Ann Dermatol.
2018 Apr;30(2):136-142. 10.5021/ad.2018.30.2.136.
A Study on Vitamin D and Cathelicidin Status in Patients with Rosacea: Serum Level and Tissue Expression
- Affiliations
-
- 1Department of Dermatology, Hallym University Sacred Heart Hospital, Anyang, Korea. dermakkh@naver.com
- 2Ilsong Institute of Life Science, Hallym University, Anyang, Korea.
- 3Department of Pathology, Hallym University Sacred Heart Hospital, Anyang, Korea.
- 4Department of Laboratory Medicine, Hallym University Sacred Heart Hospital, Anyang, Korea.
- 5Department of Plastic and Reconstructive Surgery, Hallym University Sacred Heart Hospital, Anyang, Korea.
- KMID: 2414673
- DOI: http://doi.org/10.5021/ad.2018.30.2.136
Abstract
- BACKGROUND
Rosacea is a chronic inflammatory disease characterized by centrofacial erythema. Excess cathelicidin is suggested to be important to the pathophysiology of the disease. Recently, presence of a vitamin D response element was revealed in the cathelicidin gene promoter.
OBJECTIVE
The aim of this study was to determine whether vitamin D and cathelicidin are associated with rosacea, both serologically and histopathologically.
METHODS
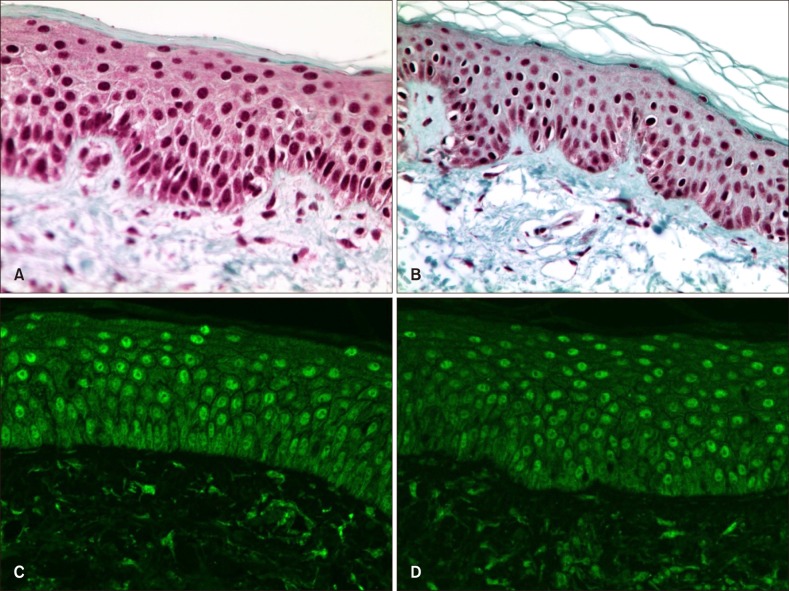
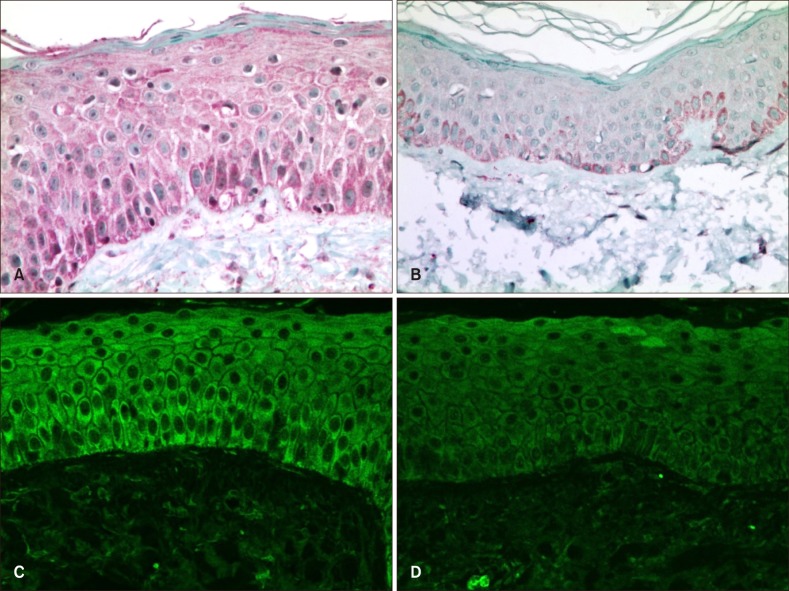
Subjects with rosacea and without chronic skin disorders were enrolled in the patient and control groups, respectively. Serum 25-hydroxy-vitamin D and cathelicidin levels were measured. Tissue expression of cathelicidin and vitamin D receptor were measured with immunostaining-intensity-distribution index.
