J Adv Prosthodont.
2018 Jun;10(3):227-235. 10.4047/jap.2018.10.3.227.
The effect of undersizing and tapping on bone to implant contact and implant primary stability: A histomorphometric study on bovine ribs
- Affiliations
-
- 1Dental School, Vita-Salute University IRCCS San Raffaele, Milan, Italy.
- 2Department of Medical, Oral and Biotechnological Sciences, Chieti-Pescara University “G. D'Annunzioâ€, Chieti, Italy. v.perrotti@unich.it
- 3Private Practitioner, Trezzano Sul Naviglio, Milano, Italy.
- 4Private Practitioner, Vimercate, Monza-Brianza, Italy.
- KMID: 2413492
- DOI: http://doi.org/10.4047/jap.2018.10.3.227
Abstract
- PURPOSE
Implant site preparation may be adjusted to achieve the maximum possible primary stability. The aim of this investigation was to study the relation among bone-to-implant contact at insertion, bone density, and implant primary stability intra-operatively measured by a torque-measuring implant motor, when implant sites were undersized or tapped.
MATERIALS AND METHODS
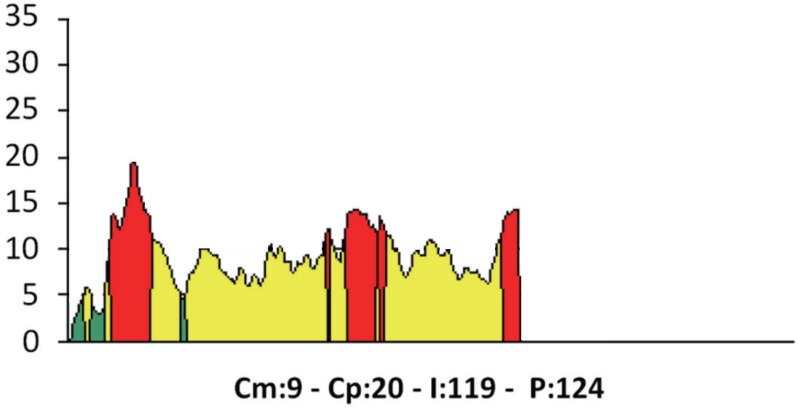
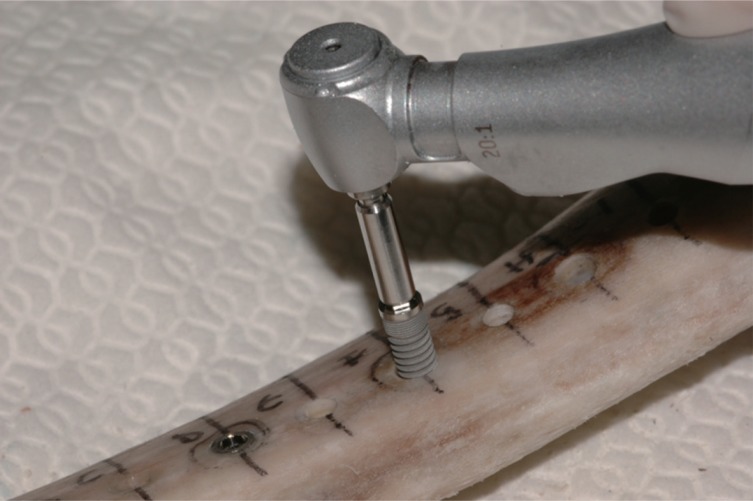
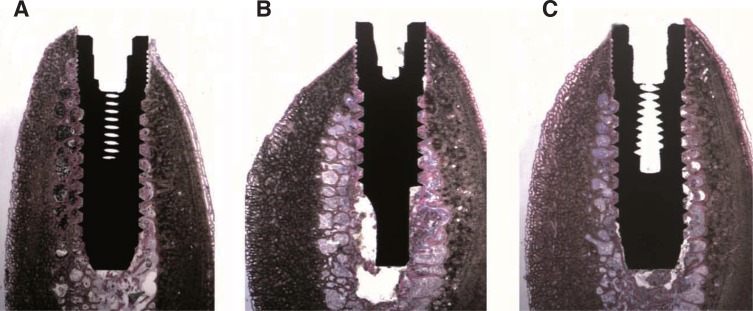
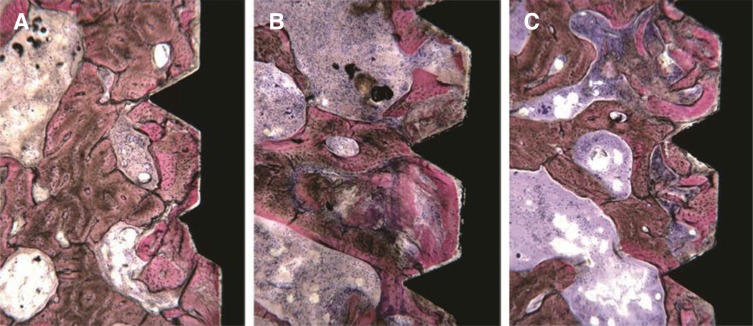
Undersized (n=14), standard (n=13), and tapped (n=13) implant sites were prepared on 9 segments of bovine ribs. After measuring bone density using the implant motor, 40 implants were placed, and their primary stability assessed by measuring the integral of the torque-depth insertion curve. Bovine ribs were then processed histologically, the bone-to-implant contact measured and statistically correlated to bone density and the integral.
