Imaging Sci Dent.
2018 Jun;48(2):97-101. 10.5624/isd.2018.48.2.97.
Radiopacity of contemporary luting cements using conventional and digital radiography
- Affiliations
-
- 1Department of Oral and Maxillofacial Radiology, School of Dentistry, Kyungpook National University, Daegu, Korea.
- 2Department of Oral and Maxillofacial Radiology, School of Dentistry, Seoul National University, Seoul, Korea. raychoi@snu.ac.kr
- KMID: 2413920
- DOI: http://doi.org/10.5624/isd.2018.48.2.97
Abstract
- PURPOSE
This study evaluated the radiopacity of contemporary luting cements using conventional and digital radiography.
MATERIALS AND METHODS
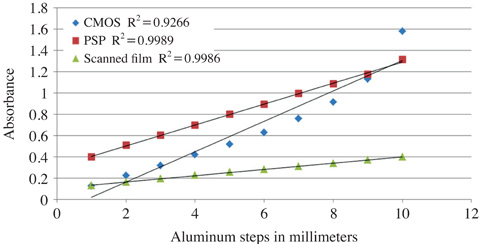
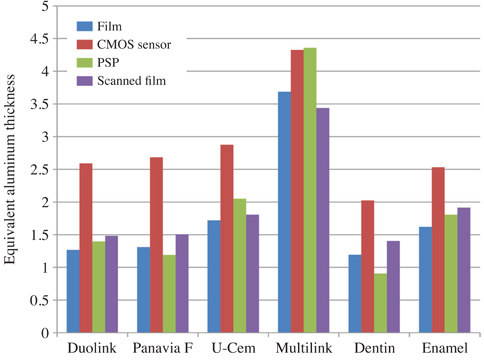
Disc specimens (N=24, n=6 per group, ø7 mm×1 mm) were prepared using 4 resin-based luting cements (Duolink, Multilink N, Panavia F 2.0, and U-cem). The specimens were radiographed using films, a complementary metal oxide semiconductor (CMOS) sensor, and a photostimulable phosphor plate (PSP) with a 10-step aluminum step wedge (1 mm incremental steps) and a 1-mm-thick tooth cut. The settings were 70 kVp, 4 mA, and 30 cm, with an exposure time of 0.2 s for the films and 0.1 s for the CMOS sensor and PSP. The films were scanned using a scanner. The radiopacity of the luting cements and tooth was measured using a densitometer for the film and NIH ImageJ software for the images obtained from the CMOS sensor, PSP, and scanned films. The data were analyzed using the Kruskal-Wallis and Mann-Whitney U tests.
RESULTS
Multilink (3.44-4.33) showed the highest radiopacity, followed by U-cem (1.81-2.88), Panavia F 2.0 (1.51-2.69), and Duolink (1.48-2.59). The R² values of the optical density of the aluminum step wedge were 0.9923 for the films, 0.9989 for the PSP, 0.9986 for the scanned films, and 0.9266 for the CMOS sensor in the linear regression models.
CONCLUSION
The radiopacities of the luting materials were greater than those of aluminum or dentin at the same thickness. PSP is recommended as a detector for radiopacity measurements because of its accuracy and convenience.
Keyword
MeSH Terms
Figure
Reference
-
1. Tsuge T. Radiopacity of conventional, resin-modified glass ionomer, and resin-based luting materials. J Oral Sci. 2009; 51:223–230.
Article2. American National Standards Institute/American Dental Association. ANSI/ADA: Specification no. 57 endodontic sealing material. Chicago: ADA;2000.3. Fraga RC, Luca-Fraga LR, Pimenta LA. Physical properties of resinous cements: an in vitro study. J Oral Rehabil. 2000; 27:1064–1067.
Article4. International Standard Organization. ISO 4049:2009. Dentistry - polymer-based restorative materials. 4th ed. Geneva: International Organization for Standardization;2009.5. Attar N, Tam LE, McComb D. Mechanical and physical properties of contemporary dental luting agents. J Prosthet Dent. 2003; 89:127–134.