RESULTS
The mean serum 25-hydroxyvitamin D level of patients with rosacea was 12.18±5.65 ng/ml, which is lower than that of the controls (17.41±6.75 ng/ml). Mean serum cathelicidin levels in patients with rosacea and the controls were 85.0±26.1 ng/ml and 55.0±23.3 ng/ml, respectively. Cathelicidin expression in rosacea tissue was significantly higher than that in control tissue (5.21 vs. 4.03). No significant difference was observed in vitamin D receptor expression.
CONCLUSION
Higher cathelicidin expression in rosacea supports the hypothesis that an abnormal inflammatory response of the innate immune system is important in pathogenesis of rosacea, but the role of high cathelicidin serum levels is complicated. Serum vitamin D was lower in patients with rosacea, although serum cathelicidin was higher than that of the controls. This suggests that the role of vitamin D level in the pathogenesis of rosacea merits further investigation.
Keyword
MeSH Terms
Figure
Reference
-
1. Yamasaki K, Di Nardo A, Bardan A, Murakami M, Ohtake T, Coda A, et al. Increased serine protease activity and cathelicidin promotes skin inflammation in rosacea. Nat Med. 2007; 13:975–980. PMID: 17676051.
Article2. Gombart AF, Borregaard N, Koeffler HP. Human cathelicidin antimicrobial peptide (CAMP) gene is a direct target of the vitamin D receptor and is strongly up-regulated in myeloid cells by 1,25-dihydroxyvitamin D3. FASEB J. 2005; 19:1067–1077. PMID: 15985530.3. Schauber J, Gallo RL. The vitamin D pathway: a new target for control of the skin's immune response? Exp Dermatol. 2008; 17:633–639. PMID: 18573153.
Article4. Two AM, Wu W, Gallo RL, Hata TR. Rosacea: part I. Introduction, categorization, histology, pathogenesis, and risk factors. J Am Acad Dermatol. 2015; 72:749–758. PMID: 25890455.5. Wilkin J, Dahl M, Detmar M, Drake L, Feinstein A, Odom R, et al. Standard classification of rosacea: report of the National Rosacea Society Expert Committee on the Classification and Staging of Rosacea. J Am Acad Dermatol. 2002; 46:584–587. PMID: 11907512.
Article6. Chaiyarit P, Kafrawy AH, Miles DA, Zunt SL, Van Dis ML, Gregory RL. Oral lichen planus: an immunohistochemical study of heat shock proteins (HSPs) and cytokeratins (CKs) and a unifying hypothesis of pathogenesis. J Oral Pathol Med. 1999; 28:210–215. PMID: 10226943.
Article7. Gennaro R, Zanetti M. Structural features and biological activities of the cathelicidin-derived antimicrobial peptides. Biopolymers. 2000; 55:31–49. PMID: 10931440.
Article8. Braff MH, Gallo RL. Antimicrobial peptides: an essential component of the skin defensive barrier. Curr Top Microbiol Immunol. 2006; 306:91–110. PMID: 16909919.
Article9. Braff MH, Hawkins MA, Di Nardo A, Lopez-Garcia B, Howell MD, Wong C, et al. Structure-function relationships among human cathelicidin peptides: dissociation of antimicrobial properties from host immunostimulatory activities. J Immunol. 2005; 174:4271–4278. PMID: 15778390.
