Allergy Asthma Respir Dis.
2018 May;6(3):174-178. 10.4168/aard.2018.6.3.174.
Clinical features of eczema herpeticum in atopic dermatitis in a single center
- Affiliations
-
- 1Department of Pediatrics, Pusan National University Hospital, Pusan National University School of Medicine, Busan, Korea. pearlhy@naver.com
- 2Department of Pediatrics, Pusan National University Children's Hospital, Pusan National University School of Medicine, Yangsan, Korea.
- KMID: 2412521
- DOI: http://doi.org/10.4168/aard.2018.6.3.174
Abstract
- PURPOSE
This study evaluated the clinical characteristics and risk factors associated with atopic dermatitis patients complicated by eczema herpeticum.
METHODS
This study included 45 patients under the age of 18 with atopic dermatitis complicated by eczema herpeticum in the disease group (ADEH+), and 50 patients under the age of 18 with atopic dermatitis without any episode of eczema herpeticum in the control group (ADEH−). We retrospectively reviewed the clinical features, treatment and prognosis of the 2 groups.
RESULTS
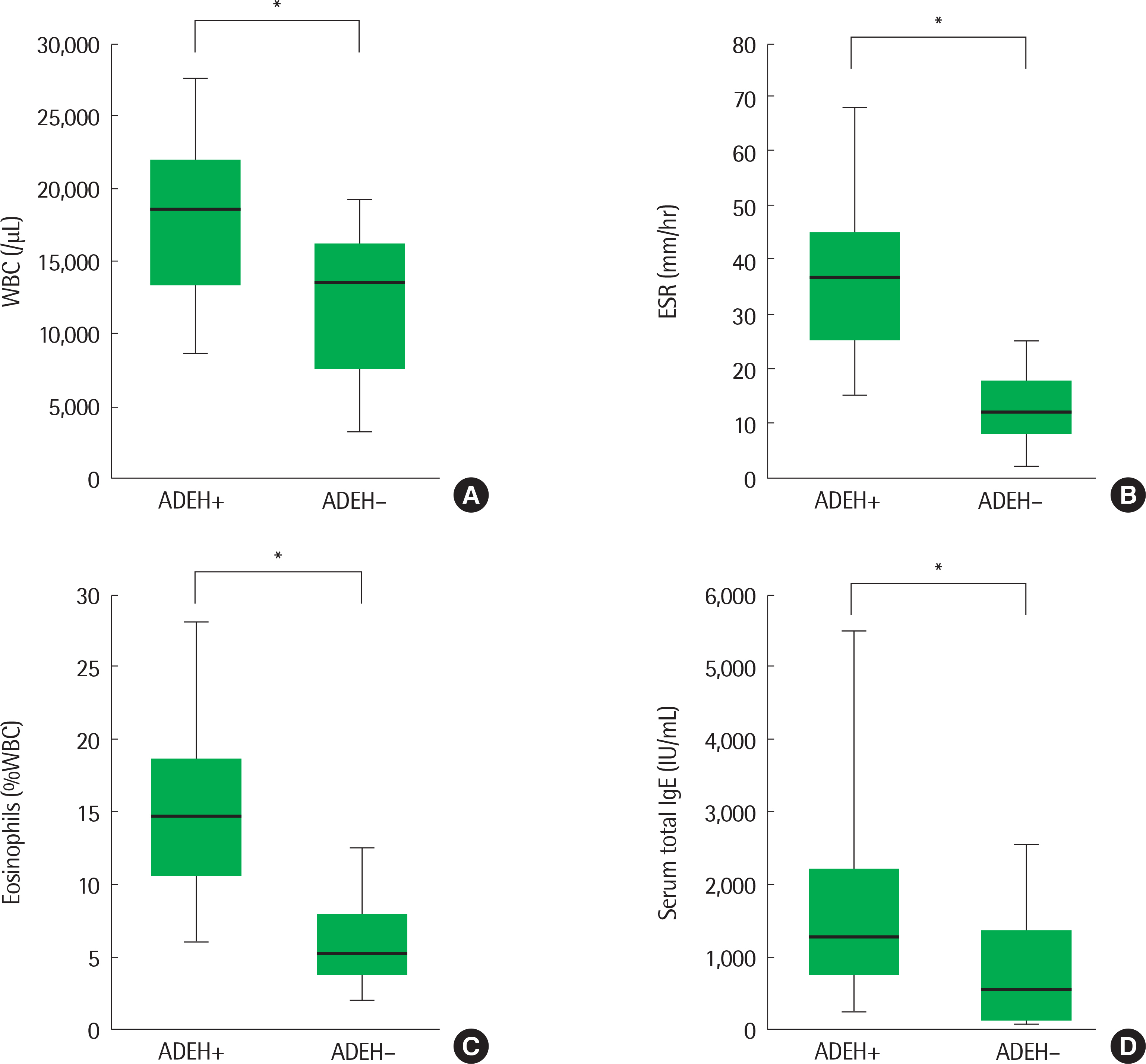
In this study, eczema herpeticum occurred in 2.7% of the AD patients. No significant difference in percentage of boys or mean age was found between the ADEH+ and ADEH− groups. In the ADEH+ group, eczema herpeticum occurred more frequently in the head and neck. Severe atopic dermatitis, recurrent impetigo, IgE−mediated atopic dermatitis and food allergy were identified as the risk factors of eczema herpeticum. The mean white blood cell count, erythrocyte sedimentation rate, percent of eosinophils and total serum IgE were higher in the ADEH+ group than in the ADEH− group. More than 2 recurrences were confirmed in 12 patients (26.7%).
