J Korean Ophthalmol Soc.
2018 Aug;59(8):718-723. 10.3341/jkos.2018.59.8.718.
Lid Wiper Epitheliopathy in Patients with Dry Eye Refractory to Conventional Medical Treatment
- Affiliations
-
- 1Department of Ophthalmology, Korea University College of Medicine, Seoul, Korea. crisim123@korea.ac.kr
- KMID: 2418497
- DOI: http://doi.org/10.3341/jkos.2018.59.8.718
Abstract
- PURPOSE
We evaluated the effects of lid wiper epitheliopathy on the clinical manifestations of dry eye in patients refractory to conventional medical treatment.
METHODS
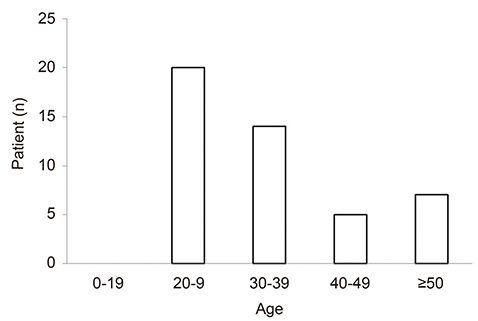
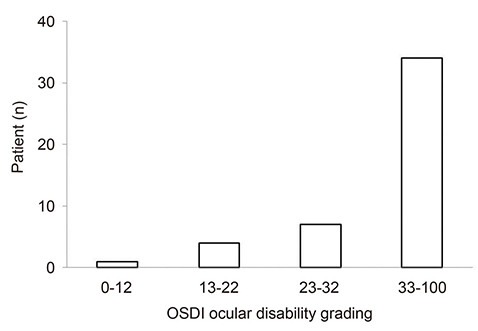
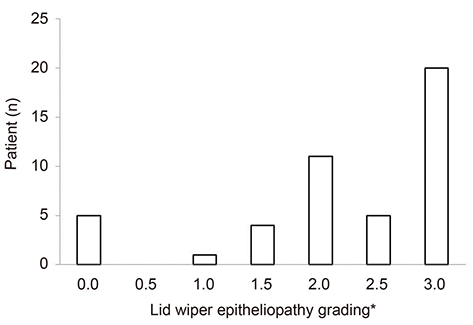
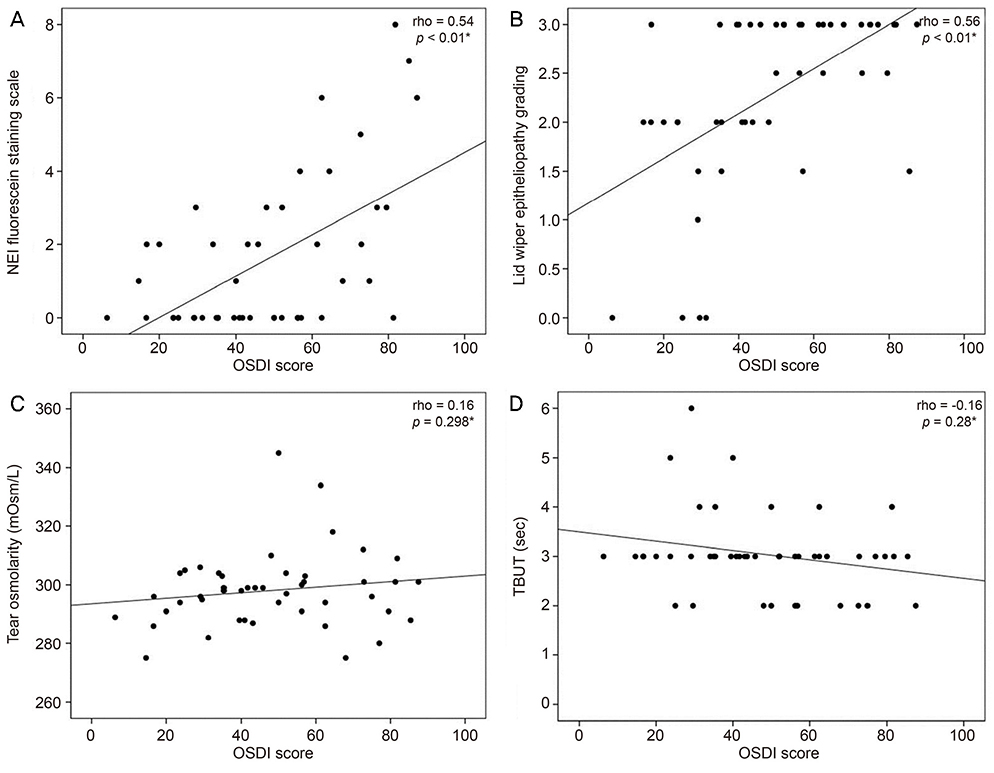
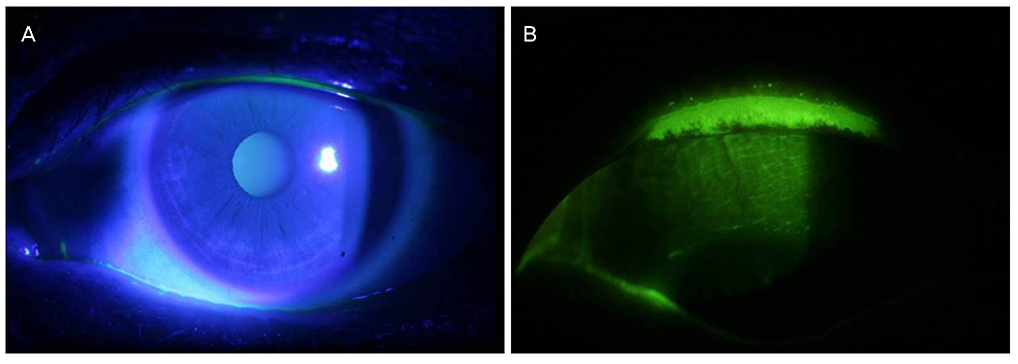
Forty-six patients (46 eyes) completed the subjective Ocular Surface Disease Index (OSDI), and we obtained objective measures including the tear break-up time (TBUT), the National Eye Institute (NEI) corneal staining score, tear osmolarity, and lid wiper epitheliopathy as revealed on photographs taken using a yellow filter after fluorescein instillation. The images were graded using the Korb B protocol.