RESULTS
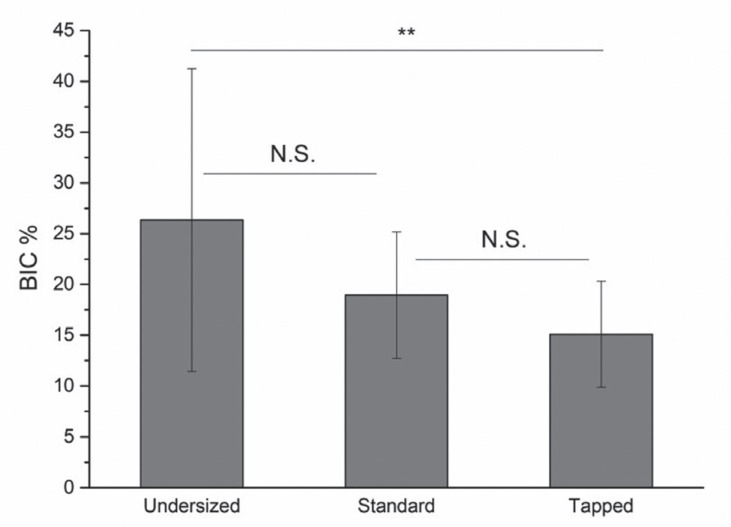
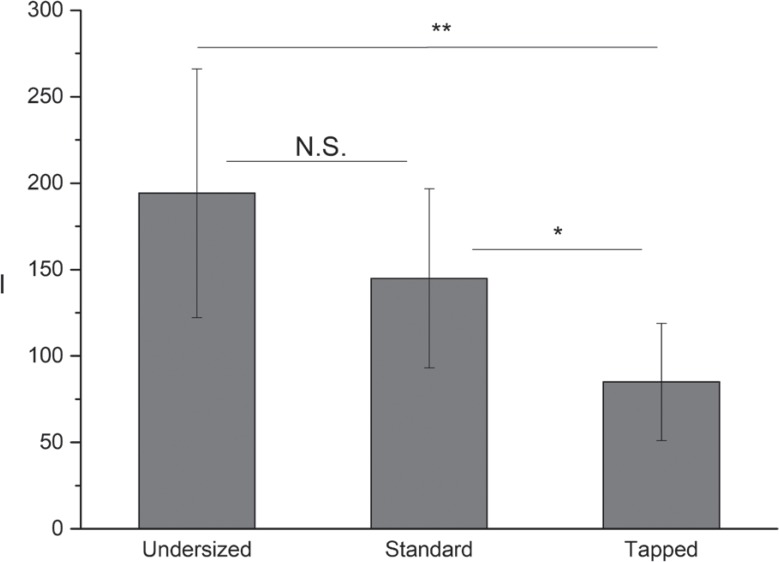
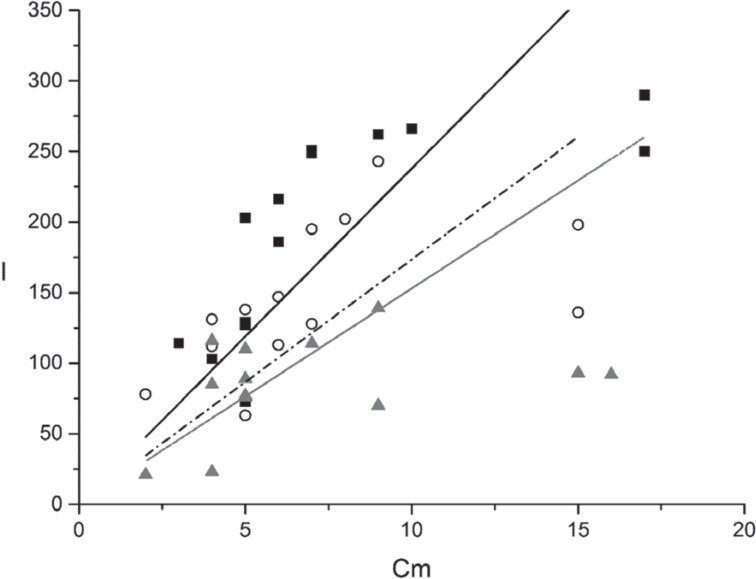
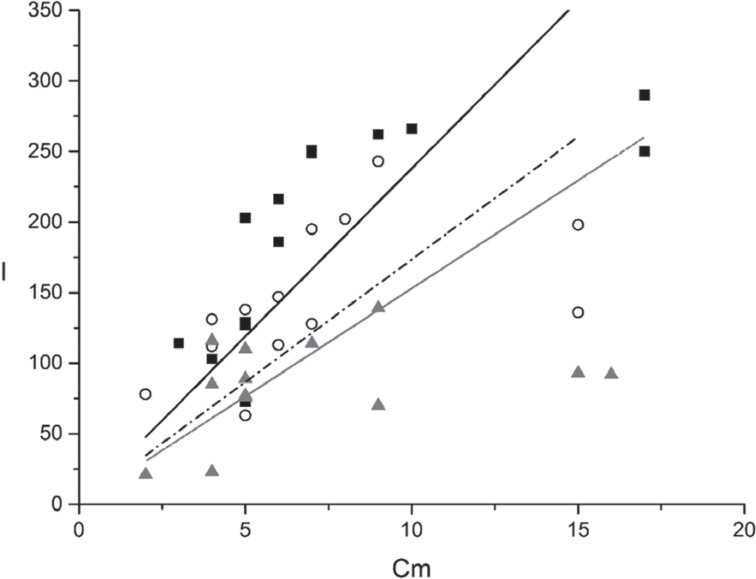
Bone-to-implant contact and the integral of the torque-depth curve were significantly greater for undersized sites than tapped sites. Moreover, a correlation between bone to implant contact, the integral and bone density was found under all preparation conditions. The slope of the bone-to-implant/density and integral/density lines was significantly greater for undersized sites, while those corresponding to standard prepared and tapped sites did not differ significantly.
CONCLUSION
The integral of the torque-depth curve provided reliable information about bone-to-implant contact and primary implant stability even in tapped or undersized sites. The linear relations found among the parameters suggests a connection between extent and modality of undersizing and the corresponding increase of the integral and, consequently, of primary stability. These results might help the physician determine the extent of undersizing needed to achieve the proper implant primary stability, according to the planned loading protocol.
Keyword
MeSH Terms
Figure
Reference
-
