J Clin Neurol.
2018 Jul;14(3):283-290. 10.3988/jcn.2018.14.3.283.
Patterns of Orthostatic Blood Pressure Changes in Patients with Orthostatic Hypotension
- Affiliations
-
- 1Department of Neurology, Korea University Medical Center, Korea University College of Medicine, Seoul, Korea. nukbj@korea.ac.kr
- 2Department of Neurology, Keimyung University School of Medicine, Daegu, Korea.
- 3Department of Neurology, Hangang Sacred Heart Hospital, Hallym University Medical Center, Seoul, Korea.
- KMID: 2415042
- DOI: http://doi.org/10.3988/jcn.2018.14.3.283
Abstract
- BACKGROUND AND PURPOSE
The objective of this study was to determine the patterns of blood pressure (BP) changes during the head-up tilt (HUT) test, particularly in terms of its clinical significance for patients with orthostatic hypotension (OH).
METHODS
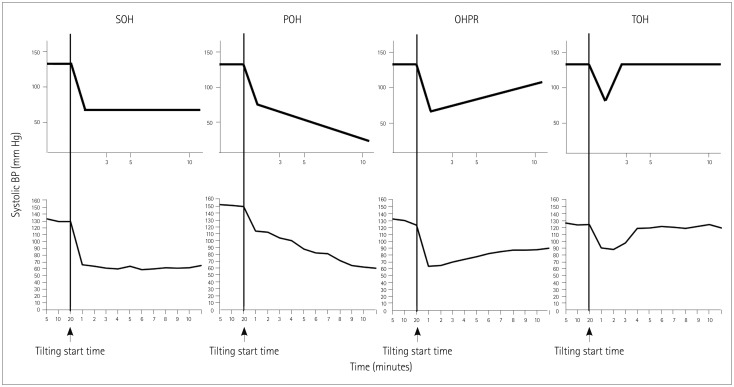
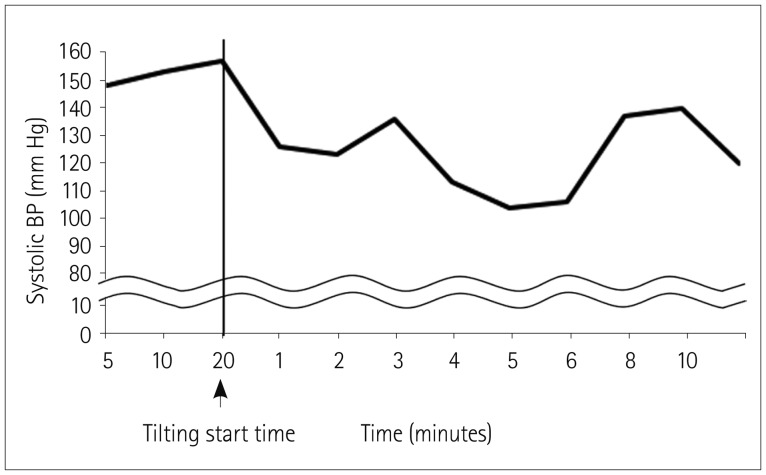
OH was divided into four categories based on systolic BP changes occurring within the first 10 minutes of the HUT test: sustained orthostatic hypotension (SOH), progressive orthostatic hypotension (POH), orthostatic hypotension with partial recovery (OHPR), and transient orthostatic hypotension (TOH).
RESULTS
In total, 151 patients were analyzed: 65 with SOH, 38 with POH, 21 with OHPR, and 27 with TOH. POH patients exhibited the greatest reduction in systolic BP after HUT and were also the most likely to develop symptoms requiring early termination of the HUT test (42.1%, p < 0.001). Additionally, SOH patients exhibited smaller heart-rate variation with deep breathing values (p=0.003) and Valsalva ratios (p=0.022) compared to POH patients. The sweat volume was greatest in OHPR patients.
CONCLUSIONS
Clinical characteristics, including the findings of autonomic function tests, differed between the OH patient groups. This might reflect differences in the underlying pathophysiologic mechanisms. Determining the patterns of BP changes during the HUT test may facilitate the development of effective management strategies in patients with OH.
