Blood Res.
2017 Jun;52(2):135-136. 10.5045/br.2017.52.2.135.
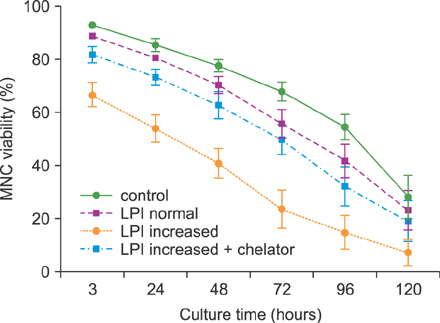
Impact of labile plasma iron and iron chelation on the viability of cultured mononuclear cells from patients undergoing autologous hematopoietic stem cell transplantation
- Affiliations
-
- 1Academia de Ciência e Tecnologia, São José do Rio Preto, Brazil.
- 2Instituto de Quimica, Universidade de São Paulo, São Paulo, Brazil.
- 3Cardiovascular Diseases Institute (IMC), São Jose do Rio Preto, Brazil. drflavio@institutonaoum.com.br
- KMID: 2413332
- DOI: http://doi.org/10.5045/br.2017.52.2.135
Abstract
- No abstract available.
Figure
Reference
-
1. Majhail NS, Lazarus HM, Burns LJ. Iron overload in hematopoietic cell transplantation. Bone Marrow Transplant. 2008; 41:997–1003.
Article2. Evens AM, Mehta J, Gordon LI. Rust and corrosion in hematopoietic stem cell transplantation: the problem of iron and oxidative stress. Bone Marrow Transplant. 2004; 34:561–571.
Article3. Parkkinen J, Sahlstedt L, von Bonsdorff L, Salo H, Ebeling F, Ruutu T. Effect of repeated apotransferrin administrations on serum iron parameters in patients undergoing myeloablative conditioning and allogeneic stem cell transplantation. Br J Haematol. 2006; 135:228–234.
Article4. Pullarkat V. Iron overload in patients undergoing hematopoietic stem cell transplantation. Adv Hematol. 2010; 2010:345756.
Article5. Bradley SJ, Gosriwitana I, Srichairatanakool S, Hider RC, Porter JB. Non-transferrin-bound iron induced by myeloablative chemotherapy. Br J Haematol. 1997; 99:337–343.
Article6. Naoum FA, Espósito BP, Ruiz LP, et al. Assessment of labile plasma iron in patients who undergo hematopoietic stem cell transplantation. Acta Haematol. 2014; 131:222–226.
Article7. Dürken M, Agbenu J, Finckh B, et al. Deteriorating free radical-trapping capacity and antioxidant status in plasma during bone marrow transplantation. Bone Marrow Transplant. 1995; 15:757–762.8. Zhao M, Xie F, Li Y, et al. Increased intracellular concentration of reactive oxygen species mediated the deficient hematopoiesis of iron overload bone marrow. Blood (ASH Annual Meeting Abstracts). 2010; 116:Suppl. abst 4247.
Article9. Juvonen E, Sahlstedt L, Parkkinen J, Ruutu T. Inhibition of erythroid and granulocyte-macrophage colony formation by non-transferrin-bound iron in vitro: protective effect of apotransferrin. Eur J Haematol. 2007; 79:126–131.
Article10. Hartmann J, Sinzig U, Wulf G, et al. Evidence for a suppression of the colony forming capacity of erythroid progenitors by iron overload in patients with MDS. Blood (ASH Annual Meeting Abstracts). 2008; 112:Suppl. abst 2694.
Article11. Jensen PD, Heickendorff L, Pedersen B, et al. The effect of iron chelation on haemopoiesis in MDS patients with transfusional iron overload. Br J Haematol. 1996; 94:288–299.
Article12. Glickstein H, Nick H, Cabantchik ZI. Susceptibility of endocrine, cardiac, and macrophage cell lines to iron-mediated oxidative damage and the cytoprotective effect of the orally active chelator deferasirox (Exjade®, ICL670). Blood (ASH Annual Meeting Abstracts). 2007; 110:Suppl. abst 3825.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Six Cases of Iron Containing Plasma Cells
- Acute Tubulointerstitial Nephritis Induced by Deferasirox following Hematopoietic Stem Cell Transplantation for Severe Aplastic Anemia
- Comparison of Quality of Life of Autologous and Allogeneic Hematopoietic Stem Cell Transplantation Recipients
- Role of redox iron towards an increase in mortality among patients: a systemic review and meta-analysis
- Influence of Serum Ferritin on Transplant-related Outcomes and Complications in Children Undergoing Allogeneic Hematopoietic Stem Cell Transplantation