Prog Med Phys.
2018 Jun;29(2):66-72. 10.14316/pmp.2018.29.2.66.
Verification of Mechanical Leaf Gap Error and VMAT Dose Distribution on Varian VitalBeamâ„¢ Linear Accelerator
- Affiliations
-
- 1Biomedical Research Institution, Seoul National University Hospital, Seoul, Korea.
- 2Department of Radiation Oncology, Seoul National University Hospital, Seoul, Korea.
- 3Department of Radiation Oncology, Veterans Health Service Medical Center, Seoul, Korea. vsoyounv@gmail.com
- KMID: 2415905
- DOI: http://doi.org/10.14316/pmp.2018.29.2.66
Abstract
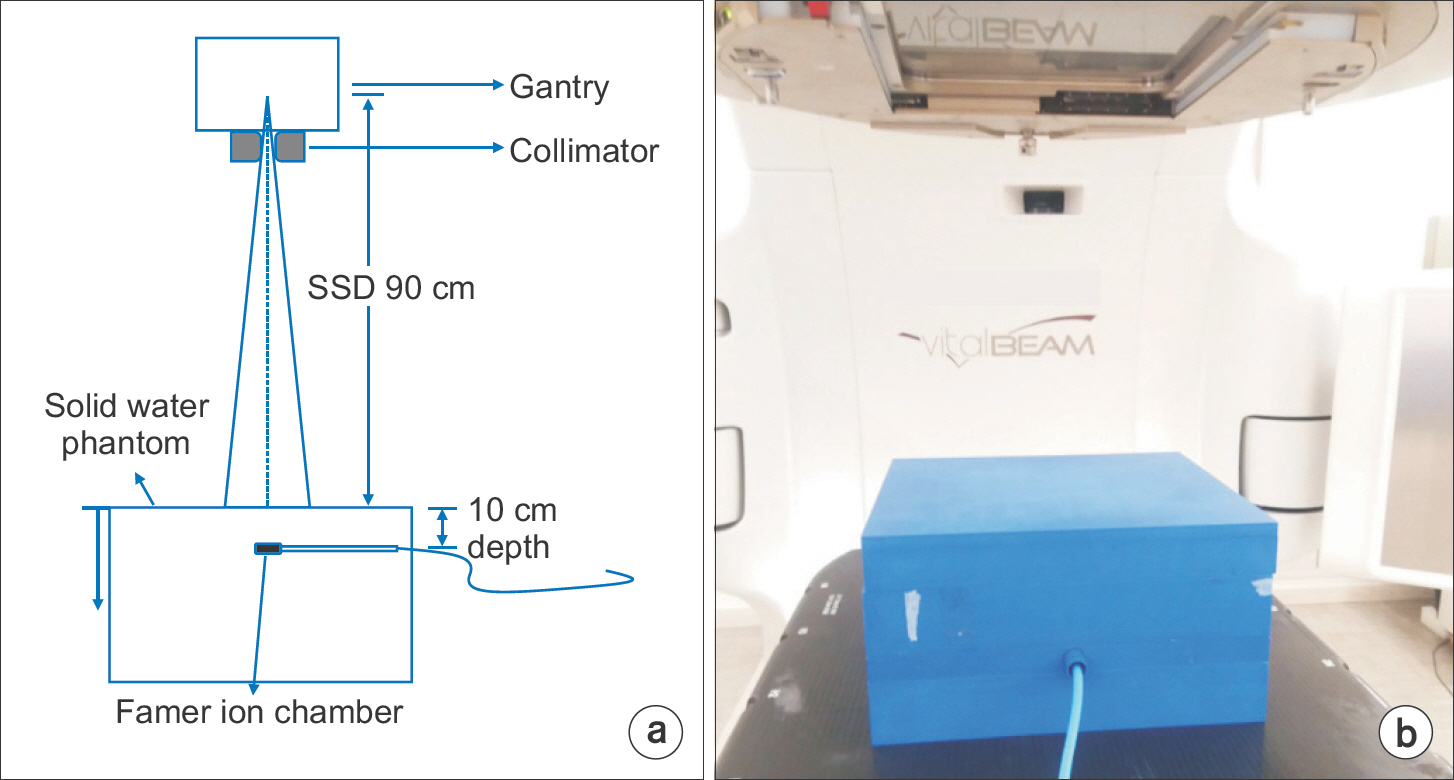
- The proper position of a multi-leaf collimator (MLC) is essential for the quality of intensity-modulated radiation therapy (IMRT) and volumetric modulated arc radiotherapy (VMAT) dose delivery. Task Group (TG) 142 provides a quality assurance (QA) procedure for MLC position. Our study investigated the QA validation of the mechanical leaf gap measurement and the maintenance procedure. Two VitalBeamâ„¢ systems were evaluated to validate the acceptance of an MLC position. The dosimetric leaf gaps (DLGs) were measured for 6 MV, 6 MVFFF, 10 MV, and 15 MV photon beams. A solid water phantom was irradiated using 10×10 cm² f ield s ize a t s ource-to-surface distance (SSD) of 90 cm and depth of 10 cm. The portal dose image prediction (PDIP) calculation was implemented on a treatment planning system (TPS) called Eclipseâ„¢. A total of 20 VMAT plans were used to confirm the accuracy of dose distribution measured by an electronic portal imaging device (EPID) and those predicted by VMAT plans. The measured leaf gaps were 0.30 mm and 0.35 mm for VitalBeam 1 and 2, respectively. The DLG values decreased by an average of 6.9% and 5.9% after mechanical MLC adjustment. Although the passing rates increased slightly, by 1.5% (relative) and 1.2% (absolute) in arc 1, the average passing rates were still within the good dose delivery level (>95%). Our study shows the existence of a mechanical leaf gap error caused by a degenerated MLC motor. This can be recovered by reinitialization of MLC position on the machine control panel. Consequently, the QA procedure should be performed regularly to protect the MLC system.