MeSH Terms
Figure
Reference
-
1. Low PA, Tomalia VA. Orthostatic hypotension: mechanisms, causes, management. J Clin Neurol. 2015; 11:220–226. PMID: 26174784.
Article2. Freeman R, Wieling W, Axelrod FB, Benditt DG, Benarroch E, Biaggioni I, et al. Consensus statement on the definition of orthostatic hypotension, neurally mediated syncope and the postural tachycardia syndrome. Clin Auton Res. 2011; 21:69–72. PMID: 21431947.
Article3. Frith J. Diagnosing orthostatic hypotension: a narrative review of the evidence. Br Med Bull. 2015; 115:123–134. PMID: 25995335.
Article4. Low PA, Singer W. Management of neurogenic orthostatic hypotension: an update. Lancet Neurol. 2008; 7:451–458. PMID: 18420158.
Article5. Metzler M, Duerr S, Granata R, Krismer F, Robertson D, Wenning GK. Neurogenic orthostatic hypotension: pathophysiology, evaluation, and management. J Neurol. 2013; 260:2212–2219. PMID: 23180176.
Article6. Naschitz JE, Rosner I. Orthostatic hypotension: framework of the syndrome. Postgrad Med J. 2007; 83:568–574. PMID: 17823222.
Article7. Kim JB, Hong S, Park JW, Cho DH, Park KJ, Kim BJ. Utility of corrected QT interval in orthostatic intolerance. PLoS One. 2014; 9:e106417. PMID: 25180969.
Article8. Gehrking JA, Hines SM, Benrud-Larson LM, Opher-Gehrking TL, Low PA. What is the minimum duration of head-up tilt necessary to detect orthostatic hypotension. Clin Auton Res. 2005; 15:71–75. PMID: 15834762.
Article9. Naschitz JE, Elias N, Slobodin G, Storch S, Rosner I. Predicting outcomes on head-up tilt based on orthostatic hypotension patterns. J Hypertens. 2006; 24:1033–1039. PMID: 16685202.
Article10. Kim HA, Yi HA, Lee H. Spectrum of autonomic dysfunction in orthostatic dizziness. Clin Neurophysiol. 2014; 125:1248–1254. PMID: 24268815.
Article11. Gibbons CH, Schmidt P, Biaggioni I, Frazier-Mills C, Freeman R, Isaacson S, et al. The recommendations of a consensus panel for the screening, diagnosis, and treatment of neurogenic orthostatic hypotension and associated supine hypertension. J Neurol. 2017; 264:1567–1582. PMID: 28050656.
Article12. Kim JB, Kim BJ, Koh SB, Park KW. Autonomic dysfunction according to disease progression in Parkinson's disease. Parkinsonism Relat Disord. 2014; 20:303–307. PMID: 24382402.
Article13. Baek SH, Seok HY, Koo YS, Kim BJ. Lengthened cutaneous silent period in fibromyalgia suggesting central sensitization as a pathogenesis. PLoS One. 2016; 11:e0149248. PMID: 26871583.
Article14. Low PA, Denq JC, Opfer-Gehrking TL, Dyck PJ, O'Brien PC, Slezak JM. Effect of age and gender on sudomotor and cardiovagal function and blood pressure response to tilt in normal subjects. Muscle Nerve. 1997; 20:1561–1568. PMID: 9390669.
Article15. Low PA. Autonomic nervous system function. J Clin Neurophysiol. 1993; 10:14–27. PMID: 8458992.
Article16. Deegan BM, O'Connor M, Donnelly T, Carew S, Costelloe A, Sheehy T, et al. Orthostatic hypotension: a new classification system. Europace. 2007; 9:937–941. PMID: 17720979.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Orthostatic Intolerance Syndrome
- Diagnostic approach of orthostatic dizziness/vertigo
- Risk Factors of Orthostatic Hypotension among the Long-term Hospitalized Elderly Patients
- Prevalence and Risk Factors of Orthostatic Hypotension among the Community-Dwelling Aged
- Diagnosis and management of neurogenic orthostatic hypotension