Korean Circ J.
2018 Aug;48(8):744-754. 10.4070/kcj.2018.0046.
Variable Hemodynamic Responses during Diastolic Stress Echocardiography in Patients Who Have Relaxation Abnormality with Possible Elevated Filling Pressure
- Affiliations
-
- 1Department of Medicine, Graduate School, Kyung Hee University, Seoul, Korea.
- 2Asan Medical Center Heart Institute, University of Ulsan College of Medicine, Seoul, Korea. jksong@amc.seoul.kr
- KMID: 2417699
- DOI: http://doi.org/10.4070/kcj.2018.0046
Abstract
- BACKGROUND AND OBJECTIVES
The clinical characteristics of patients with diastolic dysfunction characterized by a relaxation abnormality with possible elevated filling pressure is remain to be determined. We sought to test whether diastolic stress echocardiography (DSE) is useful for characterization of these patients.
METHODS
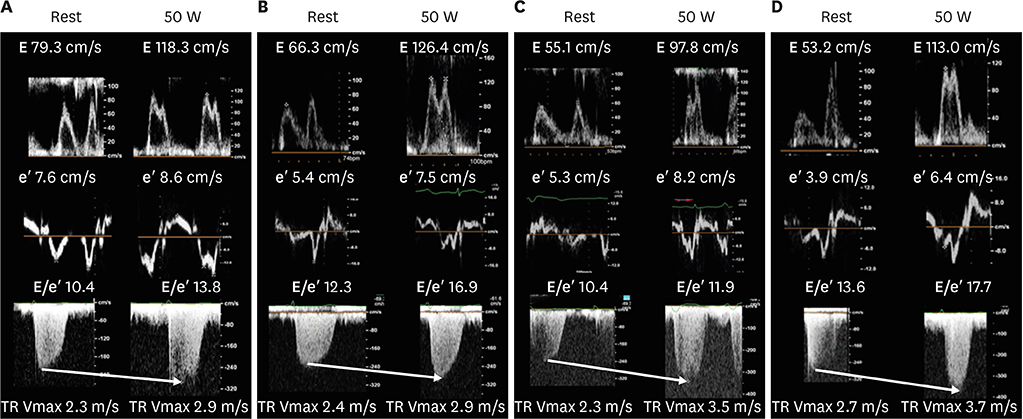
A total of 120 patients (58 men, mean age of 64±7 years) with E/A ratio < 1.0 (mean±SD, 0.7±0.1) and 10≤ E/e' < 15 at rest echocardiography was enrolled prospectively for supine bicycle exercise up to 50 W.
RESULTS
During exercise, 47 patients (39%) showed high left ventricular filling pressure (E/e' > 15, hLVFP) and 40 (30%) developed exercise-induced pulmonary hypertension (systolic pulomary arterial pressure > 50 mmHg, EiPH) without hLVFP. The remaining 33 patients did not show hLVFP or EiPH. The incidence of EiPH with hLVFP was 21% (25/120). By multivariate analysis, age (odds ratio [OR], 1.07; 95% confidence interval [CI], 1.00-1.13; p=0.039) and systolic pulmonary artery pressure at rest (OR, 1.14; 95% CI, 1.02-1.27; p=0.02) were associated with EiPH, whereas late diastolic transmitral velocity (OR, 1.04; 95% CI, 1.00-1.08; p=0.03) and diastolic blood pressure (OR, 0.94; 95% CI, 0.90-0.99; p=0.02) were associated with hLVFP during exercise.
CONCLUSIONS
Patients with relaxation abnormality and possibly hLVFP showed markedly heterogeneous hemodynamic changes during low-level exercise and DSE was useful to characterize these patients.
Keyword
MeSH Terms
Figure
Cited by 1 articles
Reference
-
1. Nagueh SF, Appleton CP, Gillebert TC, et al. Recommendations for the evaluation of left ventricular diastolic function by echocardiography. J Am Soc Echocardiogr. 2009; 22:107–133.
Article2. Unzek S, Popovic ZB, Marwick TH; Diastolic Guidelines Concordance Investigators. Effect of recommendations on interobserver consistency of diastolic function evaluation. JACC Cardiovasc Imaging. 2011; 4:460–467.
Article3. Kuwaki H, Takeuchi M, Wu VC, et al. Redefining diastolic dysfunction grading: combination of E/A ≤0.75 and deceleration time >140 ms and E/ε′ ≥10. JACC Cardiovasc Imaging. 2014; 7:749–758.4. Pandit A, Mookadam F, Hakim FA, et al. Ia diastolic dysfunction: an echocardiographic grade. Echocardiography. 2015; 32:56–63.
Article5. Fontes-Carvalho R, Azevedo A, Leite-Moreira A. Is new grade Ia of diastolic dysfunction relevant at the population level? JACC Cardiovasc Imaging. 2015; 8:229–230.
Article6. Ha JW, Oh JK, Pellikka PA, et al. Diastolic stress echocardiography: a novel noninvasive diagnostic test for diastolic dysfunction using supine bicycle exercise Doppler echocardiography. J Am Soc Echocardiogr. 2005; 18:63–68.
