J Gastric Cancer.
2018 Jun;18(2):182-188. 10.5230/jgc.2018.18.e20.
Learning Curve of Pure Single-Port Laparoscopic Distal Gastrectomy for Gastric Cancer
- Affiliations
-
- 1Department of Surgery, Seoul National University Bundang Hospital, Seongnam, Korea. viscaria@snubh.org
- 2Department of Surgery, Seoul National University College of Medicine, Seoul, Korea.
- KMID: 2414538
- DOI: http://doi.org/10.5230/jgc.2018.18.e20
Abstract
- PURPOSE
Despite the fact that there are several reports of single-port laparoscopic distal gastrectomy (SPDG), no analysis of its learning curve has been described in the literature. The aim of this study was to investigate the favorable factors for SPDG and to analyze the learning curve of SPDG.
MATERIALS AND METHODS
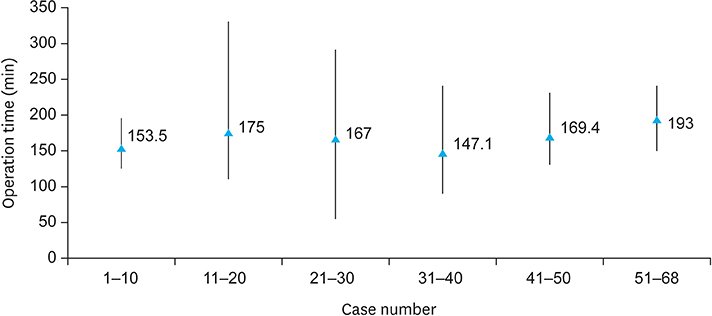
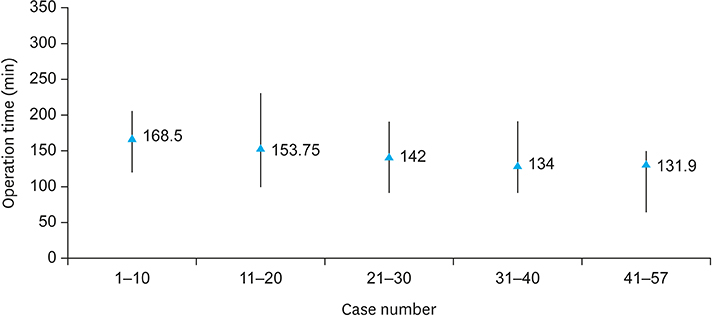
A total of 125 cases of SPDG performed from November 2011 to December 2015 were enrolled. All operations were performed by 2 surgeons (surgeon A and surgeon B). The moving average method was used for defining the learning curve. All cases were divided into 10 cases in a sequence, and the mean operative time and estimated blood loss data were extracted from each group.
RESULTS
Surgeon A performed 68 cases (female-to-male sex ratio, 91.1%:8.82%), and surgeon B performed 57 cases (female-to-male sex ratio, 61.4%:38.5%). The operative time of surgeon B significantly decreased after 30 cases (157.8±38.4 minutes vs. 118.1±34.5 minutes, P=0.003); that of surgeon A did not significantly decrease before and after around 30 cases (160.8±51.6 minutes vs. 173.3±35.2 minutes, P=0.6). The subgroup analysis showed that the operative time significantly decreased in the patients with body mass index (BMI) of < 25 kg/m2 ( < 25 kg/m2:≥25 kg/m2, 159.3±41.7 minutes: 194.25±81.1 minutes; P=0.001).
CONCLUSIONS
Although there was no significant decrease in the operative time for surgeon A, surgeon B reached the learning curve upon conducting 30 cases of SPDG. BMI of < 25 kg/m2 was found to be a favorable factor for SPDG.
Keyword
MeSH Terms
Figure
Reference
-
1. Kitano S, Maeo S, Shiraishi N, Shimoda K, Miyahara M, Bandoh T, et al. Laparoscopically assisted distal partial gastrectomy for early-stage gastric carcinomas. Surg Technol Int. 1995; IV:115–119.2. Kitano S, Shiraishi N, Uyama I, Sugihara K, Tanigawa N; Japanese Laparoscopic Surgery Study Group. A multicenter study on oncologic outcome of laparoscopic gastrectomy for early cancer in Japan. Ann Surg. 2007; 245:68–72.
