Ann Pediatr Endocrinol Metab.
2018 Jun;23(2):75-80. 10.6065/apem.2018.23.2.75.
Etiological trends in male central precocious puberty
- Affiliations
-
- 1Department of Pediatrics, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. nadri1217@naver.com, jindk@skku.edu
- KMID: 2417763
- DOI: http://doi.org/10.6065/apem.2018.23.2.75
Abstract
- PURPOSE
In the present study, the etiological trends in male central precocious puberty (CPP) were examined, and annual distribution was evaluated.
METHODS
Seventy-one male CPP subjects who started puberty before 9 years of age were included in this study. All individuals were diagnosed as having CPP at Samsung Medical Center between 2001 and 2016. Chronological age at puberty onset, diagnosis of CPP, bone age, weight (kg), height (cm), puberty stage, brain magnetic resonance imaging findings, testosterone level, basal gonadotropin level, and gonadotropin level after gonadotropin releasing hormone stimulation were analyzed.
RESULTS
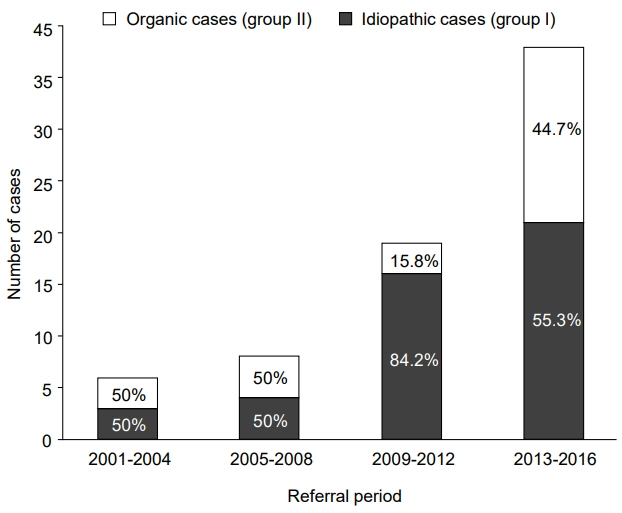
The 71 patients were divided into 2 groups: idiopathic (group I) and organic (group II) when the lesion was identified as associated with the central nervous system (CNS) or when the patient received chemotherapy for non-CNS tumors before CPP diagnosis, respectively. Forty-four cases (62%) were idiopathic, and 27 (38%) were organic. The proportion of idiopathic CPP was higher than that of organic CPP during the study period. In 51.9% of organic cases, puberty started before 8 years of age, whereas it started after that age in 93.2% of the idiopathic cases.
CONCLUSIONS
In the present study, among all male CPP cases, 62% were idiopathic. The probability of idiopathic CPP prevalence was higher in males when the puberty onset was after 8 years of age with no history of cranial radiotherapy or chemotherapy.
MeSH Terms
Figure
Reference
-
References
1. Berberoğlu M. Precocious puberty and normal variant puberty: definition, etiology, diagnosis and current management. J Clin Res Pediatr Endocrinol. 2009; 1:164–74.2. Stephen MD, Zage PE, Waguespack SG. Gonadotrop-independent precocious puberty: neoplastic causes and endocrine considerations. Int J Pediatr Endocrinol. 2011; 2011:184502.
Article3. Rohani F, Salehpur S, Saffari F. Etiology of precocious puberty, 10 years study in Endocrine Reserch Centre (Firouzgar), Tehran. Iran J Reprod Med. 2012; 10:1–6.4. Kalantaridou SN, Chrousos GP. Clinical review 148: monogenic disorders of puberty. J Clin Endocrinol Metab. 2002; 87:2481–94.5. Lee PA KJ. Precocious puberty. In : Pescovitz OH, Eugster EA, editors. Textbook of pediatric endocrinology. Philadelphia (PA): Lippincott Williams & Wilkins;2014. p. 316–30.6. Carel JC, Léger J. Clinical practice. Precocious puberty. N Engl J Med. 2008; 358:2366–77.7. Carel JC, Lahlou N, Roger M, Chaussain JL. Precocious puberty and statural growth. Hum Reprod Update. 2004; 10:135–47.
Article8. Pescovitz OH, Comite F, Hench K, Barnes K, McNemar A, Foster C, et al. The NIH experience with precocious puberty: diagnostic subgroups and response to short-term luteinizing hormone releasing hormone analogue therapy. J Pediatr. 1986; 108:47–54.