Article6. Soares CJ, Santana FR, Fonseca RB, Martins LR, Neto FH. In vitro analysis of the radiodensity of indirect composites and ceramic inlay systems and its influence on the detection of cement overhangs. Clin Oral Investig. 2007; 11:331–336.
Article7. Wilson TG Jr. The positive relationship between excess cement and peri-implant disease: a prospective clinical endoscopic study. J Periodontol. 2009; 80:1388–1392.8. Dukic W, Delija B, Derossi D, Dadic I. Radiopacity of composite dental materials using a digital X-ray system. Dent Mater J. 2012; 31:47–53.
Article9. Altintas SH, Yildirim T, Kayipmaz S, Usumez A. Evaluation of the radiopacity of luting cements by digital radiography. J Prosthodont. 2013; 22:282–286.
Article10. Nomoto R, Mishima A, Kobayashi K, McCabe JF, Darvell BW, Watts DC, et al. Quantitative determination of radioopacity: equivalence of digital and film X-ray systems. Dent Mater. 2008; 24:141–147.
Article11. Poorsattar Bejeh Mir A, Poorsattar Bejeh Mir M. Assessment of radiopacity of restorative composite resins with various target distances and exposure times and a modified aluminum step wedge. Imaging Sci Dent. 2012; 42:163–167.
Article12. Amirouche-Korichi A, Mouzali M, Watts DC. Effects of monomer ratios and highly radiopaque fillers on degree of conversion and shrinkage-strain of dental resin composites. Dent Mater. 2009; 25:1411–1418.
Article13. Akerboom HB, Kreulen CM, van Amerongen WE, Mol A. Radiopacity of posterior composite resins, composite resin luting cements, and glass ionomer lining cements. J Prosthet Dent. 1993; 70:351–355.
Article14. Kurşun Ş, Dinç G, Oztaş B, Yüksel S, Kamburoğlu K. The visibility of secondary caries under bonding agents with two different imaging modalities. Dent Mater J. 2012; 31:975–979.15. Watts DC, McCabe JF. Aluminium radiopacity standards for dentistry: an international survey. J Dent. 1999; 27:73–78.
Article16. Duarte MA, Demarchi AC, Yamashita JC, Kuga MC, Fraga Sde C. pH and calcium ion release of 2 root-end filling materials. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003; 95:345–347.
Article17. Camilleri J, Montesin FE, Di Silvio L, Pitt Ford TR. The chemical constitution and biocompatibility of accelerated Portland cement for endodontic use. Int Endod J. 2005; 38:834–842.
Article18. Tanomaru-Filho M, da Silva GF, Duarte MA, Goncalves M, Tanomaru JM. Radiopacity evaluation of root-end filling materials by digitization of images. J Appl Oral Sci. 2008; 16:376–379.
Article19. An SY, Lee DH, Lee KB. Radiopacity for contemporary luting cements using digital radiography under various exposure conditions. J Prosthodont. 2015; 24:642–646.
Article20. Lachowski KM, Botta SB, Lascala CA, Matos AB, Sobral MA. Study of the radio-opacity of base and liner dental materials using a digital radiography system. Dentomaxillofac Radiol. 2013; 42:20120153.
Article21. Kapila R, Matsuda Y, Araki K, Okano T, Nishikawa K, Sano T. Radiopacity measurement of restorative resins using film and three digital systems for comparison with ISO 4049: International standard. Bull Tokyo Dent Coll. 2015; 56:207–214.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparative study of the radiopacity of resin cements used in aesthetic dentistry
- Evaluation of the radiopacity of restorative materials with different structures and thicknesses using a digital radiography system
- Effect of adhesive luting on the fracture resistance of zirconia compared to that of composite resin and lithium disilicate glass ceramic
- Comparative evaluation of micro-shear bond strength between two different luting methods of resin cement to dentin
- MARGINAL FITNESS AND MARGINAL LEAKAGE OF FIBER-REINFORCED COMPOSITE CROWNS DEPENDING UPON LUTING CEMENTS