Korean J Ophthalmol.
2018 Jun;32(3):204-210. 10.3341/kjo.2017.0050.
Incidence and Risk Factors of Cystoid Macular Edema after Vitrectomy with Silicone Oil Tamponade for Retinal Detachment
- Affiliations
-
- 1Siloam Eye Hospital, Seoul, Korea.
- 2Department of Ophthalmology, Institute of Vision Research, Severance Hospital, Yonsei University College of Medicine, Seoul, Korea. semekim@yuhs.ac
- 3Department of Ophthalmology, Yonsei University Wonju College of Medicine, Wonju, Korea.
- KMID: 2412799
- DOI: http://doi.org/10.3341/kjo.2017.0050
Abstract
- PURPOSE
To investigate the incidence and risk factors of cystoid macular edema (CME) after silicone oil (SO) injection for retinal detachment.
METHODS
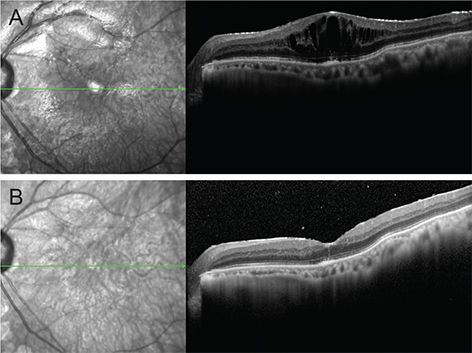
Fifty-eight patients with retinal detachment treated by vitrectomy with SO tamponade during 2011 to 2015 were retrospectively assigned to CME and non-CME groups. Patients underwent complete ophthalmological examination, including color fundus photography and preoperative and postoperative optical coherence tomography. Risk factors for CME during SO tamponade were determined by regression analyses.
RESULTS
Of the 58 eyes, 21 (36.2%) exhibited CME. The presence of posterior staphyloma in the CME group was significantly more frequent than in the non-CME group (p = 0.026). There were no significant differences in other demographic or clinical characteristics between the CME and non-CME groups. Significant correlations were observed between CME after vitrectomy with SO tamponade and the presence of posterior staphyloma (odds ratio, 4.03; p = 0.031). Of the 21 eyes with CME, 13 underwent SO removal, among which 11 experienced resolution of CME with or without further intervention.
CONCLUSIONS
The presence of posterior staphyloma is significantly associated with CME after vitrectomy with SO tamponade. Patients with retinal detachment exhibiting posterior staphyloma should be evaluated for potential CME during SO tamponade.
Keyword
MeSH Terms
Figure
Reference
-
1. Vitrectomy with silicone oil or sulfur hexafluoride gas in eyes with severe proliferative vitreoretinopathy: results of a randomized clinical trial. Silicone Study Report 1. Arch Ophthalmol. 1992; 110:770–779.2. Vitrectomy with silicone oil or perfluoropropane gas in eyes with severe proliferative vitreoretinopathy: results of a randomized clinical trial. Silicone Study Report 2. Arch Ophthalmol. 1992; 110:780–792.3. Laqua H, Lucke K, Foerster MH. Development and current status of silicone oil surgery. Klin Monbl Augenheilkd. 1988; 192:277–283.4. Riedel KG, Gabel VP, Neubauer L, et al. Intravitreal silicone oil injection: complications and treatment of 415 consecutive patients. Graefes Arch Clin Exp Ophthalmol. 1990; 228:19–23.
Article5. Casswell AG, Gregor ZJ. Silicone oil removal I The effect on the complications of silicone oil. Br J Ophthalmol. 1987; 71:893–897.
Article6. Casswell AG, Gregor ZJ. Silicone oil removal II Operative and postoperative complications. Br J Ophthalmol. 1987; 71:898–902.
Article7. Franks WA, Leaver PK. Removal of silicone oil: rewards and penalties. Eye (Lond). 1991; 5(Pt 3):333–337.8. Hutton WL, Azen SP, Blumenkranz MS, et al. The effects of silicone oil removal. Silicone Study Report 6. Arch Ophthalmol. 1994; 112:778–785.9. La Heij EC, Hendrikse F, Kessels AG. Results and complications of temporary silicone oil tamponade in patients with complicated retinal detachments. Retina. 2001; 21:107–114.
Article10. Colin J. The role of NSAIDs in the management of postoperative ophthalmic inflammation. Drugs. 2007; 67:1291–1308.
Article11. Rashad MA, Mohamed AA, Ahmed AI. Value of optical coherence tomography in the detection of macular pathology before the removal of silicone oil. Clin Ophthalmol. 2016; 10:121–135.
Article12. Bae SH, Hwang JS, Yu HG. Comparative analysis of macular microstructure by spectral-domain optical coherence tomography before and after silicone oil removal. Retina. 2012; 32:1874–1883.
Article13. Kiss CG, Richter-Muksch S, Sacu S, et al. Anatomy and function of the macula after surgery for retinal detachment complicated by proliferative vitreoretinopathy. Am J Ophthalmol. 2007; 144:872–877.
Article14. Karahan E, Tuncer I, Zengin MO, et al. Spontaneous resolution of macular edema after silicone oil removal. Int J Ophthalmol. 2014; 7:1005–1009.15. Lo DM, Flaxel CJ, Fawzi AA. Macular effects of silicone oil tamponade: optical coherence tomography findings during and after silicone oil removal. Curr Eye Res. 2017; 42:98–103.
Article16. Christensen UC, la Cour M. Visual loss after use of intraocular silicone oil associated with thinning of inner retinal layers. Acta Ophthalmol. 2012; 90:733–737.
Article17. Wolf S, Schon V, Meier P, Wiedemann P. Silicone oil-RMN3 mixture (“heavy silicone oil”) as internal tamponade for complicated retinal detachment. Retina. 2003; 23:335–342.
Article18. Asaria RH, Kon CH, Bunce C, et al. Silicone oil concentrates fibrogenic growth factors in the retro-oil fluid. Br J Ophthalmol. 2004; 88:1439–1442.
Article19. Funatsu H, Noma H, Mimura T, et al. Association of vitreous inflammatory factors with diabetic macular edema. Ophthalmology. 2009; 116:73–79.
Article20. Curtin BJ. The posterior staphyloma of pathologic myopia. Trans Am Ophthalmol Soc. 1977; 75:67–86.21. Wang NK, Wu YM, Wang JP, et al. Clinical characteristics of posterior staphylomas in myopic eyes with axial length shorter than 26.5 millimeters. Am J Ophthalmol. 2016; 162:180–190.22. Azzolini C, Donati S, Caprani SM, et al. Macular edema and silicone oil tamponade. J Clin Exp Ophthalmol. 2014; 5:366.
Article23. Scheerlinck LM, Schellekens PA, Liem AT, et al. Incidence, risk factors, and clinical characteristics of unexplained visual loss after intraocular silicone oil for macula-on retinal detachment. Retina. 2016; 36:342–350.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Primary Silicone Oil Tamponade with Vitrectomy in Macular Hole Retinal Detachment of Highly Myopic Eyes
- Silicone Oil with Short-Term Prone Position in Macular Hole Retinal Detachment Surgery in High Myopia
- Vitrectomy and Silicone Oil Tamponade to Prevent Retinal Detachment in Severe Acute Retinal Necrosis Syndrome
- A Clinical Study on the Silicone Oil in the Treatment of Proliferative Diabetic Retinopathy
- Case of Atrophied Retina after Retinal Detachment Reoperation