J Cardiovasc Imaging.
2018 Jun;26(2):65-74. 10.4250/jcvi.2018.26.e1.
Epicardial Fat Thickness and Free Fatty Acid Level are Predictors of Acute Ischemic Stroke with Atrial Fibrillation
- Affiliations
-
- 1Department of Cardiology, Kosin University College of Medicine, Busan, Korea.
- 2Department of Statistics and Actuarial Science, Soongsil University, Seoul, Korea.
- 3Department of Neurology, Kosin University College of Medicine, Busan, Korea. ybg99@naver.com
- KMID: 2415456
- DOI: http://doi.org/10.4250/jcvi.2018.26.e1
Abstract
- BACKGROUND
Increased epicardial fat is known to be associated with the presence and chronicity of atrial fibrillation (AF). Free fatty acids (FFAs) are major components of epicardial fat; however, their potential association with AF in ischemic stroke has not been investigated. We aimed to assess the performance of echocardiographic epicardial fat thickness (EFT) and plasma FFA level in identifying patients with ischemic stroke and AF.
METHODS
We enrolled a total of 214 consecutive patients (mean age, 66.8 ± 12.3 years; 39.7% women) diagnosed with acute ischemic stroke between March 2011 and June 2014. The patients were divided into two groups: ischemic stroke with AF (n = 35, 16.4%) and ischemic stroke without AF (n = 179, 83.6%).
RESULTS
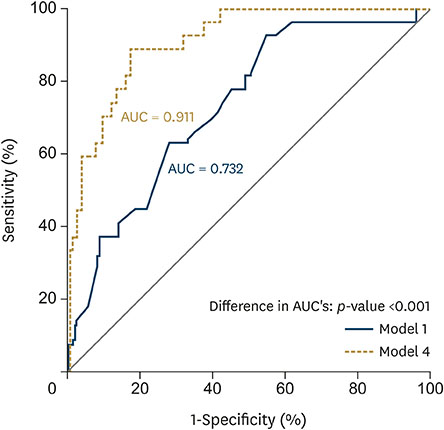
The ischemic stroke with AF group showed significantly higher serum FFA level (1379.7 ± 717.5 vs. 757.8 ± 520.5 uEq/L, p < 0.0001) and EFT (6.5 ± 1.2 vs. 5.3 ± 1.2 mm, p < 0.001) than the group without AF. Multivariable logistic regression analysis demonstrated that age (odds ratio [OR], 1.112), serum FFA level (OR, 1.002), and EFT (OR, 1.740) were independently associated with the ischemic stroke group with AF. EFT and FFA significantly improved the goodness-of-fit and discriminability of the simple regression model including age as a covariate (log likelihood difference, 21.35; p < 0.001; c-index difference, 17.9%; p < 0.001).
CONCLUSIONS
High EFT and serum FFA level were associated with ischemic stroke in patients with AF. Echocardiographic EFT and serum FFA level can play a significant role in identifying ischemic stroke with AF.
MeSH Terms
Figure
Cited by 1 articles
-
Epicardial Fat Thickness, Free Fatty Acid Can Predict Acute Ischemic Stroke in Patients with Atrial Fibrillation?
Kyung-Hee Kim
J Cardiovasc Imaging. 2018;26(2):63-64. doi: 10.4250/jcvi.2018.26.e8.
Reference
-
1. Kim BJ, Kim JS. Ischemic stroke subtype classification: an asian viewpoint. J Stroke. 2014; 16:8–17.
Article2. Sanak D, Hutyra M, Kral M, et al. Paroxysmal atrial fibrillation in young cryptogenic ischemic stroke: A 3-week ECG Holter monitoring study. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub. 2015; 159:283–287.
