J Gastric Cancer.
2013 Mar;13(1):26-33.
Totally Laparoscopic Distal Gastrectomy after Learning Curve Completion: Comparison with Laparoscopy-Assisted Distal Gastrectomy
- Affiliations
-
- 1Department Surgery, Postgraduate School of Medicine, Gyeongsang National University, Jinju, Korea. goodgsdr@gmail.com
- 2Gyeongnam Regional Cancer Center, Jinju, Korea.
- 3Institue of Health Sciences, Gyeongsang National University, Jinju, Korea.
Abstract
- PURPOSE
The aims are to: (i) display the multidimensional learning curve of totally laparoscopic distal gastrectomy, and (ii) verify the feasibility of totally laparoscopic distal gastrectomy after learning curve completion by comparing it with laparoscopy-assisted distal gastrectomy.
MATERIALS AND METHODS
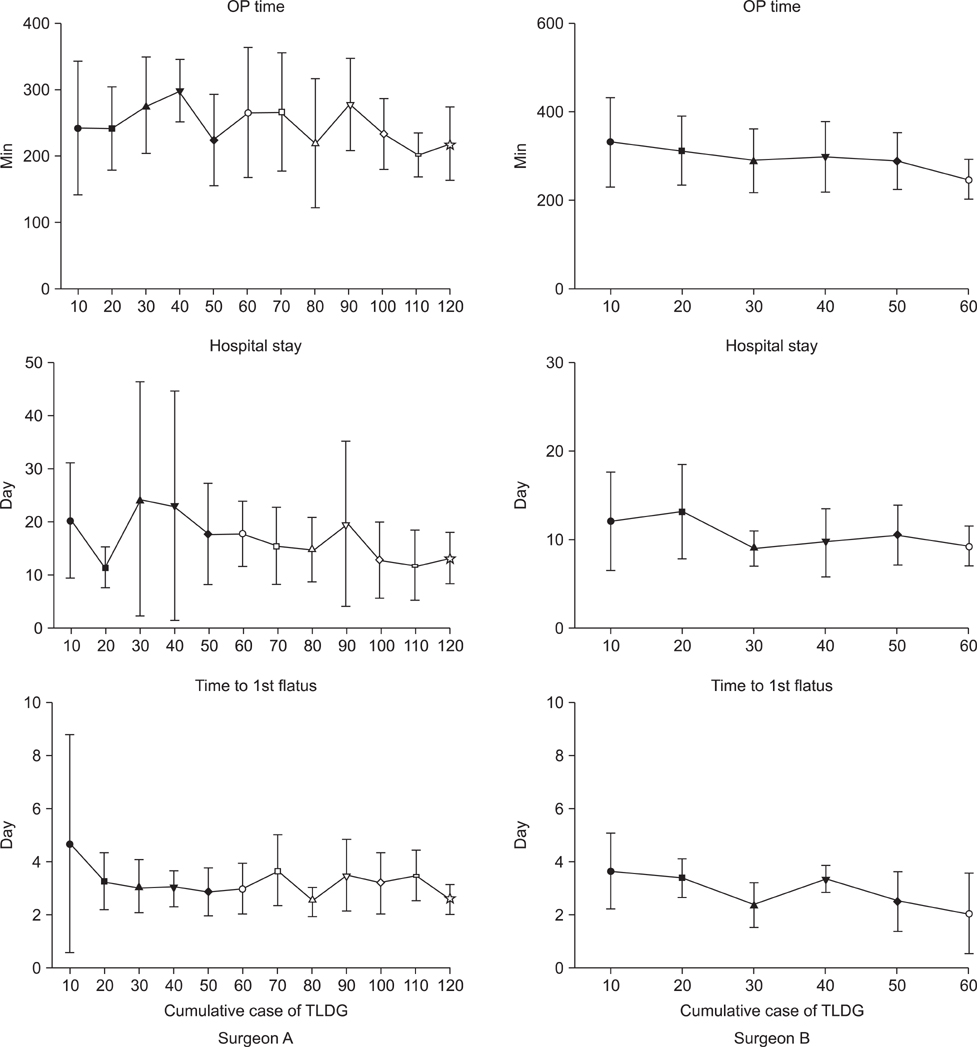
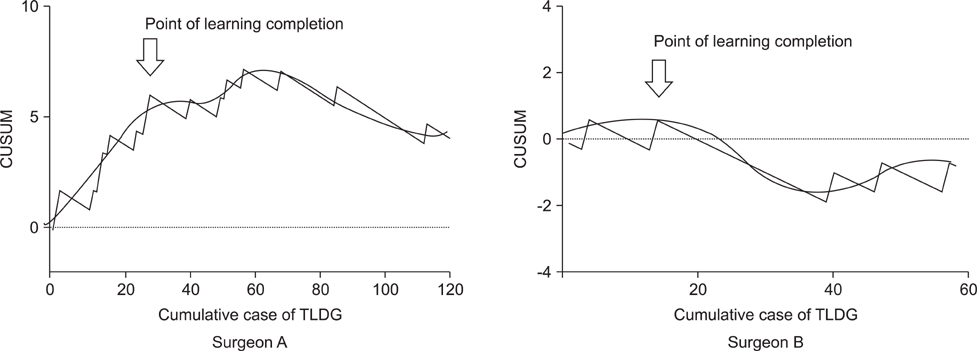
From January 2005 to June 2012, 247 patients who underwent laparoscopy-assisted distal gastrectomy (n=136) and totally laparoscopic distal gastrectomy (n=111) for early gastric cancer were enrolled. Their clinicopathological characteristics and early surgical outcomes were analyzed. Analysis of the totally laparoscopic distal gastrectomy learning curve was conducted using the moving average method and the cumulative sum method on 180 patients who underwent totally laparoscopic distal gastrectomy.
RESULTS
Our study indicated that experience with 40 and 20 totally laparoscopic distal gastrectomy cases, is required in order to achieve optimum proficiency by two surgeons. There were no remarkable differences in the clinicopathological characteristics between laparoscopy-assisted distal gastrectomy and totally laparoscopic distal gastrectomy groups. The two groups were comparable in terms of open conversion, combined resection, morbidities, reoperation rate, hospital stay and time to first flatus (P>0.05). However, totally laparoscopic distal gastrectomy had a significantly shorter mean operation time than laparoscopy-assisted distal gastrectomy (P<0.01). We also found that intra-abdominal abscess and overall complication rates were significantly higher before the learning curve than after the learning curve (P<0.05).
