Cancer Res Treat.
2018 Jul;50(3):768-776. 10.4143/crt.2017.141.
Survival Nomograms after Curative Neoadjuvant Chemotherapy and Radical Surgery for Stage IB2-IIIB Cervical Cancer
- Affiliations
-
- 1Department of Gynecological and Obstetrical Sciences and Urological Sciences, Policlinico Umberto I “Sapienza†University of Rome, Rome, Italy. clamarchetti@libero.it
- 2Department of Radiotherapy, Policlinico Umberto I “Sapienza†University of Rome, Rome, Italy.
- KMID: 2417866
- DOI: http://doi.org/10.4143/crt.2017.141
Abstract
- PURPOSE
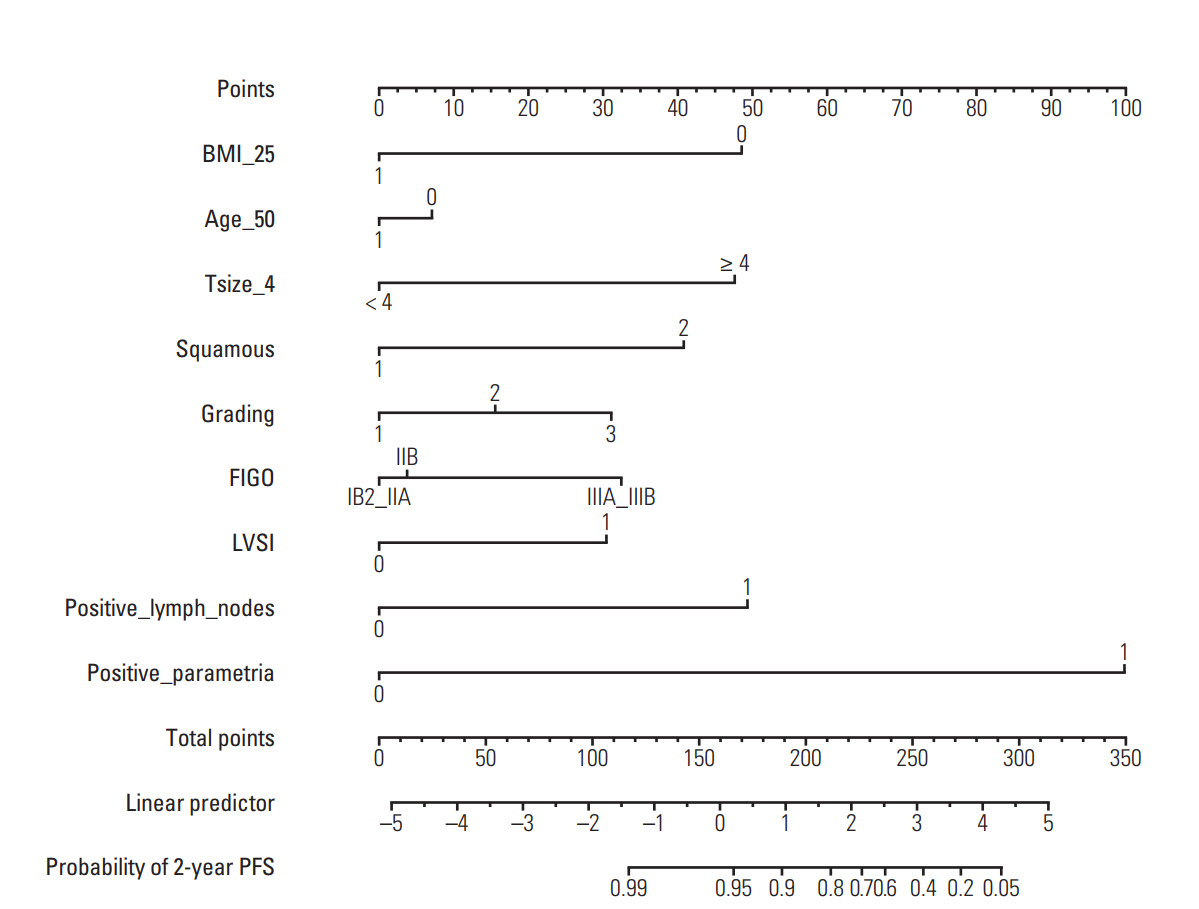
The purpose of this study was to develop nomograms for predicting the probability of overall survival (OS) and progression-free survival (PFS) in locally advanced cervical cancer treated with neoadjuvant chemotherapy and radical surgery.
MATERIALS AND METHODS
Nomograms to predict the 5-year OS rates and the 2-year PFS rates were constructed. Calibration plots were constructed, and concordance indices were calculated. Evaluated variableswere body mass index, age, tumor size, tumor histology, grading, lymphovascular space invasion, positive parametria, and positive lymph nodes.
RESULTS
In total 245 patients with locally advanced cervical cancer who underwent neoadjuvant chemotherapy and radical surgery were included for the construction of the nomogram. The 5-year OS and PFS were 72.6% and 66%, respectively. Tumor size, grading, and parametria status affected the rate of OS, whereas tumor size and positive parametria were the main independent PFS prognostic factors.
CONCLUSION
We constructed a nomogram based on clinicopathological features in order to predict 2-year PFS and 5-year OS in locally advanced cervical cancer primarily treated with neoadjuvant chemotherapy followed by radical surgery. This tool might be particularly helpful for assisting in the follow-up of cervical cancer patients who have not undergone concurrent chemoradiotherapy.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Siegel RL, Miller KD, Jemal A. Cancer statistics, 2016. CA Cancer J Clin. 2016; 66:7–30.
Article2. Lim MC, Moon EK, Shin A, Jung KW, Won YJ, Seo SS, et al. Incidence of cervical, endometrial, and ovarian cancer in Korea, 1999-2010. J Gynecol Oncol. 2013; 24:298–302.