Article10. Koczulla R, von Degenfeld G, Kupatt C, Krötz F, Zahler S, Gloe T, et al. An angiogenic role for the human peptide antibiotic LL-37/hCAP-18. J Clin Invest. 2003; 111:1665–1672. PMID: 12782669.
Article11. Mookherjee N, Brown KL, Bowdish DM, Doria S, Falsafi R, Hokamp K, et al. Modulation of the TLR-mediated inflammatory response by the endogenous human host defense peptide LL-37. J Immunol. 2006; 176:2455–2464. PMID: 16456005.
Article12. Steinhoff M, Schauber J, Leyden JJ. New insights into rosacea pathophysiology: a review of recent findings. J Am Acad Dermatol. 2013; 69(6 Suppl 1):S15–S26. PMID: 24229632.
Article13. Linde A, Lushington GH, Abello J, Melgarejo T. Clinical relevance of cathelicidin in infectious disease. J Clin Cell Immunol. 2013; S13:003.
Article14. Kanda N, Ishikawa T, Kamata M, Tada Y, Watanabe S. Increased serum leucine, leucine-37 levels in psoriasis: positive and negative feedback loops of leucine, leucine-37 and pro- or anti-inflammatory cytokines. Hum Immunol. 2010; 71:1161–1171. PMID: 20849904.
Article15. Kanda N, Watanabe S. Increased serum human β-defensin-2 levels in atopic dermatitis: relationship to IL-22 and oncostatin M. Immunobiology. 2012; 217:436–445. PMID: 22137028.
Article16. Yamasaki K, Kanada K, Macleod DT, Borkowski AW, Morizane S, Nakatsuji T, et al. TLR2 expression is increased in rosacea and stimulates enhanced serine protease production by keratinocytes. J Invest Dermatol. 2011; 131:688–697. PMID: 21107351.
Article17. Yamasaki K, Schauber J, Coda A, Lin H, Dorschner RA, Schechter NM, et al. Kallikrein-mediated proteolysis regulates the antimicrobial effects of cathelicidins in skin. FASEB J. 2006; 20:2068–2080. PMID: 17012259.
Article18. Yamasaki K, Gallo RL. Rosacea as a disease of cathelicidins and skin innate immunity. J Investig Dermatol Symp Proc. 2011; 15:12–15.
Article19. Liu PT, Stenger S, Li H, Wenzel L, Tan BH, Krutzik SR, et al. Toll-like receptor triggering of a vitamin D-mediated human antimicrobial response. Science. 2006; 311:1770–1773. PMID: 16497887.
Article20. Ekiz O, Balta I, Sen BB, Dikilitş MC, Ozuğuz P, Rifaioğlu EN. Vitamin D status in patients with rosacea. Cutan Ocul Toxicol. 2014; 33:60–62. PMID: 23713748.
Article21. Hata TR, Kotol P, Jackson M, Nguyen M, Paik A, Udall D, et al. Administration of oral vitamin D induces cathelicidin production in atopic individuals. J Allergy Clin Immunol. 2008; 122:829–831. PMID: 19014773.
Article22. Park K, Elias PM, Oda Y, Mackenzie D, Mauro T, Holleran WM, et al. Regulation of cathelicidin antimicrobial peptide expression by an endoplasmic reticulum (ER) stress signaling, vitamin D receptor-independent pathway. J Biol Chem. 2011; 286:34121–34130. PMID: 21832078.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Cathelicidin LL-37: An Antimicrobial Peptide with a Role in Inflammatory Skin Disease
- Increased Expression of Cathelicidin by Direct Activation of Protease-Activated Receptor 2: Possible Implications on the Pathogenesis of Rosacea
- Two Cases of Widespread Eczema Herpeticum with Low Serum Vitamin D Levels
- The Effect of Capsaicin on Neuroinflammatory Mediators of Rosacea
- Vitamin D-Cathelicidin Axis: at the Crossroads between Protective Immunity and Pathological Inflammation during Infection