MeSH Terms
Figure
Reference
-
References
1. LoSasso T, Chui CS, Ling CC. Physical and dosimetric aspects of a multileaf collimation system used in the dynamic mode for implementing intensity modulated radiotherapy. Med Phys. 1998; 25:1919–27.
Article2. Arnfield MR, Siebers JV, Kim JO, Wu Q, Keall PJ, Mohan R. A method for determining multileaf collimator transmission and scatter for dynamic intensity modulated radiotherapy. Med Phys. 2000; 27:2231–41.
Article3. Xia P, Verhey LJ. Delivery systems of intensitymodulated radiotherapy using conventional multileaf collimators. Med Dosim. 2001; 26:169–77.
Article4. Butson MJ, Yu PK, Cheung T. Rounded end multileaf penumbral measurements with radiochromic film. Phys Med Biol. 2003; 48:247–52.
Article5. Shende R, Patel G. Validation of Dosimetric Leaf Gap (DLG) prior to its implementation in Treatment Planning System (TPS): TrueBeamTM millennium 120 leaf MLC. Rep Pract Oncol Radiother. 2017; 22:485–494.6. Vial P, et al. An experimental investigation into the radiation field offset of a dynamic multileaf collimator. Phys Med Biol. 2006; 51:5517.
Article7. Mei X, Nygren I, Villarreal-Barajas JE. On the use of the MLC dosimetric leaf gap as a quality control tool for accurate dynamic IMRT delivery. Med Phys. 2011; 38:2246.
Article8. Shende R, et al. Commissioning of TrueBeamTM medical linear accelerator: quantitative and qualitative dosimetric analysis and comparison of flattening filter (FF) and FLATTENING FILTER FRee (FFF) beam. Int J Med Phys Clin Engi Radiat Oncol. 2016; 5:1.9. Vial P, Hunt P, Greer PB, Oliver L, Baldock C. Software tool for portal dosimetry research. Australas Phys Eng Sci Med. 2008; 31:216–22.
Article10. Herman MG, Kruse JJ, Hagness CR. Guide to clinical use of electronic portal imaging. J Appl Clin Med Phys. 2000; 1(2):38–57.
Article11. Low DA, Harms WB, Mutic S, Purdy JA. A technique for the quantitative evaluation of dose distributions. Med Phys. 1998; 25:656–61.
Article12. Sharma DS, Mhatre V, Heigrujam M, Talapatra K, Mallik S. Portal dosimetry for pretreatment verification of IMRT plan: a comparison with 2D ion chamberarray. J Appl Clin Med Phys. 2010; 11:3268.13. Clemente S, et al. To evaluate the accuracy of dynamic versus static IMRT delivery using portal dosimetry. Clin Transl Oncol. 2014; 16:208–12.
Article14. Chang Z, et al. Commissioning and dosimetric character-istics of TrueBeam system: composite data of three TrueBeam machines. Med Phys. 2012; 39:6981–7018.
Article15. Agnew A, Agnew CE, Grattan MW, Hounsell AR, McGarry CK. Monitoring daily MLC positional errors using trajectory log files and EPID measurements for IMRT and VMAT deliveries. Phys Med Biol. 2014; 59:49–63.
Article16. Asmerom G, et al. The design and physical characterization of a multileaf collimator for robotic radiosurgery. Biomed. Phys. Eng. Express 2. 2016. 017003.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Development of an Instantaneously Interpretable Real-Time Dosimeter System for Quality Assurance of a Medical Linear Accelerator
- Segmental Analysis Trial of Volumetric Modulated Arc Therapy for Quality Assurance of Linear Accelerator
- Dosimetric Effect on Selectable Optimization Parameters of Volumatric Modulated Arc Therapy
- A Verification for Multiple Arc Stereotaxic Radiotherapy
- Evaluation of Dosimetric Leaf Gap (DLG) at Different Depths for Dynamic IMRT