1. Glauser R, Sennerby L, Meredith N, Rée A, Lundgren A, Gottlow J, Hämmerle CH. Resonance frequency analysis of implants subjected to immediate or early functional occlusal loading. Successful vs. failing implants. Clin Oral Implants Res. 2004; 15:428–434. PMID: 15248877.
Article2. Möhlhenrich SC, Kniha K, Heussen N, Hölzle F, Modabber A. Effects on primary stability of three different techniques for implant site preparation in synthetic bone models of different densities. Br J Oral Maxillofac Surg. 2016; 54:980–986. PMID: 27461557.
Article3. Friberg B, Ekestubbe A, Mellström D, Sennerby L. Brånemark implants and osteoporosis: a clinical exploratory study. Clin Implant Dent Relat Res. 2001; 3:50–56. PMID: 11441543.
Article4. Stocchero M, Toia M, Cecchinato D, Becktor JP, Coelho PG, Jimbo R. Biomechanical, biologic, and clinical outcomes of undersized implant surgical preparation: A systematic review. Int J Oral Maxillofac Implants. 2016; 31:1247–1263. PMID: 27861649.
Article5. Tabassum A, Walboomers XF, Wolke JG, Meijer GJ, Jansen JA. Bone particles and the undersized surgical technique. J Dent Res. 2010; 89:581–586. PMID: 20212102.
Article6. Shalabi MM, Wolke JG, de Ruijter AJ, Jansen JA. Histological evaluation of oral implants inserted with different surgical techniques into the trabecular bone of goats. Clin Oral Implants Res. 2007; 18:489–495. PMID: 17517059.
