J Rhinol.
2018 May;25(1):55-58. 10.18787/jr.2018.25.1.55.
Saddle Nose Deformity as a Result of an Aseptic Nasal Abscess Accompanied by Ulcerative Colitis and Pyoderma Gangrenosum
- Affiliations
-
- 1Department of Otolaryngology-Head and Neck Surgery, Inje University Seoul Paik Hospital, Seoul, Korea. jsc4g@paik.ac.kr
- KMID: 2412923
- DOI: http://doi.org/10.18787/jr.2018.25.1.55
Abstract
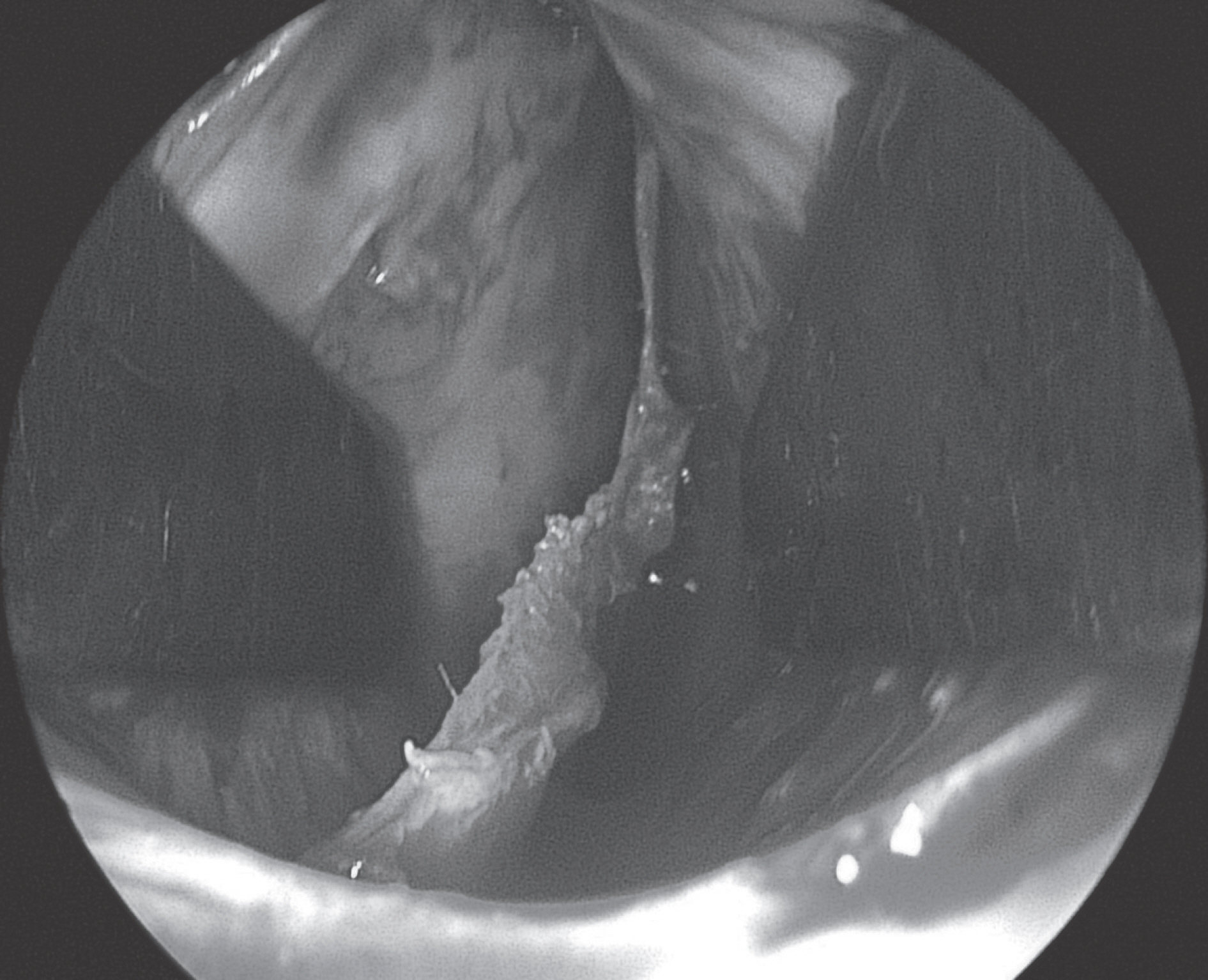
- Ulcerative colitis (UC) is a chronic inflammatory bowel disease (IBD) that causes granulomatous inflammation in the mucous membrane of the intestinal tract, especially in the colon. Additionally, UC can be accompanied by extraintestinal manifestation (EIM). EIM of UC includes cutaneous lesions such as pyoderma gangrenosum, and rarely, systemically occurring aseptic abscesses (AA) have been reported in a few cases. Nasal involvement of UC as an extraintestinal manifestation of IBD is rare, and few reports of nasal mucosa and septal cartilage involvement have been documented in the literature. However, aseptic nasal abscess involving septal cartilage associated with UC and pyoderma gangrenosum resulting in saddle nose deformity have not been reported. The author presents a case of a 52 year-old woman with UC and pyoderma gangrenosum and an aseptic abscess in the nasal septal cartilage resulting in saddle nose deformity, which was corrected by augmentation rhinoplasty.
MeSH Terms
Figure
Reference
-
1). Vavricka SR., Schoepfer A., Scharl M., Lakatos PL., Navarini A., Ro-gler G. Extraintestinal Manifestations of Inflammatory Bowel Disease. Inflamm Bowel Dis. 2015. 21(8):1982–92.