CONCLUSION
In the ADEH+ group, skin lesions were dominant on the head and neck. We revealed that severe atopic dermatitis, frequent impetigo, IgE-mediated atopic dermatitis, and food allergy are risk factors for eczema herpeticum.
MeSH Terms
Figure
Reference
-
1. Ahn K. The prevalence of atopic dermatitis in Korean children. Allergy Asthma Immunol Res. 2016; 8:1–2.
Article2. Lee SI, Kim J, Han Y, Ahn K. A proposal: Atopic Dermatitis Organizer (ADO) guideline for children. Asia Pac Allergy. 2011; 1:53–63.
Article3. Schneider L, Tilles S, Lio P, Boguniewicz M, Beck L, LeBovidge J, et al. Atopic dermatitis: a practice parameter update 2012. J Allergy Clin Immunol. 2013; 131:295–9.e1-27.4. Spergel JM. Epidemiology of atopic dermatitis and atopic march in children. Immunol Allergy Clin North Am. 2010; 30:269–80.
Article5. Bieber T. Atopic dermatitis. N Engl J Med. 2008; 358:1483–94.
Article6. Boguniewicz M, Leung DY. Atopic dermatitis: a disease of altered skin barrier and immune dysregulation. Immunol Rev. 2011; 242:233–46.
Article7. Malik K, Heitmiller KD, Czarnowicki T. An update on the pathophysiology of atopic dermatitis. Dermatol Clin. 2017; 35:317–26.
Article8. McGibbon D. Rook's textbook of dermatology, 7th edition. Clin Exp Dermatol. 2006; 31:178–9.
Article9. Wollenberg A, Wetzel S, Burgdorf WH, Haas J. Viral infections in atopic dermatitis: pathogenic aspects and clinical management. J Allergy Clin Immunol. 2003; 112:667–74.
Article10. Park HS, You CE, Son SJ, Park MY, Whang KU. A clinicopathological study of Kaposi's varicelliform eruption. Korean J Dermatol. 2005; 43:1220–7.11. Liaw FY, Huang CF, Hsueh JT, Chiang CP. Eczema herpeticum: a medical emergency. Can Fam Physician. 2012; 58:1358–61.12. Leung DY. Why is eczema herpeticum unexpectedly rare? Antiviral Res. 2013; 98:153–7.
Article13. Beck LA, Boguniewicz M, Hata T, Schneider LC, Hanifin J, Gallo R, et al. Phenotype of atopic dermatitis subjects with a history of eczema herpeticum. J Allergy Clin Immunol. 2009; 124:260–9. 269.e1-7.
Article14. Hanifin JM, Rajka G. Diagnostic features of atopic dermatitis. Acta Derm Venereol (Stockh). 1980; 92(Suppl):44–7.15. Swart RN, Vermeer BJ, van Der Meer JW, Enschedé FA, Versteeg J. Treatment of eczema herpeticum with acyclovir. Arch Dermatol. 1983; 119:13–6.
Article16. Lin Y, Zhu M, Su Z. The pursuit of balance: an overview of covariate-adaptive randomization techniques in clinical trials. Contemp Clin Trials. 2015; 45(Pt A):21–5.
Article17. Rullo VE, Segato A, Kirsh A, Sole D. Severity scoring of atopic dermatitis: a comparison of two scoring systems. Allergol Immunopathol (Madr). 2008; 36:205–11.
Article18. Zheng T, Yu J, Oh MH, Zhu Z. The atopic march: progression from atopic dermatitis to allergic rhinitis and asthma. Allergy Asthma Immunol Res. 2011; 3:67–73.
Article19. Peng WM, Jenneck C, Bussmann C, Bogdanow M, