Intest Res.
2018 Apr;16(2):216-222. 10.5217/ir.2018.16.2.216.
Characteristics and management of patients with inflammatory bowel disease between a secondary and tertiary hospitals: a propensity score analysis
- Affiliations
-
- 1Department of Surgery, Goo Hospital, Daegu, Korea.
- 2Department of Internal Medicine, School of Medicine, Kyungpook National University, Daegu, Korea. dandy813@hanmail.net
- 3Department of Internal Medicine, Keimyung University School of Medicine, Daegu, Korea.
- 4Department of Internal Medicine, Yeungnam University College of Medicine, Daegu, Korea.
- 5Department of Medical Statistics, Catholic University of Daegu School of Medicine, Daegu, Korea.
- KMID: 2417673
- DOI: http://doi.org/10.5217/ir.2018.16.2.216
Abstract
- BACKGROUND/AIMS
This study aimed to compare the clinical characteristics and management patterns of inflammatory bowel disease (IBD) patients in a secondary hospital (SH) with those in tertiary referral centers (TRC).
METHODS
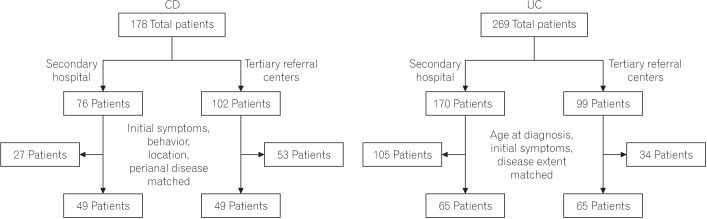
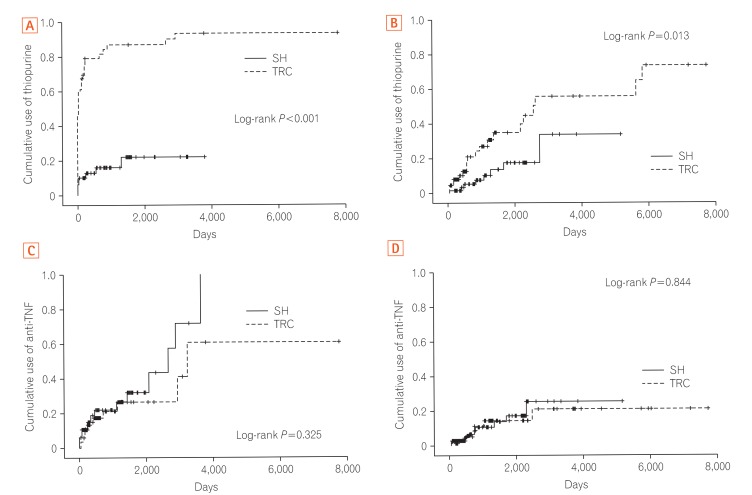
Data from IBD patients in SH and 2 TRCs were retrospectively reviewed. The cumulative thiopurine use rate was compared between hospitals after controlling for different baseline characteristics using propensity score matching.
RESULTS
Among the total of 447 patients with IBD, 178 Crohn's disease (CD) and 269 ulcerative colitis (UC) patients were included. Regarding initial CD symptoms, patients from SH were more likely to show perianal symptoms, such as anal pain or discharge (56.6% vs. 34.3%, P=0.003), whereas those from TRCs more often had luminal symptoms, such as abdominal pain (54.9% vs. 17.1%, P < 0.001), diarrhea (44.1% vs. 18.4%, P < 0.001), and body weight loss (9.8% vs. 1.3%, P=0.025). Complicating behaviors, such as stricturing and penetrating, were significantly higher in TRCs, while perianal disease was more common in SH. Ileal location was more frequently observed in TRCs. For UC, SH had a more limited extent of disease (proctitis 58.8% vs. 21.2%, P < 0.001). The cumulative azathioprine use rate in SH was significantly lower than that in TRCs in both CD and UC patients after controlling for disease behavior, location, and perianal disease of CD and extent of UC.
CONCLUSIONS
The clinical characteristics and management of the IBD patients in SH were substantially different from those in TRCs. Thiopurine treatment was less commonly used for SH patients.
MeSH Terms
Figure
Reference
-
1. Baumgart DC, Bernstein CN, Abbas Z, et al. IBD Around the world: comparing the epidemiology, diagnosis, and treatment: proceedings of the World Digestive Health Day 2010: Inflammatory Bowel Disease Task Force meeting. Inflamm Bowel Dis. 2011; 17:639–644. PMID: 20725944.
Article2. Thia KT, Loftus EV Jr, Sandborn WJ, Yang SK. An update on the epidemiology of inflammatory bowel disease in Asia. Am J Gastroenterol. 2008; 103:3167–3182. PMID: 19086963.
