J Educ Eval Health Prof.
2016;13:44. 10.3352/jeehp.2016.13.44.
A cost-effectiveness analysis of self-debriefing versus instructor debriefing for simulated crises in perioperative medicine in Canada
- Affiliations
-
- 1Centre for Excellence in Economic Analysis Research, The HUB Health Research Solutions, Li Ka Shing Knowledge Institute, St. Michael's Hospital, Ontario, Canada.
- 2Institute for Health Policy, Management and Evaluation, University of Toronto, Ontario, Canada.
- 3Department of Anesthesia, Sunnybrook Health Sciences Centre, Ontario, Canada.
- 4The Wilson Centre for Research in Medical Education, University of Toronto, Ontario, Canada.
- 5Department of Anesthesiology, The Ottawa Hospital Research Institute, The Ottawa Hospital, Ontario, Canada. sboet@toh.ca
- 6Department of Innovation in Medical Innovation, University of Ottawa, Ontario, Canada.
- KMID: 2413793
- DOI: http://doi.org/10.3352/jeehp.2016.13.44
Abstract
- PURPOSE
High-fidelity simulation training is effective for learning crisis resource management (CRM) skills, but cost is a major barrier to implementing high-fidelity simulation training into the curriculum. The aim of this study was to examine the cost-effectiveness of self-debriefing and traditional instructor debriefing in CRM training programs and to calculate the minimum willingness-to-pay (WTP) value when one debriefing type becomes more cost-effective than the other.
METHODS
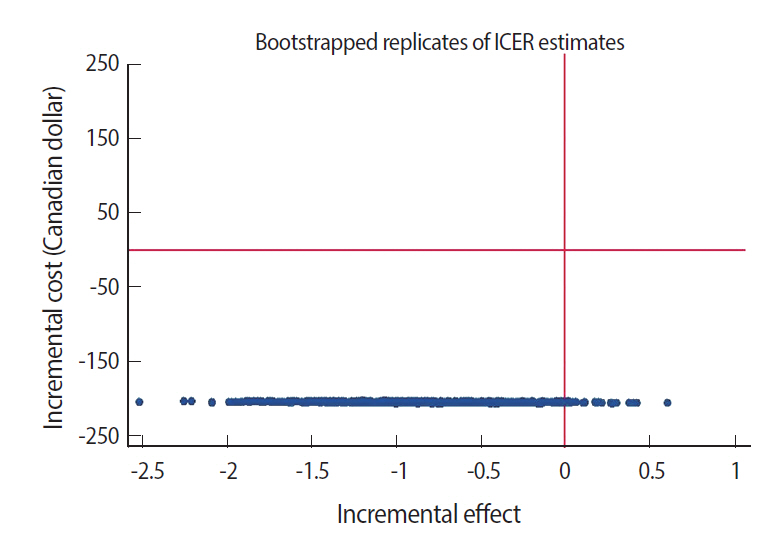
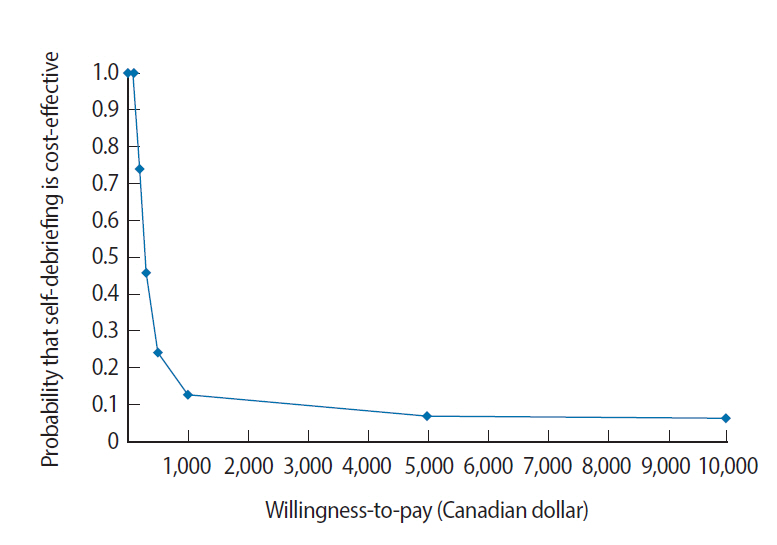
This study used previous data from a randomized controlled trial involving 50 anesthesiology residents in Canada. Each participant managed a pretest crisis scenario. Participants who were randomized to self-debrief used the video of their pretest scenario with no instructor present during their debriefing. Participants from the control group were debriefed by a trained instructor using the video of their pretest scenario. Participants individually managed a post-test simulated crisis scenario. We compared the cost and effectiveness of self-debriefing versus instructor debriefing using net benefit regression. The cost-effectiveness estimate was reported as the incremental net benefit and the uncertainty was presented using a cost-effectiveness acceptability curve.