Article9. Pigneur B, Trivin C, Brauner R. Idiopathic central precocious puberty in 28 boys. Med Sci Monit. 2008; 14:CR10–14.10. Alikasifoglu A, Vuralli D, Gonc EN, Ozon A, Kandemir N. Changing etiological trends in male precocious puberty: evaluation of 100 cases with central precocious puberty over the last decade. Horm Res Paediatr. 2015; 83:340–4.
Article11. De Sanctis V, Corrias A, Rizzo V, Bertelloni S, Urso L, Galluzzi F, et al. Etiology of central precocious puberty in males: the results of the Italian Study Group for Physiopathology of Puberty. J Pediatr Endocrinol Metab. 2000; 13 Suppl 1:687–93.
Article12. Bajpai A, Menon PS. Contemporary issues in precocious puberty. Indian J Endocrinol Metab. 2011; 15 Suppl 3:S172–9.13. Cisternino M, Arrigo T, Pasquino AM, Tinelli C, Antoniazzi F, Beduschi L, et al. Etiology and age incidence of precocious puberty in girls: a multicentric study. J Pediatr Endocrinol Metab. 2000; 13:695–701.
Article14. Moon JS, Lee SY, Nam CM, Choi JM, Choe BK, Seo JW, et al. 2007 Korean National Growth Charts: review of developmental process and an outlook. Korean J Pediatr. 2008; 51:1–25.
Article15. Marshall WA, Tanner JM. Variations in the pattern of pubertal changes in boys. Arch Dis Child. 1970; 45:13–23.
Article16. Milner GR, Levick RK, Kay R. Assessment of bone age: a comparison of the Greulich and Pyle, and the Tanner and Whitehouse methods. Clin Radiol. 1986; 37:119–21.
Article17. Kim SH, Huh K, Won S, Lee KW, Park MJ. A Significant increase in the incidence of central precocious puberty among Korean girls from 2004 to 2010. PLoS One. 2015; 10:e0141844.
Article18. Stanhope R. Central precocious puberty and occult intracranial tumours. Clin Endocrinol (Oxf). 2001; 54:287–8.
Article19. Leiper AD, Stanhope R, Kitching P, Chessells JM. Precocious and premature puberty associated with treatment of acute lymphoblastic leukaemia. Arch Dis Child. 1987; 62:1107–12.
Article20. Oberfield SE, Soranno D, Nirenberg A, Heller G, Allen JC, David R, et al. Age at onset of puberty following high-dose central nervous system radiation therapy. Arch Pediatr Adolesc Med. 1996; 150:589–92.
Article21. Spoudeas HA. Growth and endocrine function after chemotherapy and radiotherapy in childhood. Eur J Cancer. 2002; 38:1748–59.
Article22. Müller J. Disturbance of pubertal development after cancer treatment. Best Pract Res Clin Endocrinol Metab. 200r; 16:91–103.
Article23. Schwartz CL. Long-term survivors of childhood cancer: the late effects of therapy. Oncologist. 1999; 4:45–54.
Article24. Parent AS, Rasier G, Gerard A, Heger S, Roth C, Mastronardi C, et al. Early onset of puberty: tracking genetic and environmental factors. Horm Res. 2005; 64 Suppl 2:41–7.
Article25. Sørensen K, Mouritsen A, Aksglaede L, Hagen CP, Mogensen SS, Juul A. Recent secular trends in pubertal timing: implications for evaluation and diagnosis of precocious puberty. Horm Res Paediatr. 2012; 77:137–45.
Article26. Laron Z. Is obesity associated with early sexual maturation? Pediatrics. 2004; 113(1 Pt 1):171–2.
Article27. Ribeiro J, Santos P, Duarte J, Mota J. Association between overweight and early sexual maturation in Portuguese boys and girls. Ann Hum Biol. 2006; 33:55–63.
Article28. He Q, Karlberg J. Bmi in childhood and its association with height gain, timing of puberty, and final height. Pediatr Res. 2001; 49:244–51.
Article29. Sørensen K, Aksglaede L, Petersen JH, Juul A. Recent changes in pubertal timing in healthy Danish boys: associations with body mass index. J Clin Endocrinol Metab. 2010; 95:263–70.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Diagnosis and Treatment of Central Precocious Puberty
- Central Precocious Puberty Following Treatment of Precocious Pseudo-Puberty Caused by Leydig Cell Tumor: A Pediatric Case and Literature Review
- Clinical Experiences of Precocious Puberty due to Neoplasms in Male Infants
- Two Cases of Secondary Central Precocious Puberty in Boys with Congenital Adrenal Hyperplasia - before and after Treatment with Corticosteroid
- Etiology and Age Incidence of Precocious Puberty