Ann Rehabil Med.
2018 Jun;42(3):483-487. 10.5535/arm.2018.42.3.483.
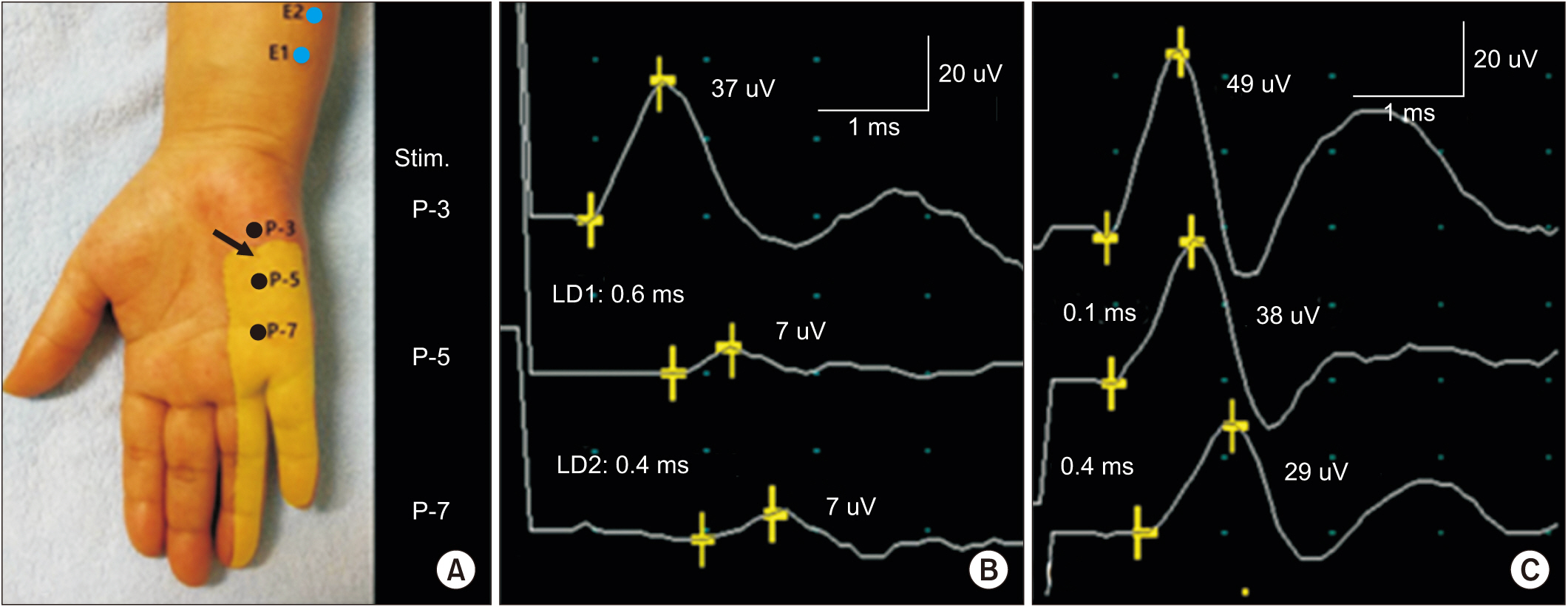
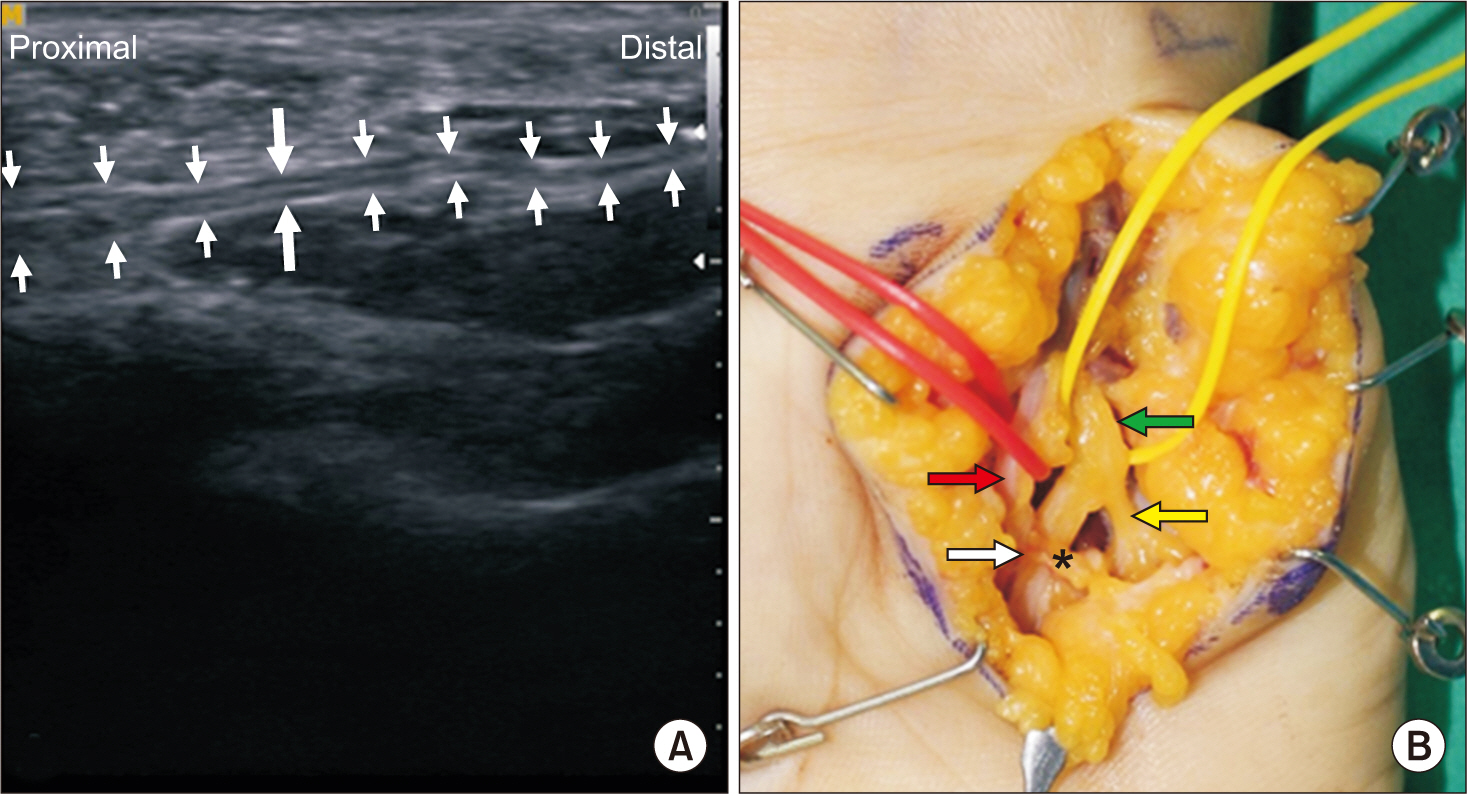
Diagnosis of Pure Ulnar Sensory Neuropathy Around the Hypothenar Area Using Orthodromic Inching Sensory Nerve Conduction Study: A Case Report
- Affiliations
-
- 1Department of Physical Medicine and Rehabilitation, Korea University Ansan Hospital, Ansan, Korea. rmkdh@korea.ac.kr
- 2Department of Orthopedic Surgery, Korea University Ansan Hospital, Ansan, Korea.
- KMID: 2417842
- DOI: http://doi.org/10.5535/arm.2018.42.3.483
Abstract
- Ulnar neuropathy at the wrist is an uncommon disease and pure ulnar sensory neuropathy at the wrist is even rarer. It is difficult to diagnose pure ulnar sensory neuropathy at the wrist by conventional methods. We report a case of pure ulnar sensory neuropathy at the hypothenar area. The lesion was localized between 3 cm and 5 cm distal to pisiform using orthodromic inching test of ulnar sensory nerve to stimulate at three points around the hypothenar area. Ultrasonographic examination confirmed compression of superficial sensory branch of the ulnar nerve. Further, surgical exploration reconfirmed compression of the ulnar nerve. This case report demonstrates the utility of orthodromic ulnar sensory inching test.
MeSH Terms
Figure
Reference
-
1. Preston DC, Shapiro BE. Electromyography and neuromuscular disorders: clinical-electrophysiologic correlations. 3rd ed. London: Elsevier;2013. p. 319.2. Olney RK, Hanson M. AAEE case report #15: ulnar neuropathy at or distal to the wrist. Muscle Nerve. 1988; 11:828–32.