CONCLUSIONS
Experience with 20~40 cases of totally laparoscopic distal gastrectomy is required to complete the learning curve. The use of totally laparoscopic distal gastrectomy after learning curve completion is a feasible and timesaving method compared to laparoscopy-assisted distal gastrectomy.
Keyword
MeSH Terms
Figure
Reference
-
1. Kim HH, Hyung WJ, Cho GS, Kim MC, Han SU, Kim W, et al. Morbidity and mortality of laparoscopic gastrectomy versus open gastrectomy for gastric cancer: an interim report--a phase III multicenter, prospective, randomized Trial (KLASS Trial). Ann Surg. 2010. 251:417–420.
Article2. Kitano S, Shiraishi N, Uyama I, Sugihara K, Tanigawa N. Japanese Laparoscopic Surgery Study Group. A multicenter study on oncologic outcome of laparoscopic gastrectomy for early cancer in Japan. Ann Surg. 2007. 245:68–72.
Article3. Song KY, Park CH, Kang HC, Kim JJ, Park SM, Jun KH, et al. Is totally laparoscopic gastrectomy less invasive than laparoscopy-assisted gastrectomy?: prospective, multicenter study. J Gastrointest Surg. 2008. 12:1015–1021.
Article4. Hosogi H, Kanaya S. Intracorporeal anastomosis in laparoscopic gastric cancer surgery. J Gastric Cancer. 2012. 12:133–139.
Article5. Kim MG, Kawada H, Kim BS, Kim TH, Kim KC, Yook JH, et al. A totally laparoscopic distal gastrectomy with gastroduodenostomy (TLDG) for improvement of the early surgical outcomes in high BMI patients. Surg Endosc. 2011. 25:1076–1082.
Article6. Jin SH, Kim DY, Kim H, Jeong IH, Kim MW, Cho YK, et al. Multidimensional learning curve in laparoscopy-assisted gastrectomy for early gastric cancer. Surg Endosc. 2007. 21:28–33.
Article7. Kim MC, Jung GJ, Kim HH. Learning curve of laparoscopy-assisted distal gastrectomy with systemic lymphadenectomy for early gastric cancer. World J Gastroenterol. 2005. 11:7508–7511.
