Korean Circ J.
2018 May;48(5):406-417. 10.4070/kcj.2017.0328.
Effect of Non-vitamin K Antagonist Oral Anticoagulants in Atrial Fibrillation Patients with Newly Diagnosed Cancer
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine, Severance Cardiovascular Hospital, Yonsei University College of Medicine, Seoul, Korea. cby6908@yuhs.ac
- KMID: 2414909
- DOI: http://doi.org/10.4070/kcj.2017.0328
Abstract
- BACKGROUND AND OBJECTIVES
There are limited data on the use of non-vitamin K antagonist oral anticoagulants (NOACs) in atrial fibrillation (AF) patients with cancer. We aimed to assess the efficacy and safety of NOACs in AF patients with cancer in this study.
METHODS
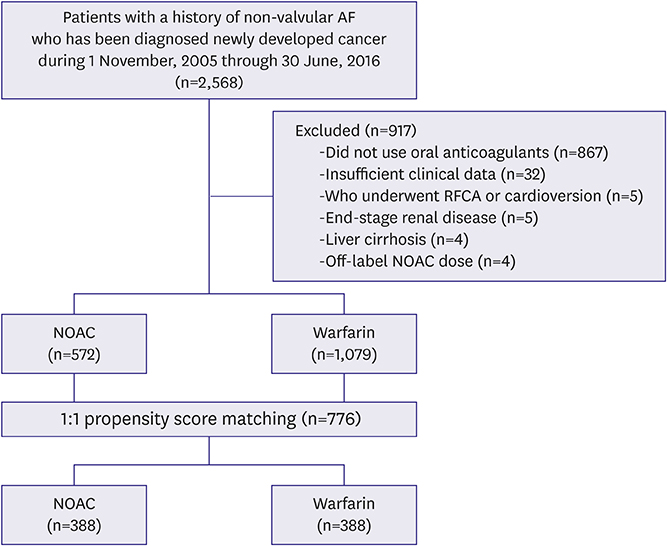
In 2,568 consecutive non-valvular AF patients with newly diagnosed cancer, we analyzed ischemic stroke/systemic embolism (SE), major bleeding, and all-cause death. Based on propensity score matching, 388 matched pairs were included in the NOAC and warfarin groups.
RESULTS
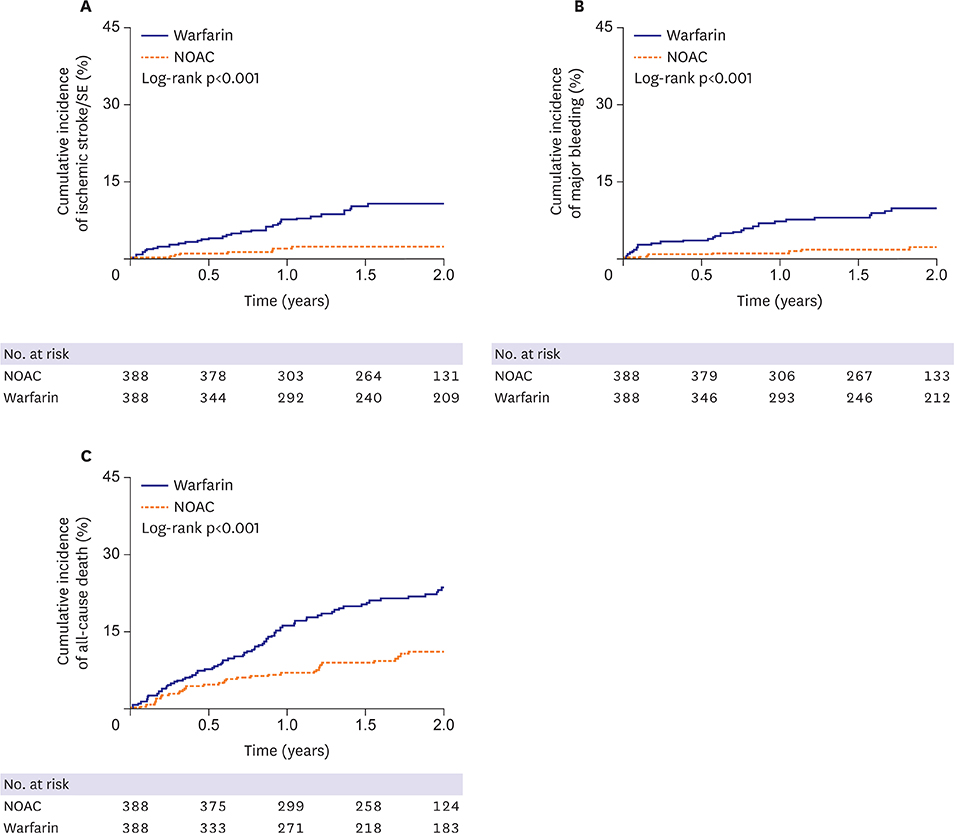
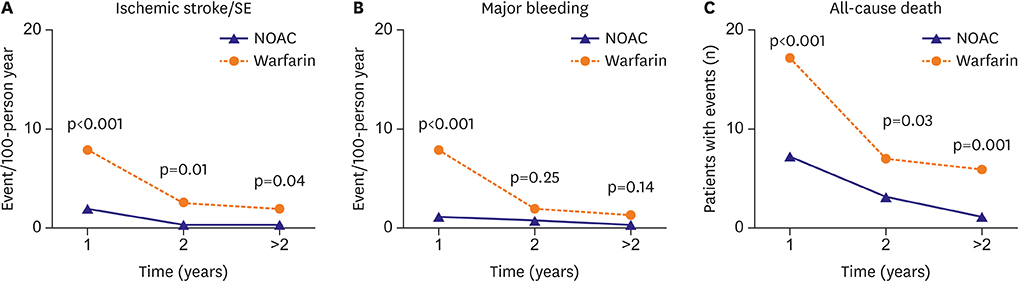
Patient baseline characteristics were comparable between the matched groups. During median follow-up of 1.8 years, the NOAC group had significantly lower incidences of ischemic stroke/SE (p < 0.001), major bleeding (p < 0.001), and all-cause death (p < 0.001) than the warfarin group. Moreover, the incidence of major bleeding was significantly lower in the NOAC group than in the warfarin group with optimal international normalized ratio control (p=0.03). Especially, within 1 year after cancer diagnosis, the incidences of all clinical events were significantly lower in the NOAC group than in the warfarin group.
CONCLUSIONS
In AF patients with newly diagnosed cancer, NOACs showed lower incidences of ischemic stroke/SE, major bleeding, and all-cause death than warfarin, especially within 1 year after cancer diagnosis.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
Oral Anticoagulants for Atrial Fibrillation Patients with Active Cancer
Do Young Kim, Hong Euy Lim
