Korean J Gastroenterol.
2018 Aug;72(2):86-89. 10.4166/kjg.2018.72.2.86.
Spontaneously Resolving of Huge Simple Hepatic Cyst
- Affiliations
-
- 1Department of Internal Medicine, Gachon University Gil Medical Center, Incheon, Korea. kos@gilhospital.com
- KMID: 2418769
- DOI: http://doi.org/10.4166/kjg.2018.72.2.86
Abstract
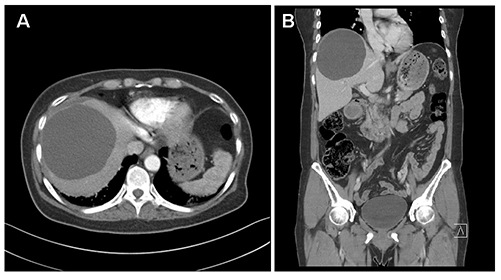
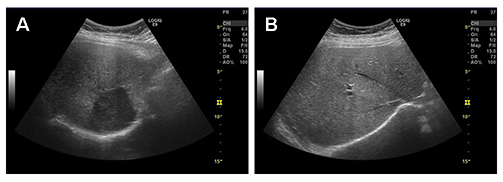
- Simple hepatic cysts are common benign liver lesions that usually have no malignant capability. They are generally asymptomatic and are often found incidentally by abdominal imaging procedures. Treatment becomes necessary, however, when huge hepatic cysts cause symptoms and develop complications, such as hemorrhage, adjacent organ damage, and infection. Several therapeutic options have been performed for symptomatic and huge cysts, including the aspiration of cystic fluid, infusion of various sclerosing agents, and surgical intervention. The optimal management of huge hepatic cysts is controversial and each option has its complications and limitations. This paper reports a case of a 66-year-old woman diagnosed with a simple hepatic cyst 2 years earlier, who was referred to hospital due to abdominal pain. The diagnosis was a huge hepatic cyst with symptoms by abdominal imaging studies. During the follow-up period, the huge cysts resolved spontaneously without treatment.
Keyword
MeSH Terms
Figure
Reference
-
1. Drenth JP, Chrispijn M, Bergmann C. Congenital fibrocystic liver diseases. Best Pract Res Clin Gastroenterol. 2010; 24:573–584.
Article2. Méndez-Sánchez N, Pichardo-Bahena R, Uribe M. Images in hepatology. Microhamartomas (Von Meyenburg Complexes). Ann Hepatol. 2003; 2:98.3. Reid-Lombardo KM, Khan S, Sclabas G. Hepatic cysts and liver abscess. Surg Clin North Am. 2010; 90:679–697.
Article4. Gaines PA, Sampson MA. The prevalence and characterization of simple hepatic cysts by ultrasound examination. Br J Radiol. 1989; 62:335–337.
Article5. Caremani M, Vincenti A, Benci A, Sassoli S, Tacconi D. Ecographic epidemiology of non-parasitic hepatic cysts. J Clin Ultrasound. 1993; 21:115–118.
Article6. Jørgensen MJ. The ductal plate malformation. Acta Pathol Microbiol Scand Suppl. 1977; (257):1–87.7. Asuquo M, Nwagbara V, Agbor C, Otobo F, Omotoso A. Giant simple hepatic cyst: a case report and review of relevant literature. Afr Health Sci. 2015; 15:293–298.
Article8. Larssen TB, Rørvik J, Hoff SR, Horn A, Rosendahl K. The occurrence of asymptomatic and symptomatic simple hepatic cysts. A prospective, hospital-based study. Clin Radiol. 2005; 60:1026–1029.
Article9. Haap M, Seeger A, Haas CS. Giant solitary hepatic cyst. Liver Int. 2008; 28:840.
Article10. Brancatelli G, Federle MP, Vilgrain V, Vullierme MP, Marin D, Lagalla R. Fibropolycystic liver disease: CT and MR imaging findings. Radiographics. 2005; 25:659–670.
Article11. Fernandez M, Cacioppo JC, Davis RP, Nora PF. Management of solitary nonparasitic liver cyst. Am Surg. 1984; 50:205–208.12. Palacios E, Shannon M, Solomon C, Guzman M. Biliary cystadenoma: ultrasound, CT, and MRI. Gastrointest Radiol. 1990; 15:313–316.
Article13. Zarzour JG, Porter KK, Tchelepi H, Robbin ML. Contrast-enhanced ultrasound of benign liver lesions. Abdom Radiol (NY). 2018; 43:848–860.
Article14. Saini S, Mueller PR, Ferrucci JT Jr, Simeone JF, Wittenberg J, Butch RJ. Percutaneous aspiration of hepatic cysts does not provide definitive therapy. AJR Am J Roentgenol. 1983; 141:559–560.
Article15. Macedo FI. Current management of noninfectious hepatic cystic lesions: a review of the literature. World J Hepatol. 2013; 5:462–469.
Article16. Lynch MJ, McLeod MK, Weatherbee L, Gilsdorf JR, Guice KS, Eckhauser FE. Squamous cell cancer of the liver arising from a solitary benign nonparasitic hepatic cyst. Am J Gastroenterol. 1988; 83:426–431.17. Hanazaki K, Wakabayashi M, Mori H, et al. Hemorrhage into a simple liver cyst: diagnostic implications of a recent case. J Gastroenterol. 1997; 32:848–851.
Article18. Salemis NS, Georgoulis E, Gourgiotis S, Tsohataridis E. Spontaneous rupture of a giant non parasitic hepatic cyst presenting as an acute surgical abdomen. Ann Hepatol. 2007; 6:190–193.19. Bourgeois N, Kinnaert P, Vereerstraeten P, Schoutens A, Toussaint C. Infection of hepatic cysts following kidney transplantation in polycystic disease. World J Surg. 1983; 7:629–631.
Article20. Arai H, Nagamine T, Suzuki H, et al. Simple liver cyst with spontaneous regression. J Gastroenterol. 2002; 37:755–757.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A huge hepatic cyst successfully treated with absolute ethano: report of a case
- Successful Alcoholic Sclerotherapy of Huge Hepatic Cyse in a Patient with Autosomal Dominant Polycystic Kidney Disease
- A Case of Huge Hepatic Cyst Treated by One-Shot Instillation of Minocycline Chloride
- Renal cell carcinoma developed in a patient treated with huge simple renal cyst sclerotherapy
- Comparison between Laparoscopic Unroofing and Open Surgery for Nonparasitic Hepatic Cyst