RESULTS
The mean OSDI score was 48.06 ± 21.19; 34 patients (73.9%) were had scores ≥33. Lid wiper epitheliopathy was evident in 41 (89.1%), and the epitheliopathy grade and OSDI score were correlated (r = 0.56, p < 0.01). The NEI score was also positively correlated with the OSDI score (r = 0.54, p < 0.01), but the mean value was low (1.59 ± 2.13). The OSDI score did not correlate significantly with either the TBUT or tear osmolarity (r = −0.16, p = 0.279; r = 0.16, p = 0.298, respectively).
CONCLUSIONS
Lid wiper epitheliopathy was present in about 90% of patients with dry eye who visited our tertiary hospital, and a significant correlation was evident between the epitheliopathy grade and the OSDI score.
Keyword
MeSH Terms
Figure
Reference
-
1. The definition and classification of dry eye disease: report of the Definition and Classification Subcommittee of the International Dry Eye WorkShop (2007). Ocul Surf. 2007; 5:75–92.2. Ahn JM, Lee SH, Rim TH, et al. Prevalence of and risk factors associated with dry eye: the Korea National Health and Nutrition Examination Survey 2010-2011. Am J Ophthalmol. 2014; 158:1205–1214.e7.
Article3. Barabino S, Labetoulle M, Rolando M, Messmer EM. Understanding symptoms and quality of life in patients with dry eye syndrome. Ocul Surf. 2016; 14:365–376.4. Baudouin C, Aragona P, Van Setten G, et al. Diagnosing the severity of dry eye: a clear and practical algorithm. Br J Ophthalmol. 2014; 98:1168–1176.
Article5. Bartlett JD, Keith MS, Sudharshan L, Snedecor SJ. Associations between signs and symptoms of dry eye disease: a systematic review. Clin Ophthalmol. 2015; 9:1719–1730.
Article6. Nichols KK, Nichols JJ, Mitchell GL. The lack of association between signs and symptoms in patients with dry eye disease. Cornea. 2004; 23:762–770.
Article7. Schulze MM, Srinivasan S, Hickson-Curran SB, et al. Lid wiper epitheliopathy in soft contact lens wearers. Optom Vis Sci. 2016; 93:943–954.
Article8. Korb DR, Herman JP, Greiner JV, et al. Lid wiper epitheliopathy and dry eye symptoms. Eye Contact Lens. 2005; 31:2–8.
Article9. Efron N, Brennan NA, Morgan PB, Wilson T. Lid wiper epitheliopathy. Prog Retin Eye Res. 2016; 53:140–174.
Article10. Hyon JY, Kim HM, Lee D, et al. Korean guidelines for the diagnosis and management of dry eye: development and validation of clinical efficacy. Korean J Ophthalmol. 2014; 28:197–206.
Article11. Ng ALK, Choy BNK, Chan TCY, et al. Comparison of tear osmolarity in rheumatoid arthritis patients with and without secondary Sjogren syndrome. Cornea. 2017; 36:805–809.
Article12. Miller KL, Walt JG, Mink DR, et al. Minimal clinically important difference for the ocular surface disease index. Arch Ophthalmol. 2010; 128:94–101.
Article13. Yoon KC, Im SK, Kim HG, You IC. Usefulness of double vital staining with 1% fluorescein and 1% lissamine green in patients with dry eye syndrome. Cornea. 2011; 30:972–976.
Article14. Chun YS, Park IK. Reliability of 4 clinical grading systems for corneal staining. Am J Ophthalmol. 2014; 157:1097–1102.
Article15. Korb DR, Herman JP, Blackie CA, et al. Prevalence of lid wiper epitheliopathy in subjects with dry eye signs and symptoms. Cornea. 2010; 29:377–383.
Article16. Peck T, Olsakovsky L, Aggarwal S. Dry eye syndrome in menopause and perimenopausal age group. J Midlife Health. 2017; 8:51–54.17. McMonnies CW. An examination of the relationship between ocular surface tear osmolarity compartments and epitheliopathy. Ocul Surf. 2015; 13:110–117.
Article18. Yeniad B, Beginoglu M, Bilgin LK. Lid-wiper epitheliopathy in contact lens users and patients with dry eye. Eye Contact Lens. 2010; 36:140–143.
Article