Article2). Zois CD., Katsanos KH., Tsianos EV. Ear-nose-throat manifestations in Inflammatory Bowel Diseases. Ann gastroenterol. 2007. 20(4):265–74.3). Powell FC., Schroeter AL., Su WP., Perry HO. Pyoderma gangrenosum: a review of 86 patient. Q J Med. 1985. 55(217):173–86.4). Krikovich MD., Kelly SM., Jackson WD. Nasal septal perforation: rare extraintestinal manifestation of Crohn's diasese. Ear Nose Throat. 2000. 79:520–3.5). Merkonidis C., Verma S., Salam MA. Saddle nose deformity in a patient with Crohn's disease. J Laryngol Otol. 2005. 119:573–6.
Article6). Andre MF., Piette JC., Kemery JL., Ninet J., Jego P., Delevaux I, et al. Aseptic abscesses: a study of 30 patients with or without inflammatory bowel disease and review of the literature. Medicine. 2007. 86:145–61.7). Bollegala N., Khan N., Scaffidi MA., Al-Mazroui A., Tessolini J., Showler A, et al. Aseptic Abscess and inflammatory bowel disease: Two cases and Review of Literature. Can J Gastroenterol Hepatol. 2017. 2017:5124354.8). Yılmaz B., Yusel O., Coban S¸ Cakmak I., Basar O., Ekiz F. Rare Complication of Ulcerative Colitis: Aseptic Nasal Septal Abscess. In-flamm Bowel Dis. 2011. 17(7):E71.9). Goral V. Rare and New Extraintestinal Complication of Ulcerative Colitis: Nasal Septal Perforation. Inflamm Bowel Dis. 2012. 18(2):E397–8.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Post-traumatic Pyoderma Gangrenosum Associated with Ulcerative Colitis
- A Case of Pyoderma Gangrenosum Associated with Ulcerative Colitis
- Multiple Pyoderma Gangrenosum in Ulcerative Colitis
- A Case of Simultaneous Presentation of Bullous and Ulcerative Types of Pyoderma Gangrenosum in an Ulcerative Colitis Patient
- Pyoderma Gangrenosum in a Patient with Ulcerative Colitis: A Case Report