RESULTS
Self-debriefing costs less than instructor debriefing. As the WTP increased, the probability that self-debriefing would be cost-effective decreased. With a WTP ≤Can$200, the self-debriefing program was cost-effective. However, when effectiveness was priced higher than cost-savings and with a WTP >Can$300, instructor debriefing was the preferred alternative.
CONCLUSION
With a lower WTP (≤Can$200), self-debriefing was cost-effective in CRM simulation training when compared to instructor debriefing. This study provides evidence regarding cost-effectiveness that will inform decision-makers and clinical educators in their decision-making process, and may help to optimize resource allocation in education.
MeSH Terms
Figure
Cited by 1 articles
-
What is interesting in the issue 2016 of
Journal of Educational Evaluation for Health Professions?
Yera Hur
J Educ Eval Health Prof. 2016;13:46. doi: 10.3352/jeehp.2016.13.46.
Reference
-
References
1. Savoldelli GL, Naik VN, Park J, Joo HS, Chow R, Hamstra SJ. Value of debriefing during simulated crisis management: oral versus video-assisted oral feedback. Anesthesiology. 2006; 105:279–285. https://doi.org/10.1097/00000542-200608000-00010.
Article2. Boet S, Bould MD, Bruppacher HR, Desjardins F, Chandra DB, Naik VN. Looking in the mirror: self-debriefing versus instructor debriefing for simulated crises. Crit Care Med. 2011; 39:1377–1381. https://doi.org/10.1097/CCM.0b013e31820eb8be.
Article3. Boet S, Bould MD, Sharma B, Revees S, Naik VN, Triby E, Grantcharov T. Within-team debriefing versus instructor-led debriefing for simulation-based education: a randomized controlled trial. Ann Surg. 2013; 258:53–58. https://doi.org/10.1097/SLA.0b013e31829659e4.
Article4. Khanduja PK, Bould MD, Naik VN, Hladkowicz E, Boet S. The role of simulation in continuing medical education for acute care physicians: a systematic review. Crit Care Med. 2015; 43:186–193. https://doi.org/10.1097/CCM.0000000000000672.
Article5. Boet S, Bould MD, Fung L, Qosa H, Perrier L, Tavares W, Reeves S, Tricco AC. Transfer of learning and patient outcome in simulated crisis resource management: a systematic review. Can J Anaesth. 2014; 61:571–582. https://doi.org/10.1007/s12630-014-0143-8.
Article6. Levatt-Jones T, Lapkin S. A systematic review of the effectiveness of simulation debriefing in health professional education. Nurse Educ Today. 2014; 34:e58–63. https://doi.org/10.1016/j.nedt.2013.09.020.
Article7. Cheng A, Eppich W, Grant V, Sherbino J, Zendejas B, Cook DA. Debriefing for technology-enhanced simulation: a systematic review and meta-analysis. Med Educ. 2014; 48:657–666. https://doi.org/10.1111/medu.12432.
Article8. Zendejas B, Wang AT, Brydges R, Hamstra SJ, Cook DA. Cost: the missing outcome in simulation-based medical education research: a systematic review. Surgery. 2013; 153:160–176. https://doi.org/10.1016/j.surg.2012.06.025.