Article3. Ng SC, Tang W, Ching JY, et al. Incidence and phenotype of inflammatory bowel disease based on results from the Asia-Pacific Crohn's and Colitis Epidemiology Study. Gastroenterology. 2013; 145:158–165.e2. PMID: 23583432.
Article4. Ng WK, Wong SH, Ng SC. Changing epidemiological trends of inflammatory bowel disease in Asia. Intest Res. 2016; 14:111–119. PMID: 27175111.
Article5. Tursi A, Elisei W, Picchio M. Incidence and prevalence of inflammatory bowel diseases in gastroenterology primary care setting. Eur J Intern Med. 2013; 24:852–856. PMID: 23867759.
Article6. Ye BD, Jang BI, Jeen YT, et al. Diagnostic guideline of Crohn's disease. Korean J Gastroenterol. 2009; 53:161–176. PMID: 19835218.7. Choi CH, Jung SA, Lee BI, et al. Diagnostic guideline of ulcerative colitis. Korean J Gastroenterol. 2009; 53:145–160. PMID: 19835217.8. Thomas A, Lodhia N. Advanced therapy for inflammatory bowel disease: a guide for the primary care physician. J Am Board Fam Med. 2014; 27:411–420. PMID: 24808120.
Article9. Torjesen I. Care of IBD patients compromised by poor communication between primary and secondary care. BMJ. 2012; 344:e2675. DOI: 10.1136/bmj.e2675. PMID: 22498956.
Article10. Ye BD, Yang SK, Cho YK, et al. Clinical features and long-term prognosis of Crohn's disease in Korea. Scand J Gastroenterol. 2010; 45:1178–1185. PMID: 20560811.
Article11. Bernell O, Lapidus A, Hellers G. Risk factors for surgery and postoperative recurrence in Crohn's disease. Ann Surg. 2000; 231:38–45. PMID: 10636100.
Article12. Reenaers C, Pirard C, Vankemseke C, Latour P, Belaiche J, Louis E. Long-term evolution and predictive factors of mild inflammatory bowel disease. Scand J Gastroenterol. 2016; 51:712–719. PMID: 26815198.
Article13. Riegler G, Tartaglione MT, Carratú R, et al. Age-related clinical severity at diagnosis in 1705 patients with ulcerative colitis: a study by GISC (Italian Colon-Rectum Study Group). Dig Dis Sci. 2000; 45:462–465. PMID: 10749318.14. Choi JH, Kim ES, Cho KB, et al. Old age at diagnosis is associated with favorable outcomes in Korean patients with inflammatory bowel disease. Intest Res. 2015; 13:60–67. PMID: 25691844.
Article15. Fischer SH, Tjia J, Reed G, Peterson D, Gurwitz JH, Field TS. Factors associated with ordering laboratory monitoring of high-risk medications. J Gen Intern Med. 2014; 29:1589–1598. PMID: 24965280.
Article16. Yang SK, Hong M, Baek J, et al. A common missense variant in NUDT15 confers susceptibility to thiopurine-induced leukopenia. Nat Genet. 2014; 46:1017–1020. PMID: 25108385.
Article17. Takatsu N, Matsui T, Murakami Y, et al. Adverse reactions to azathioprine cannot be predicted by thiopurine S-methyltransferase genotype in Japanese patients with inflammatory bowel disease. J Gastroenterol Hepatol. 2009; 24:1258–1264. PMID: 19682195.
Article18. Connell WR, Kamm MA, Ritchie JK, Lennard-Jones JE. Bone marrow toxicity caused by azathioprine in inflammatory bowel disease: 27 years of experience. Gut. 1993; 34:1081–1085. PMID: 8174958.
Article19. Fraser AG, Orchard TR, Jewell DP. The efficacy of azathioprine for the treatment of inflammatory bowel disease: a 30 year review. Gut. 2002; 50:485–489. PMID: 11889067.
Article20. Lee KM, Kim YS, Seo GS, Kim TO, Yang SK. IBD Study Group of the Korean Association for the Study of Intestinal Diseases. Use of thiopurines in inflammatory bowel disease: a consensus statement by the Korean Association for the Study of Intestinal Diseases (KASID). Intest Res. 2015; 13:193–207. PMID: 26130993.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Interhospital Comparison of Outcome from Intensive Care Unit with APACHE III Scoring System
- Difference in Healthcare Utilization for Percutaneous Transluminal Coronary Angioplasty Inpatients by Insurance Types: Propensity Score Matching Analysis
- Inflammatory Bowel Disease in Pediatric Age
- Nutritional concerns in pediatric inflammatory bowel disease
- The Pharmacotherapy of Inflammatory Bowel Disease in Child and Adolescence