Article3. Mozaffarian D, Benjamin EJ, Go AS, American Heart Association Statistics Committee and Stroke Statistics Subcommittee, et al. Heart disease and stroke statistics--2015 update: a report from the American Heart Association. Circulation. 2015; 131:e29–e322.4. Tsang TS, Petty GW, Barnes ME, et al. The prevalence of atrial fibrillation in incident stroke cases and matched population controls in Rochester, Minnesota: changes over three decades. J Am Coll Cardiol. 2003; 42:93–100.5. Grau AJ, Weimar C, Buggle F, et al. Risk factors, outcome, and treatment in subtypes of ischemic stroke: the German stroke data bank. Stroke. 2001; 32:2559–2566.
Article6. Gage BF, Waterman AD, Shannon W, Boechler M, Rich MW, Radford MJ. Validation of clinical classification schemes for predicting stroke: results from the National Registry of Atrial Fibrillation. JAMA. 2001; 285:2864–2870.
Article7. European Heart Rhythm Association; European Association for Cardio-Thoracic Surgery, Camm AJ, Kirchhof P, Lip GY, et al. Guidelines for the management of atrial fibrillation: the Task Force for the Management of Atrial Fibrillation of the European Society of Cardiology (ESC). Eur Heart J. 2010; 31:2369–2429.8. Khawaja O, Bartz TM, Ix JH, et al. Plasma free fatty acids and risk of atrial fibrillation (from the Cardiovascular Health Study). Am J Cardiol. 2012; 110:212–216.
Article9. Djoussé L, Benkeser D, Arnold A, et al. Plasma free fatty acids and risk of heart failure: the Cardiovascular Health Study. Circ Heart Fail. 2013; 6:964–969.10. Al Chekakie MO, Welles CC, Metoyer R, et al. Pericardial fat is independently associated with human atrial fibrillation. J Am Coll Cardiol. 2010; 56:784–788.
Article11. Ouchi N. Obesity: Progress in diagnosis and treatment; Topics, IV. Recent topics; 3. Obesity and new secretory factors; 2) Sfrp 5 acts as a novel adipocytokine that affects metabolic function. Nihon Naika Gakkai Zasshi. 2011; 100:1002–1007.12. Chhabra L, Spodick DH. Role of epicardial fat in atrial fibrillation after coronary artery bypass surgery. Am J Cardiol. 2014; 113:2090.
Article13. Hendrickson SC, St Louis JD, Lowe JE, Abdel-aleem S. Free fatty acid metabolism during myocardial ischemia and reperfusion. Mol Cell Biochem. 1997; 166:85–94.14. Mazzali G, Fantin F, Zoico E, et al. Heart fat infiltration in subjects with and without coronary artery disease. J Clin Endocrinol Metab. 2015; 100:3364–3371.
Article15. Pantanowitz L. Fat infiltration in the heart. Heart. 2001; 85:253.
Article16. Lin YK, Chen YC, Chen JH, Chen SA, Chen YJ. Adipocytes modulate the electrophysiology of atrial myocytes: implications in obesity-induced atrial fibrillation. Basic Res Cardiol. 2012; 107:293.
Article17. Abed HS, Samuel CS, Lau DH, et al. Obesity results in progressive atrial structural and electrical remodeling: implications for atrial fibrillation. Heart Rhythm. 2013; 10:90–100.
Article18. Hirata Y, Yamada H, Kusunose K, et al. Clinical utility of measuring epicardial adipose tissue thickness with echocardiography using a high-frequency linear probe in patients with coronary artery disease. J Am Soc Echocardiogr. 2015; 28:1240–1246.e1.
Article19. Tok D, Çağli K, Kadife I, et al. Impaired coronary flow reserve is associated with increased echocardiographic epicardial fat thickness in metabolic syndrome patients. Coron Artery Dis. 2013; 24:191–195.
Article20. Kim BJ, Kim BS, Kang JH. Echocardiographic epicardial fat thickness is associated with arterial stiffness. Int J Cardiol. 2013; 167:2234–2238.
Article21. Kim BJ, Kim BS, Kang JH. Echocardiographic epicardial fat thickness is associated with coronary artery calcification - results from the CAESAR study. Circ J. 2015; 79:818–824.22. Sengul C, Cevik C, Ozveren O, et al. Echocardiographic epicardial fat thickness is associated with carotid intima-media thickness in patients with metabolic syndrome. Echocardiography. 2011; 28:853–858.