Article7. Tabassum A, Meijer GJ, Wolke JG, Jansen JA. Influence of the surgical technique and surface roughness on the primary stability of an implant in artificial bone with a density equivalent to maxillary bone: a laboratory study. Clin Oral Implants Res. 2009; 20:327–332. PMID: 19298286.
Article8. Al-Marshood MM, Junker R, Al-Rasheed A, Al Farraj Aldosari A, Jansen JA, Anil S. Study of the osseointegration of dental implants placed with an adapted surgical technique. Clin Oral Implants Res. 2011; 22:753–759. PMID: 21198894.
Article9. Alghamdi H, Anand PS, Anil S. Undersized implant site preparation to enhance primary implant stability in poor bone density: a prospective clinical study. J Oral Maxillofac Surg. 2011; 69:e506–e512. PMID: 22117707.
Article10. Di Stefano DA, Arosio P, Piattelli A, Perrotti V, Iezzi G. A torque-measuring micromotor provides operator independent measurements marking four different density areas in maxillae. J Adv Prosthodont. 2015; 7:51–55. PMID: 25722838.
Article11. Iezzi G, Scarano A, Di Stefano DA, Arosio P, Doi K, Ricci L, Piattelli A, Perrotti V. Correlation between the bone density recorded by a computerized implant motor and by a histomorphometric analysis: a preliminary in vitro study on bovine ribs. Clin Implant Dent Relat Res. 2015; 17:e35–e44. PMID: 23879771.
Article12. Di Stefano DA, Arosio P. Correlation between bone density and instantaneous torque at implant site preparation: A validation on polyurethane foam blocks of a device assessing density of jawbones. Int J Oral Maxillofac Implants. 2016; 31:e128–e135. PMID: 27632279.
Article13. Degidi M, Daprile G, Piattelli A, Iezzi G. Development of a new implant primary stability parameter: insertion torque revisited. Clin Implant Dent Relat Res. 2013; 15:637–644. PMID: 22008885.
Article14. Iezzi G, Filippone A, Di Stefano DA, Arosio P, Piattelli A, Scarano A, Perrotti V. A site-specific intraoperative measurement of bone-to-implant contact during implant insertion: A study on bovine ribs using a computerized implant motor. J Dent Sci. 2015; 10:21–27.
Article15. Capparé P, Vinci R, Di Stefano DA, Traini T, Pantaleo G, Gherlone EF, Gastaldi G. Correlation between initial BIC and the insertion torque/depth integral recorded with an instantaneous torque-measuring implant motor: An in vivo study. Clin Implant Dent Relat Res. 2015; 17:e613–e620. PMID: 25876078.
Article16. Di Stefano DA, Arosio P, Gastaldi G, Gherlone E. The insertion torque-depth curve integral as a measure of implant primary stability: An in vitro study on polyurethane foam blocks. J Prosthet Dent. 2017; 7. 08.17. Wang TM, Lee MS, Wang JS, Lin LD. The effect of implant design and bone quality on insertion torque, resonance frequency analysis, and insertion energy during implant placement in low or low- to medium-density bone. Int J Prosthodont. 2015; 28:40–47. PMID: 25588172.
Article18. Degidi M, Daprile G, Piattelli A. Influence of underpreparation on primary stability of implants inserted in poor quality bone sites: an in vitro study. J Oral Maxillofac Surg. 2015; 73:1084–1088. PMID: 25861691.19. Piattelli A, Scarano A, Quaranta M. High-precision, cost-effective cutting system for producing thin sections of oral tissues containing dental implants. Biomaterials. 1997; 18:577–579. PMID: 9105598.
Article20. Andrade JM, Estévez-Pérez MG. Statistical comparison of the slopes of two regression lines: A tutorial. Anal Chim Acta. 2014; 838:1–12. PMID: 25064237.
Article21. Ku HH. Notes on the use of propagation of error formulas. J Res Natl Bur Stand. 1966; 70C:263–273.
Article22. Fernandes Ede L, Unikowski IL, Teixeira ER, da Costa NP, Shinkai RS. Primary stability of turned and acid-etched screw-type implants: a removal torque and histomorphometric study in rabbits. Int J Oral Maxillofac Implants. 2007; 22:886–892. PMID: 18271369.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effect of bone quality and implant surgical technique on implant stability quotient (ISQ) value
- The effect of osteotome technique on primary implant stability according to implant fixture diameter
- The effect of implant shape and bone preparation on primary stability
- Influence of implant fixture design on implant primary stability
- A study on the finite element analysis and bone formation of the apically expandable implant