. Neuroanatomical, clinical and cognitive correlates of post-stroke dysphagia. Eur Neurol. 2015; 74:171–7.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Validity of the Functional Dysphagia Scale Based on Videofluoroscopic Swallowing Study
- Dysphagia in Traumatic Brain Injured Patients
- Scoring System in Videofluoroscopic Swallowing Study
- Comparison of Swallowing Functions Between Brain Tumor and Stroke Patients
- Dysphagia Pattern according to Stroke Location