Article7. Burgess MI, Jenkins C, Sharman JE, Marwick TH. Diastolic stress echocardiography: hemodynamic validation and clinical significance of estimation of ventricular filling pressure with exercise. J Am Coll Cardiol. 2006; 47:1891–1900.
Article8. Nagueh SF, Smiseth OA, Appleton CP, et al. Recommendations for the evaluation of left ventricular diastolic function by echocardiography: an update from the American society of echocardiography and the European association of cardiovascular imaging. J Am Soc Echocardiogr. 2016; 29:277–314.9. Ha JW, Choi D, Park S, et al. Determinants of exercise-induced pulmonary hypertension in patients with normal left ventricular ejection fraction. Heart. 2009; 95:490–494.
Article10. Shim CY, Kim SA, Choi DH, et al. Clinical outcomes of exercise-induced pulmonary hypertension in subjects with preserved left ventricular ejection fraction: implication of an increase in left ventricular filling pressure during exercise. Heart. 2011; 97:1417–1424.
Article11. Seo JS, Jang MK, Lee EY, et al. Evaluation of left ventricular diastolic function after valve replacement in aortic stenosis using exercise Doppler echocardiography. Circ J. 2012; 76:2792–2798.
Article12. Lancellotti P, Pellikka PA, Budts W, et al. The clinical use of stress echocardiography in non-ischaemic heart disease: recommendations from the European association of cardiovascular imaging and the American society of echocardiography. Eur Heart J Cardiovasc Imaging. 2016; 17:1191–1229.
Article13. Bhatia RS, Tu JV, Lee DS, et al. Outcome of heart failure with preserved ejection fraction in a population-based study. N Engl J Med. 2006; 355:260–269.
Article14. Davies M, Hobbs F, Davis R, et al. Prevalence of left-ventricular systolic dysfunction and heart failure in the echocardiographic heart of England screening study: a population based study. Lancet. 2001; 358:439–444.
Article15. Podolec P, Rubis P, Tomkiewicz-Pajak L, Kopec G, Tracz W. Usefulness of the evaluation of left ventricular diastolic function changes during stress echocardiography in predicting exercise capacity in patients with ischemic heart failure. J Am Soc Echocardiogr. 2008; 21:834–840.
Article16. Kane GC, Oh JK. Diastolic stress test for the evaluation of exertional dyspnea. Curr Cardiol Rep. 2012; 14:359–365.
Article17. Marchandise S, Vanoverschelde JL, D'Hondt AM, et al. Usefulness of tissue Doppler imaging to evaluate pulmonary capillary wedge pressure during exercise in patients with reduced left ventricular ejection fraction. Am J Cardiol. 2014; 113:2036–2044.
Article18. Lester SJ, Tajik AJ, Nishimura RA, Oh JK, Khandheria BK, Seward JB. Unlocking the mysteries of diastolic function: deciphering the Rosetta Stone 10 years later. J Am Coll Cardiol. 2008; 51:679–689.19. Song JK, Kang DH, Lee CW, et al. Factors determining the exercise capacity in mitral stenosis. Am J Cardiol. 1996; 78:1060–1062.
Article20. Piérard LA, Lancellotti P. The role of ischemic mitral regurgitation in the pathogenesis of acute pulmonary edema. N Engl J Med. 2004; 351:1627–1634.
Article21. Magne J, Lancellotti P, Pierard LA. Exercise pulmonary hypertension in asymptomatic degenerative mitral regurgitation. Circulation. 2010; 122:33–41.
Article22. Kulik TJ, Bass JL, Fuhrman BP, Moller JH, Lock J. Exercise induced pulmonary vasoconstriction. Br Heart J. 1983; 50:59–64.
Article23. Bossone E, Rubenfire M, Bach DS, Ricciardi M, Armstrong WF. Range of tricuspid regurgitation velocity at rest and during exercise in normal adult men: implications for the diagnosis of pulmonary hypertension. J Am Coll Cardiol. 1999; 33:1662–1666.
Article24. Bidart CM, Abbas AE, Parish JM, Chaliki HP, Moreno CA, Lester SJ. The noninvasive evaluation of exercise-induced changes in pulmonary artery pressure and pulmonary vascular resistance. J Am Soc Echocardiogr. 2007; 20:270–275.
Article25. Magne J, Donal E, Mahjoub H, et al. Impact of exercise pulmonary hypertension on postoperative outcome in primary mitral regurgitation. Heart. 2015; 101:391–396.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Diastolic Stress Echocardiography to Quantify the Response of Diastolic Functional Indices to Dynamic Exercise in Abnormal Relaxation: Unmasking Diastolic Abnormalities is Getting Ready for Prime Time
- Use and Limitations of E/e' to Assess Left Ventricular Filling Pressure by Echocardiography
- Doppler Flow Patterns of Constrictive Pericarditis
- A Study for Diastolic Functions in Patients with Early Acute Myocardial Infarction
- Clinical Utility of Mitral Annulus Velocity to Estimate Left Ventricular Filling Pressure