Article3. Kim DH, Kang YK, Hwang M, Kwon HK, Lee HJ, Kim BG. Reference values of fractionated neurography of the ulnar nerve at the wrist in healthy subjects. Clin Neurophysiol. 2005; 116:2853–7.
Article4. McIntosh KA, Preston DC, Logigian EL. Short-segment incremental studies to localize ulnar nerve entrapment at the wrist. Neurology. 1998; 50:303–6.
Article5. Seror P. Electrophysiological pattern of 53 cases of ulnar nerve lesion at the wrist. Neurophysiol Clin. 2013; 43:95–103.6. Lee HJ, DeLisa JA. Manual of nerve conduction study and surface anatomy for needle electromyography. 4th ed. Philadelphia: Lippincott Williams & Wilkins;2005. p. 25–27. p. 34p. 36–38. p. 45–49. p. 52–55.7. Kim Y, Kim DH, Kim NH, Kim BH, Park BK. Dorsal sural neuropathy: electrophysiological, ultrasonographic, and magnetic resonance imaging findings. Muscle Nerve. 2012; 46:597–600.
Article8. Dumitru D, Amato AA, Zwarts MJ. Electrodiagnostic medicine. 2nd ed. Philadelphia: Hanley & Belfus;2002. p. 1084.9. Preston DC, Shapiro BE. Electromyography and neuromuscular disorders: clinical-electrophysiologic correlations. 3rd ed. London: Elsevier;2013. p. 322–23.10. Kim KH, Park BK, Kim DH. A case of lateral calcaneal neuropathy: lateral heel pain. Muscle Nerve. 2016; 54:801–4.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Antidromic and Orthodromic Sensory Conduction of Ring Finger in Carpal Tunnel Syndrome
- Pitfalls in Superficial Radial Sensory Nerve Conduction Study
- The Diagnostic Value of Segmental Nerve Conduction Study in Diabetics
- Ulnar Neuropathy Around the Mid-Arm Combined with Martin-Gruber Anastomosis
- Hereditary Motor and Sensory Neuropathy Type I: A case report