Article3. National Cancer Institute. Concurrent chemoradiation for cervical cancer. Clinical announcement. Washington, DC: National Cancer Institute;1999.4. Neoadjuvant Chemotherapy for Locally Advanced Cervical Cancer Meta-analysis Collaboration. Neoadjuvant chemotherapy for locally advanced cervical cancer: a systematic review and meta-analysis of individual patient data from 21 randomised trials. Eur J Cancer. 2003; 39:2470–86.5. Benedetti Panici P, Bellati F, Pastore M, Manci N, Musella A, Pauselli S, et al. An update in neoadjuvant chemotherapy in cervical cancer. Gynecol Oncol. 2007; 107(1 Suppl 1):S20–2.
Article6. Je HU, Han S, Kim YS, Nam JH, Kim HJ, Kim JW, et al. A nomogram predicting the risks of distant metastasis following postoperative radiotherapy for uterine cervical carcinoma: a Korean radiation oncology group study (KROG 12-08). Radiother Oncol. 2014; 111:437–41.
Article7. Kong TW, Kim J, Son JH, Kang SW, Paek J, Chun M, et al. Preoperative nomogram for prediction of microscopic parametrial infiltration in patients with FIGO stage IB cervical cancer treated with radical hysterectomy. Gynecol Oncol. 2016; 142:109–14.
Article8. Polterauer S, Grimm C, Hofstetter G, Concin N, Natter C, Sturdza A, et al. Nomogram prediction for overall survival of patients diagnosed with cervical cancer. Br J Cancer. 2012; 107:918–24.
Article9. Kidd EA, El Naqa I, Siegel BA, Dehdashti F, Grigsby PW. FDG-PET-based prognostic nomograms for locally advanced cervical cancer. Gynecol Oncol. 2012; 127:136–40.
Article10. Seo Y, Yoo SY, Kim MS, Yang KM, Yoo HJ, Kim JH, et al. Nomogram prediction of overall survival after curative irradiation for uterine cervical cancer. Int J Radiat Oncol Biol Phys. 2011; 79:782–7.
Article11. Edge S, Byrd DR, Compton CC, Fritz AG, Greene FL, Trotti A. AJCC cancer staging handbook. New York: Springer-Verlag;2010.12. Capanu M, Gonen M. Building a nomogram for surveyweighted Cox models using R. J Stat Softw. 2015; 64:1–17.13. Benedetti-Panici P, Greggi S, Scambia G, Amoroso M, Salerno MG, Maneschi F, et al. Long-term survival following neoadjuvant chemotherapy and radical surgery in locally advanced cervical cancer. Eur J Cancer. 1998; 34:341–6.
Article14. Rose PG, Java J, Whitney CW, Stehman FB, Lanciano R, Thomas GM, et al. Nomograms predicting progression-free survival, overall survival, and pelvic recurrence in locally advanced cervical cancer developed from an analysis of identifiable prognostic factors in patients from NRG Oncology/Gynecologic Oncology Group randomized trials of chemoradiotherapy. J Clin Oncol. 2015; 33:2136–42.
Article15. Tseng JY, Yen MS, Twu NF, Lai CR, Horng HC, Tseng CC, et al. Prognostic nomogram for overall survival in stage IIB-IVA cervical cancer patients treated with concurrent chemoradiotherapy. Am J Obstet Gynecol. 2010; 202:174.
Article16. Benedetti-Panici P, Greggi S, Colombo A, Amoroso M, Smaniotto D, Giannarelli D, et al. Neoadjuvant chemotherapy and radical surgery versus exclusive radiotherapy in locally advanced squamous cell cervical cancer: results from the Italian multicenter randomized study. J Clin Oncol. 2002; 20:179–88.
Article17. Chen RJ, Lin YH, Chen CA, Huang SC, Chow SN, Hsieh CY. Influence of histologic type and age on survival rates for invasive cervical carcinoma in Taiwan. Gynecol Oncol. 1999; 73:184–90.
Article18. Gronchi A, Miceli R, Shurell E, Eilber FC, Eilber FR, Anaya DA, et al. Outcome prediction in primary resected retroperitoneal soft tissue sarcoma: histology-specific overall survival and disease-free survival nomograms built on major sarcoma center data sets. J Clin Oncol. 2013; 31:1649–55.
Article19. Meretoja TJ, Strien L, Heikkila PS, Leidenius MH. A simple nomogram to evaluate the risk of nonsentinel node metastases in breast cancer patients with minimal sentinel node involvement. Ann Surg Oncol. 2012; 19:567–76.
Article20. Wang Y, Li J, Xia Y, Gong R, Wang K, Yan Z, et al. Prognostic nomogram for intrahepatic cholangiocarcinoma after partial hepatectomy. J Clin Oncol. 2013; 31:1188–95.
Article21. Giordano A, Egleston BL, Hajage D, Bland J, Hortobagyi GN, Reuben JM, et al. Establishment and validation of circulating tumor cell-based prognostic nomograms in first-line metastatic breast cancer patients. Clin Cancer Res. 2013; 19:1596–602.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Recent Management of FIGO stage IB2 Cervical Cancer
- Comparative study of neoadjuvant chemotherapy before radical hysterectomy and radical surgery alone in stage IB2-IIA bulky cervical cancer
- Neoadjuvant chemotherapy in stage IB2 cervical cancer
- The outcome of the cervical cancer (stage Ib1) treated by radical surgery with and without neoadjuvant chemotherapy
- Prognosis of stage IIB cervical cancer among treatment regimens: Radical hysterectomy vs. neoadjuvant chemotherapy followed by radical hysterectomy vs. concurrent chemoradiotherapy