Article8. Fujiwara M, Kodera Y, Miura S, Kanyama Y, Yokoyama H, Ohashi N, et al. Laparoscopy-assisted distal gastrectomy with systemic lymph node dissection: a phase II study following the learning curve. J Surg Oncol. 2005. 91:26–32.
Article9. Zhang X, Tanigawa N. Learning curve of laparoscopic surgery for gastric cancer, a laparoscopic distal gastrectomy-based analysis. Surg Endosc. 2009. 23:1259–1264.
Article10. Novick RJ, Stitt LW. The learning curve of an academic cardiac surgeon: use of the CUSUM method. J Card Surg. 1999. 14:312–320.
Article11. Strasberg SM, Linehan DC, Hawkins WG. The accordion severity grading system of surgical complications. Ann Surg. 2009. 250:177–186.
Article12. Williams SM, Parry BR, Schlup MM. Quality control: an application of the cusum. BMJ. 1992. 304:1359–1361.
Article13. Edge SB, Compton CC. The American Joint Committee on Cancer: the 7th edition of the AJCC cancer staging manual and the future of TNM. Ann Surg Oncol. 2010. 17:1471–1474.
Article14. Japanese Gastric Cancer Association. Japanese classification of gastric carcinoma: 3rd English edition. Gastric Cancer. 2011. 14:101–112.15. Japanese Gastric Cancer Association. Japanese gastric cancer treatment guidelines 2010 (ver. 3). Gastric Cancer. 2011. 14:113–123.16. Joo YT, Moon HG, Lee SH, Jeong CY, Jung EJ, Hong SC, et al. Laparoscopy-assisted distal gastrectomy with intracorporeal Billroth I stapled anastomosis using a hand access device for patients with gastric cancer. Surg Endosc. 2007. 21:859–862.
Article17. Kanaya S, Gomi T, Momoi H, Tamaki N, Isobe H, Katayama T, et al. Delta-shaped anastomosis in totally laparoscopic Billroth I gastrectomy: new technique of intraabdominal gastroduodenostomy. J Am Coll Surg. 2002. 195:284–287.
Article18. Hyung WJ, Lim JS, Cheong JH, Kim J, Choi SH, Song SY, et al. Intraoperative tumor localization using laparoscopic ultrasonography in laparoscopic-assisted gastrectomy. Surg Endosc. 2005. 19:1353–1357.
Article19. Kim HI, Hyung WJ, Lee CR, Lim JS, An JY, Cheong JH, et al. Intraoperative portable abdominal radiograph for tumor localization: a simple and accurate method for laparoscopic gastrectomy. Surg Endosc. 2011. 25:958–963.
Article20. Tanimura S, Higashino M, Fukunaga Y, Osugi H. Laparoscopic distal gastrectomy with regional lymph node dissection for gastric cancer. Surg Endosc. 2003. 17:758–762.
Article21. Jeong O, Cho SB, Joo YE, Ryu SY, Park YK. Novel technique for intraoperative tumor localization during totally laparoscopic distal gastrectomy: endoscopic autologous blood tattooing. Surg Endosc. 2012. 26:1778–1783.
Article22. Jeong SH, Lee YJ, Bae K, Ha WS, Park ST, Choi SK, et al. Clinical factors affecting the length of minilaparotomy incision in laparoscopy-assisted distal gastrectomy. J Laparoendosc Adv Surg Tech A. 2009. 19:129–133.
Article23. Lee J, Kim D, Kim W. Comparison of laparoscopy-assisted and totally laparoscopic Billroth-II distal gastrectomy for gastric cancer. J Korean Surg Soc. 2012. 82:135–142.
Article24. Park DJ, Lee HJ, Kim HH, Yang HK, Lee KU, Choe KJ. Predictors of operative morbidity and mortality in gastric cancer surgery. Br J Surg. 2005. 92:1099–1102.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of laparoscopy-assisted and totally laparoscopic Billroth-II distal gastrectomy for gastric cancer
- Comparison of Laparoscopy-Assisted and Totally Laparoscopic Distal Gastrectomy: The Short-Term Outcome at a Low Volume Center
- Comparison of a Postoperative Pain in Laparoscopy-Assisted Distal Gastrectomy and Totally Laparoscopic Distal Gastrectomy according to the Location of the Mini-Laparotomy Site
- Corrigendum: Comparison of Short-Term Postoperative Outcomes in Totally Laparoscopic Distal Gastrectomy Versus Laparoscopy-Assisted Distal Gastrectomy
- Intracorporeal Anastomosis in Laparoscopic Gastric Cancer Surgery