J Bone Metab.
2018 Aug;25(3):175-180. 10.11005/jbm.2018.25.3.175.
Regional Distribution of Stress on the Distal Femur in Advanced Osteoarthritis
- Affiliations
-
- 1Department of Orthopedic Surgery, Konyang University College of Medicine, Daejeon, Korea. kimajouos@gmail.com
- KMID: 2419845
- DOI: http://doi.org/10.11005/jbm.2018.25.3.175
Abstract
- BACKGROUND
The aim of this study was to analyze regional differences in the stress distribution within the distal femur in advanced osteoarthritis (OA).
METHODS
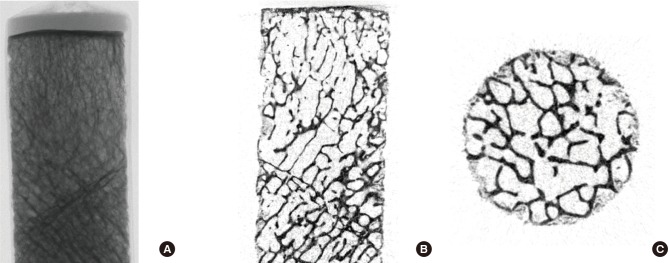
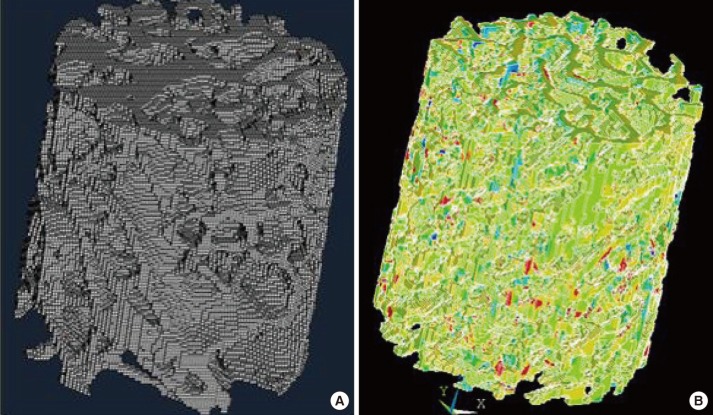
Distal femoral specimens with primary OA were obtained from 10 female donor cadavers (mean age, 65 years; range, 53-79). As controls, distal femurs without OA were obtained from 10 age- and sex-matched female cadavers (mean age, 67 years; range, 58-81). The articular surface of the distal femur was divided into anterior, middle, and posterior regions on each condyle. Mechanical properties and microstructure were assessed for each region with micro-computed tomography and finite element model analysis.
RESULTS
The control group showed differences in stress distribution among 6 regions on the distal femur (P=0.037), but there was no regional difference in stress distribution among 6 regions on the distal femur in the advanced OA group (P=0.179).
CONCLUSIONS
Regional stress distribution in the distal femur was different between advanced OA and normal groups. There were no regional differences in stress distribution in the advanced OA group. Altered loading patterns, bone remodeling, and chemical composition will affect stress distribution.
Keyword
MeSH Terms
Figure
Reference
-
1. Neogi T. Clinical significance of bone changes in osteoarthritis. Ther Adv Musculoskelet Dis. 2012; 4:259–267. PMID: 22859925.
Article2. Rubin CT, Lanyon LE. Regulation of bone formation by applied dynamic loads. J Bone Joint Surg Am. 1984; 66:397–402. PMID: 6699056.
Article3. Li B, Aspden RM. Composition and mechanical properties of cancellous bone from the femoral head of patients with osteoporosis or osteoarthritis. J Bone Miner Res. 1997; 12:641–651. PMID: 9101376.
Article4. Brittberg M, Winalski CS. Evaluation of cartilage injuries and repair. J Bone Joint Surg Am. 2003; 85-A(Suppl 2):58–69.
Article5. Niebur GL, Feldstein MJ, Yuen JC, et al. High-resolution finite element models with tissue strength asymmetry accurately predict failure of trabecular bone. J Biomech. 2000; 33:1575–1583. PMID: 11006381.
Article6. Brown SJ, Pollintine P, Powell DE, et al. Regional differences in mechanical and material properties of femoral head cancellous bone in health and osteoarthritis. Calcif Tissue Int. 2002; 71:227–234. PMID: 12170373.
Article7. Ding M, Odgaard A, Hvid I. Changes in the three-dimensional microstructure of human tibial cancellous bone in early osteoarthritis. J Bone Joint Surg Br. 2003; 85:906–912. PMID: 12931817.
Article8. Boyd SK, Muller R, Matyas JR, et al. Early morphometric and anisotropic change in periarticular cancellous bone in a model of experimental knee osteoarthritis quantified using microcomputed tomography. Clin Biomech (Bristol, Avon). 2000; 15:624–631.
Article9. Ding M, Hvid I. Quantification of age-related changes in the structure model type and trabecular thickness of human tibial cancellous bone. Bone. 2000; 26:291–295. PMID: 10710004.
Article10. Kim KK, Baek MH, Won YY. Changes in the microstructural and mechanical properties in the medial condyle of human distal femur in advanced osteoarthritis. Osteoporosis. 2012; 10:61–66.11. Feldkamp LA, Goldstein SA, Parfitt AM, et al. The direct examination of three-dimensional bone architecture in vitro by computed tomography. J Bone Miner Res. 1989; 4:3–11. PMID: 2718776.
Article12. Parfitt AM, Drezner MK, Glorieux FH, et al. Bone histomorphometry: standardization of nomenclature, symbols, and units. Report of the ASBMR Histomorphometry Nomenclature Committee. J Bone Miner Res. 1987; 2:595–610. PMID: 3455637.
Article13. Chevalier F, Laval-Jeantet AM, Laval-Jeantet M, et al. CT image analysis of the vertebral trabecular network in vivo. Calcif Tissue Int. 1992; 51:8–13. PMID: 1393783.
Article14. Dempster DW, Ferguson-Pell MW, Mellish RW, et al. Relationships between bone structure in the iliac crest and bone structure and strength in the lumbar spine. Osteoporos Int. 1993; 3:90–96. PMID: 8453196.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Deformity Correction by Femoral Supracondylar Dome Osteotomy with Retrograde Intramedullary Nailing in Varus Deformity of the Distal Femur after Pathologic Fracture of Giant Cell Tumor
- Changes in the Microstructural and Mechanical Properties in the Medial Condyle of Human Distal Femur in Advanced Osteoarthritis
- Fatigue Fracture of the Distal femur Shaft: A Case Report
- Fatigue Fracture of the Distal Femur in Adolescence: A case Report
- Femoral Stress Fractures in Civilians who are not military recruits and athlethes :Two cases report