Article9. LeBlanc V, Bould M, McNaughton N, Brydges R, Piquette D, Sharma B. Simulation in postgraduate medical education [Internet]. Ottawa (ON): Members of the FMEC PG consortium;2011. [cited 2016 Oct 26 ]. Available from: https://www.afmc.ca/pdf/fmec/18_LeBlanc_Simulation%20and%20Technology.pdf.10. Cohen ER, Feinglass J, Barsuk JH, Barnard C, O’Donnell A, McGaghie WC, Wayne DB. Cost savings from reduced catheter-related bloodstream infection after simulation-based education for residents in a medical intensive care unit. Simul Healthc. 2010; 5:98–102. https://doi.org/10.1097/SIH.0b013e3181bc8304.
Article11. Barsuk JH, Cohen ER, Feinglass J, Kozmic SE, McGaghie WC, Ganger D, Wayne DB. Cost savings of performing paracentesis procedures at the bedside after simulation-based education. Simul Healthc. 2014; 9:312–318. https://doi.org/10.1097/SIH.0000000000000040.
Article12. Welke TM, LeBlanc VR, Savoldelli GL, Joo HS, Chandra DB, Crabtree NA, Naik VN. Personalized oral debriefing versus standardized multimedia instruction after patient crisis simulation. Anesth Analg. 2009; 109:183–189. https://doi.org/10.1213/ane.0b013e3181a324ab.
Article13. Isaranuwatchai W, Brydges R, Carnahan H, Backstein D, Dubrowski A. Comparing the cost-effectiveness of simulation modalities: a case study of peripheral intravenous catheterization training. Adv Health Sci Educ Theory Pract. 2014; 19:219–232. https://doi.org/10.1007/s10459-013-9464-6.
Article14. Fletcher G, Flin R, McGeorge P, Glavin R, Maran N, Patey R. Anaesthetists’ Non-Technical Skills (ANTS): evaluation of a behavioural marker system. Br J Anaesth. 2003; 90:580–588. https://doi.org/10.1093/bja/aeg112.
Article15. University of Ottawa Skills and Simulation Centre. Fee structure [Internet]. Ottawa (ON): The Ottawa Hospital;[cited 2016 Oct 26 ]. Available from: http://uossc.ca/book-your-event/fee-structure/.16. Medical Career Services. Canadian medical residency guide: taking control of your future medical career and financial life [Internet]. [Montreal]: RBC Royal Bank and Medical Career Services;c2012. [cited 2016 Oct 26 ]. Available from: https://www.schulich.uwo.ca/learner-equity-wellness/services/Canadian_Medical_Residency_Guide.pdf.17. Hoch JS, Briggs AH, Willan AR. Something old, something new, something borrowed, something blue: a framework for the marriage of health econometrics and cost-effectiveness analysis. Health Econ. 2002; 11:415–430. https://doi.org/10.1002/hec.678.
Article18. Drummond M, Sculpher MJ, Claxton K, Stoddart G, Torrance GW. Textbook of methods for the economic evaluation of health care programmes. 4th ed. New York (NY): Oxford University Press;2015.19. Hoch JS, Rockx MA, Krahn AD. Using the net benefit regression framework to construct cost-effectiveness acceptability curves: an example using data from a trial of external loop recorders versus Holter monitoring for ambulatory monitoring of “community acquired” syncope. BMC Health Serv Res. 2006; 6:68. https://doi.org/10.1186/1472-6963-6-68.
Article20. Riem N, Boet S, Bould MD, Tavares W, Naik VN. Do technical skills correlate with non-technical skills in crisis resource management: a simulation study. Br J Anaesth. 2012; 109:723–728. https://doi.org/10.1093/bja/aes256.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Learning with our peers: peer-led versus instructor-led debriefing for simulated crises, a randomized controlled trial
- Standardized learner simulation for debriefer training through video conference
- Comparative analysis of nursing students’ reflection levels before and after debriefing in simulation training in South Korea: qualitative analysis design
- Debriefing in pediatrics
- Nursing Students' Perceptions of Meaning, Response, and Effective Methods for Debriefing in Simulation-based Education