Article23. Stojanovska J, Kazerooni EA, Sinno M, et al. Increased epicardial fat is independently associated with the presence and chronicity of atrial fibrillation and radiofrequency ablation outcome. Eur Radiol. 2015; 25:2298–2309.
Article24. Adams HP Jr, Bendixen BH, Kappelle LJ, et al. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke. 1993; 24:35–41.
Article25. Oh MS, Yu KH, Lee JH, et al. Validity and reliability of a Korean version of the national institutes of health stroke scale. J Clin Neurol. 2012; 8:177–183.
Article26. Bonita R, Beaglehole R. Recovery of motor function after stroke. Stroke. 1988; 19:1497–1500.
Article27. Levy D, Savage DD, Garrison RJ, Anderson KM, Kannel WB, Castelli WP. Echocardiographic criteria for left ventricular hypertrophy: the Framingham Heart Study. Am J Cardiol. 1987; 59:956–960.
Article28. Shim IK, Cho KI, Kim HS, Heo JH, Cha TJ. Impact of gender on the association of epicardial fat thickness, obesity, and circadian blood pressure pattern in hypertensive patients. J Diabetes Res. 2015; 2015:924539.
Article29. Harrell FE Jr, Califf RM, Pryor DB, Lee KL, Rosati RA. Evaluating the yield of medical tests. JAMA. 1982; 247:2543–2546.
Article30. DeLong ER, DeLong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics. 1988; 44:837–845.
Article31. Acet H, Ertaş F, Akıl MA, et al. New inflammatory predictors for non-valvular atrial fibrillation: echocardiographic epicardial fat thickness and neutrophil to lymphocyte ratio. Int J Cardiovasc Imaging. 2014; 30:81–89.
Article32. Soeki T, Sata M. Role of epicardial adipose tissue in atrial fibrillation. Circ J. 2012; 76:2738–2739.
Article33. Spence JD. Free fatty acids and stroke from atrial fibrillation. Can J Neurol Sci. 2011; 38:803.
Article34. Jickling GC, Spence JD. Free fatty acids to predict recurrent ischemic stroke. Neurology. 2014; 82:1110–1111.
Article35. Seo WK, Kim J, Kim YH, et al. Elevated free fatty acid is associated with cardioembolic stroke subtype. Can J Neurol Sci. 2011; 38:874–879.
Article36. Choi JY, Jung JM, Kwon DY, et al. Free fatty acid as an outcome predictor of atrial fibrillation-associated stroke. Ann Neurol. 2016; 79:317–325.
Article37. Koutsari C, Dumesic DA, Patterson BW, Votruba SB, Jensen MD. Plasma free fatty acid storage in subcutaneous and visceral adipose tissue in postabsorptive women. Diabetes. 2008; 57:1186–1194.
Article38. O'Connell RP, Musa H, Gomez MS, et al. Free fatty acid effects on the atrial myocardium: membrane ionic currents are remodeled by the disruption of T-tubular architecture. PLoS One. 2015; 10:e0133052.39. Petrovičová A, Kurča E, Brozman M, et al. Detection of occult paroxysmal atrial fibrilation by implantable long-term electrocardiographic monitoring in cryptogenic stroke and transient ischemic attack population: a study protocol for prospective matched cohort study. BMC Cardiovasc Disord. 2015; 15:160.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Epicardial Fat Thickness, Free Fatty Acid Can Predict Acute Ischemic Stroke in Patients with Atrial Fibrillation?
- The Mechanism of and Preventive Therapy for Stroke in Patients with Atrial Fibrillation
- Non-medication Treatment of Atrial Fibrillation
- Relation of Stroke Risk Factors to Severity and Disability after Ischemic Stroke
- Echocardiographic Epicardial Fat Thickness on Short Term Prognosis in Patients with Acute Coronary Syndrome