Korean J Radiol.
2018 Oct;19(5):1000-1005. 10.3348/kjr.2018.19.5.1000.
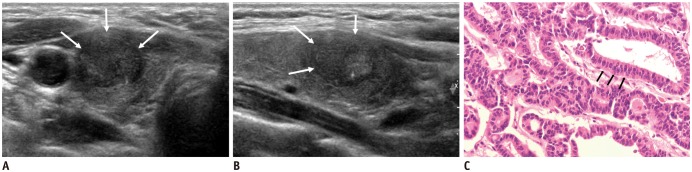
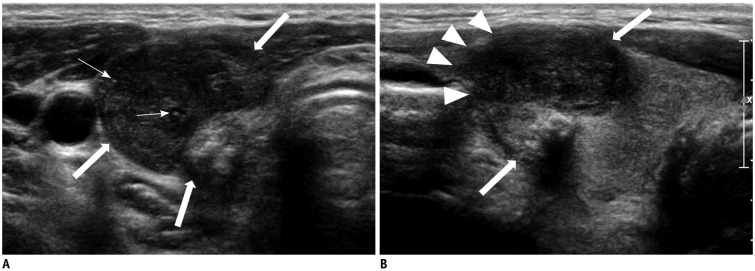
Columnar Cell Variant of Papillary Thyroid Carcinoma: Ultrasonographic and Clinical Differentiation between the Indolent and Aggressive Types
- Affiliations
-
- 1Department of Radiology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul 06351, Korea. jhshin11@skku.edu
- 2Department of Pathology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul 06351, Korea.
- KMID: 2418564
- DOI: http://doi.org/10.3348/kjr.2018.19.5.1000
Abstract
OBJECTIVE
To evaluate the ultrasonography (US) features and clinical characteristics of columnar cell variant of papillary thyroid carcinoma (CCV-PTC) that can predict disease progression.
MATERIALS AND METHODS
Six cases of CCV-PTC were identified via surgical pathology analysis at our institution from 1994 to 2016. The histological, architectural, and cytological features met the diagnostic criteria of CCV-PTC. We reviewed the US features and clinicopathological findings in the six cases.
RESULTS
An indolent clinical course was observed in four young female patients aged 27-34 years (median: 32 years), while two older patients aged 55 years or 70 years had an aggressive clinical course. All patients underwent total thyroidectomy and radioiodine therapy. The indolent group included patients with T1 and nodal metastasis, where the disease was not observed during the follow-up period (range: 8-17 years). On the other hand, a larger tumor size (1.8 cm and 6.0 cm), gross extrathyroidal extension to the muscle and lymph node, and distant metastasis were observed in the aggressive group. In one male patient, recurrence occurred immediately after operation, and this patient died 4 years after the diagnosis of thyroid cancer. Based on US, the individuals from the indolent group had a smooth margin, except for one. Both cases in the aggressive group had a microlobulated margin.
CONCLUSION
Favorable prognosis in CCV-PTC is observed in young patients with T1 staging and demonstrates a smooth margin at US. These US findings might help exclude the same treatment as the aggressive type in the indolent type of CCV-PTC.
MeSH Terms
Figure
Cited by 2 articles
-
Update from the 2022 World Health Organization Classification of Thyroid Tumors: A Standardized Diagnostic Approach
Chan Kwon Jung, Andrey Bychkov, Kennichi Kakudo
Endocrinol Metab. 2022;37(5):703-718. doi: 10.3803/EnM.2022.1553.Korean Thyroid Association Guidelines on the Management of Differentiated Thyroid Cancers; Part I. Initial Management of Differentiated Thyroid Cancers - Chapter 5. Evaluation of Recurrence Risk Postoperatively and Initial Risk Stratification in Differentiated Thyroid Cancer 2024
Eun Kyung Lee, Young Shin Song, Ho-Cheol Kang, Sun Wook Kim, Dong Gyu Na, Shin Je Moon, Dong-Jun Lim, Kyong Yeun Jung, Yun Jae Chung, Chan Kwon Jung, Young Joo Park
Int J Thyroidol. 2024;17(1):68-96. doi: 10.11106/ijt.2024.17.1.68.
Reference
-
1. Hundahl SA, Fleming ID, Fremgen AM, Menck HR. A National Cancer Data Base report on 53,856 cases of thyroid carcinoma treated in the U.S., 1985-1995 [see commetns]. Cancer. 1998; 83:2638–2648. PMID: 9874472.2. Papp S, Asa SL. When thyroid carcinoma goes bad: a morphological and molecular analysis. Head Neck Pathol. 2015; 9:16–23. PMID: 25804379.