Korean Circ J. 2018;48(5):433-434. doi: 10.4070/kcj.2018.0081.Cancer-Associated Stroke: Thrombosis Mechanism, Diagnosis, Outcome, and Therapeutic Strategies
Ji Hoe Heo, Jaeseob Yun, Kwang Hyun Kim, Jae Wook Jung, Joonsang Yoo, Young Dae Kim, Hyo Suk Nam
J Stroke. 2024;26(2):164-178. doi: 10.5853/jos.2023.03279.
Reference
-
1. Go AS, Hylek EM, Phillips KA, et al. Prevalence of diagnosed atrial fibrillation in adults: national implications for rhythm management and stroke prevention: the AnTicoagulation and Risk Factors in Atrial Fibrillation (ATRIA) Study. JAMA. 2001; 285:2370–2375.2. Kim TH, Yang PS, Uhm JS, et al. CHA2DS2-VASc score (congestive heart failure, hypertension, age ≥75 [doubled], diabetes mellitus, prior stroke or transient ischemic attack [doubled], vascular disease, age 65–74, female) for stroke in Asian patients with atrial fibrillation: a Korean nationwide sample cohort study. Stroke. 2017; 48:1524–1530.3. Furie KL, Kasner SE, Adams RJ, et al. Guidelines for the prevention of stroke in patients with stroke or transient ischemic attack: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2011; 42:227–276.
Article4. Lee SJ, Uhm JS, Kim JY, Pak HN, Lee MH, Joung B. The safety and efficacy of vitamin K antagonist in patients with atrial fibrillation and liver cirrhosis. Int J Cardiol. 2015; 180:185–191.
Article5. Lee YJ, Park JK, Uhm JS, et al. Bleeding risk and major adverse events in patients with cancer on oral anticoagulation therapy. Int J Cardiol. 2016; 203:372–378.
Article6. O'Neal WT, Lakoski SG, Qureshi W, et al. Relation between cancer and atrial fibrillation (from the REasons for Geographic and Racial Differences in Stroke Study). Am J Cardiol. 2015; 115:1090–1094.7. Guzzetti S, Costantino G, Vernocchi A, Sada S, Fundarò C. First diagnosis of colorectal or breast cancer and prevalence of atrial fibrillation. Intern Emerg Med. 2008; 3:227–231.
Article8. Ostenfeld EB, Erichsen R, Pedersen L, Farkas DK, Weiss NS, Sørensen HT. Atrial fibrillation as a marker of occult cancer. PLoS One. 2014; 9:e102861.