Article3. Kim HH, Han SU, Kim MC, Hyung WJ, Kim W, Lee HJ, et al. Prospective randomized controlled trial (phase III) to comparing laparoscopic distal gastrectomy with open distal gastrectomy for gastric adenocarcinoma (KLASS 01). J Korean Surg Soc. 2013; 84:123–130.
Article4. Omori T, Oyama T, Akamatsu H, Tori M, Ueshima S, Nishida T. Transumbilical single-incision laparoscopic distal gastrectomy for early gastric cancer. Surg Endosc. 2011; 25:2400–2404.
Article5. Ahn SH, Son SY, Jung DH, Park DJ, Kim HH. Pure single-port laparoscopic distal gastrectomy for early gastric cancer: comparative study with multi-port laparoscopic distal gastrectomy. J Am Coll Surg. 2014; 219:933–943.
Article6. Kim SM, Ha MH, Seo JE, Kim JE, Choi MG, Sohn TS, et al. Comparison of single-port and reduced-port totally laparoscopic distal gastrectomy for patients with early gastric cancer. Surg Endosc. 2016; 30:3950–3957.
Article7. Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004; 240:205–213.8. Kim MC, Jung GJ, Kim HH. Learning curve of laparoscopy-assisted distal gastrectomy with systemic lymphadenectomy for early gastric cancer. World J Gastroenterol. 2005; 11:7508–7511.
Article9. Bracale U, Marzano E, Nastro P, Barone M, Cuccurullo D, Cutini G, et al. Side-to-side esophagojejunostomy during totally laparoscopic total gastrectomy for malignant disease: a multicenter study. Surg Endosc. 2010; 24:2475–2479.
Article10. Lee JH, Ahn SH, Park DJ, Kim HH, Lee HJ, Yang HK. Laparoscopic total gastrectomy with D2 lymphadenectomy for advanced gastric cancer. World J Surg. 2012; 36:2394–2399.
Article11. Zhang X, Tanigawa N. Learning curve of laparoscopic surgery for gastric cancer, a laparoscopic distal gastrectomy-based analysis. Surg Endosc. 2009; 23:1259–1264.
Article12. Chatzizacharias NA, Dajani K, Koong JK, Jah A. The role of the single incision laparoscopic approach in liver and pancreatic resectional surgery. Minim Invasive Surg. 2016; 2016:1454026.
Article13. Omori T, Fujiwara Y, Moon J, Sugimura K, Miyata H, Masuzawa T, et al. Comparison of single-incision and conventional multi-port laparoscopic distal gastrectomy with D2 lymph node dissection for gastric cancer: a propensity score-matched analysis. Ann Surg Oncol. 2016; 23:817–824.
Article14. Wakasugi M, Tei M, Omori T, Anno K, Mikami T, Tsukada R, et al. Single-incision laparoscopic surgery as a teaching procedure: a single-center experience of more than 2100 procedures. Surg Today. 2016; 46:1318–1324.
Article15. Katebi Kashi P, Rostaminia G, Javadian P, Iskandar G, Tabbarah R, Garg R, et al. Association between patient's BMI and uterine weight with feasibility of single-port robotic-assisted surgery in benign gynecology. J Minim Invasive Gynecol. 2015; 22:S25.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Transition from Conventional to Reduced-Port Laparoscopic Gastrectomy to Treat Gastric Carcinoma: a Single Surgeon's Experience from a Small-Volume Center
- Single-Port Laparoscopic Proximal Gastrectomy with Double Tract Reconstruction for Early Gastric Cancer: Report of a Case
- Single Port Gastrectomy for Gastric Cancer
- Totally Laparoscopic Distal Gastrectomy after Learning Curve Completion: Comparison with Laparoscopy-Assisted Distal Gastrectomy
- Evaluation of Reduced Port Laparoscopic Distal Gastrectomy Performed by a Novice Surgeon