Article3. Lee JH, Shin JH, Lee HW, Oh YL, Hahn SY, Ko EY. Sonographic and cytopathologic correlation of papillary thyroid carcinoma variants. J Ultrasound Med. 2015; 34:1–15.
Article4. Sywak M, Pasieka JL, Ogilvie T. A review of thyroid cancer with intermediate differentiation. J Surg Oncol. 2004; 86:44–54. PMID: 15048680.
Article5. Haugen BR, Alexander EK, Bible KC, Doherty GM, Mandel SJ, Nikiforov YE, et al. 2015 American Thyroid Association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: the American Thyroid Association guidelines task force on thyroid nodules and differentiated thyroid cancer. Thyroid. 2016; 26:1–133. PMID: 26462967.
Article6. Berends D, Mouthaan PJ. Columnar-cell carcinoma of the thyroid. Histopathology. 1992; 20:360–362. PMID: 1577416.
Article7. Evans HL. Columnar-cell carcinoma of the thyroid. A report of two cases of an aggressive variant of thyroid carcinoma. Am J Clin Pathol. 1986; 85:77–78. PMID: 3940424.
Article8. Gaertner EM, Davidson M, Wenig BM. The columnar cell variant of thyroid papillary carcinoma. Case report and discussion of an unusually aggressive thyroid papillary carcinoma. Am J Surg Pathol. 1995; 19:940–947. PMID: 7611541.
Article9. Evans HL. Encapsulated columnar-cell neoplasms of the thyroid. A report of four cases suggesting a favorable prognosis. Am J Surg Pathol. 1996; 20:1205–1211. PMID: 8827026.10. Ferreiro JA, Hay ID, Lloyd RV. Columnar cell carcinoma of the thyroid: report of three additional cases. Hum Pathol. 1996; 27:1156–1160. PMID: 8912824.
Article11. Wenig BM, Thompson LD, Adair CF, Shmookler B, Heffess CS. Thyroid papillary carcinoma of columnar cell type: a clinicopathologic study of 16 cases. Cancer. 1998; 82:740–753. PMID: 9477108.12. Shin JH. Ultrasonographic imaging of papillary thyroid carcinoma variants. Ultrasonography. 2017; 36:103–110. PMID: 28222584.
Article13. Shin JH, Baek JH, Chung J, Ha EJ, Kim JH, Lee YH, et al. Ultrasonography diagnosis and imaging-based management of thyroid nodules: revised Korean Society of Thyroid Radiology consensus statement and recommendations. Korean J Radiol. 2016; 17:370–395. PMID: 27134526.
Article14. Huang WT, Yang SF, Wang SL, Chan HM, Chai CY. Encapsulated columnar-cell carcinoma of the thyroid: a case report. Kaohsiung J Med Sci. 2005; 21:241–244. PMID: 15960072.
Article15. Chen JH, Faquin WC, Lloyd RV, Nosé V. Clinicopathological and molecular characterization of nine cases of columnar cell variant of papillary thyroid carcinoma. Mod Pathol. 2011; 24:739–749. PMID: 21358618.
Article16. Sujoy V, Pinto A, Nosś V. Columnar cell variant of papillary thyroid carcinoma: a study of 10 cases with emphasis on CDX2 expression. Thyroid. 2013; 23:714–719. PMID: 23488912.
Article17. Verma R, Paul P. Columnar cell variant of papillary thyroid carcinoma: a diagnostic dilemma in fine-needle aspiration cytology. Diagn Cytopathol. 2016; 44:816–819. PMID: 27279270.
Article18. Ylagan LR, Dehner LP, Huettner PC, Lu D. Columnar cell variant of papillary thyroid carcinoma. Report of a case with cytologic findings. Acta Cytol. 2004; 48:73–77. PMID: 14969185.19. Bongiovanni M, Mermod M, Canberk S, Saglietti C, Sykiotis GP, Pusztaszeri M, et al. Columnar cell variant of papillary thyroid carcinoma: cytomorphological characteristics of 11 cases with histological correlation and literature review. Cancer Cytopathol. 2017; 125:389–397. PMID: 28374549.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Columnar Cell Variant of Papillary Thyroid Carcinoma: Report of 2 Cases
- Fine Needle Aspiration Cytology of Columnar Cell Variant of Papillary Carcinoma of the Thyroid: A Case Report
- Urinalysis and Analysis and Imaging Studies in Children with Urinary Tract Infecion
- Diffuse Sclerosing Variant of Papillary Thyroid Carcinoma: Case Report
- Ultrasonographic imaging of papillary thyroid carcinoma variants