Article9. Lanas A, García-Rodríguez LA, Arroyo MT, et al. Risk of upper gastrointestinal ulcer bleeding associated with selective cyclo-oxygenase-2 inhibitors, traditional non-aspirin non-steroidal anti-inflammatory drugs, aspirin and combinations. Gut. 2006; 55:1731–1738.
Article10. Kirchhof P, Benussi S, Kotecha D, et al. 2016 ESC guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur Heart J. 2016; 37:2893–2962.11. Dentali F, Riva N, Crowther M, Turpie AG, Lip GY, Ageno W. Efficacy and safety of the novel oral anticoagulants in atrial fibrillation: a systematic review and meta-analysis of the literature. Circulation. 2012; 126:2381–2391.12. Mani H, Lindhoff-Last E. New oral anticoagulants in patients with nonvalvular atrial fibrillation: a review of pharmacokinetics, safety, efficacy, quality of life, and cost effectiveness. Drug Des Devel Ther. 2014; 8:789–798.
Article13. Connolly SJ, Ezekowitz MD, Yusuf S, et al. Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med. 2009; 361:1139–1151.
Article14. Lip GY, Edwards SJ. Stroke prevention with aspirin, warfarin and ximelagatran in patients with non-valvular atrial fibrillation: a systematic review and meta-analysis. Thromb Res. 2006; 118:321–333.
Article15. Cowie MR, Struthers AD, Wood DA, et al. Value of natriuretic peptides in assessment of patients with possible new heart failure in primary care. Lancet. 1997; 350:1349–1353.
Article16. Pisters R, Lane DA, Nieuwlaat R, de Vos CB, Crijns HJ, Lip GY. A novel user-friendly score (HAS-BLED) to assess 1-year risk of major bleeding in patients with atrial fibrillation: the Euro Heart Survey. Chest. 2010; 138:1093–1100.17. Rosendaal FR, Cannegieter SC, van der Meer FJ, Briët E. A method to determine the optimal intensity of oral anticoagulant therapy. Thromb Haemost. 1993; 69:236–239.
Article18. Cockcroft DW, Gault MH. Prediction of creatinine clearance from serum creatinine. Nephron. 1976; 16:31–41.
Article19. Jauch EC, Saver JL, Adams HP Jr, et al. Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2013; 44:870–947.20. Schulman S, Kearon C. Subcommittee on Control of Anticoagulation of the Scientific and Standardization Committee of the International Society on Thrombosis and Haemostasis. Definition of major bleeding in clinical investigations of antihemostatic medicinal products in non-surgical patients. J Thromb Haemost. 2005; 3:692–694.
Article21. Austin PC. Some methods of propensity-score matching had superior performance to others: results of an empirical investigation and Monte Carlo simulations. Biom J. 2009; 51:171–184.
Article22. Cronin-Fenton DP, Søndergaard F, Pedersen LA, et al. Hospitalisation for venous thromboembolism in cancer patients and the general population: a population-based cohort study in Denmark, 1997–2006. Br J Cancer. 2010; 103:947–953.
Article23. Akao M, Chun YH, Esato M, et al. Inappropriate use of oral anticoagulants for patients with atrial fibrillation. Circ J. 2014; 78:2166–2172.
Article24. Rose AJ, Sharman JP, Ozonoff A, Henault LE, Hylek EM. Effectiveness of warfarin among patients with cancer. J Gen Intern Med. 2007; 22:997–1002.
Article25. Giugliano RP, Ruff CT, Braunwald E, et al. Edoxaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2013; 369:2093–2104.
Article26. Patel MR, Mahaffey KW, Garg J, et al. Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N Engl J Med. 2011; 365:883–891.
Article27. Granger CB, Alexander JH, McMurray JJ, et al. Apixaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2011; 365:981–992.28. Gómez-Outes A, Terleira-Fernández AI, Calvo-Rojas G, Suárez-Gea ML, Vargas-Castrillón E. Dabigatran, rivaroxaban, or apixaban versus warfarin in patients with nonvalvular atrial fibrillation: a systematic review and meta-analysis of subgroups. Thrombosis. 2013; 2013:640723.
Article29. Hori M, Matsumoto M, Tanahashi N, et al. Rivaroxaban vs. warfarin in Japanese patients with atrial fibrillation – the J-ROCKET AF study –. Circ J. 2012; 76:2104–2111.30. Chan YH, Kuo CT, Yeh YH, et al. Thromboembolic, bleeding, and mortality risks of rivaroxaban and dabigatran in Asians with nonvalvular atrial fibrillation. J Am Coll Cardiol. 2016; 68:1389–1401.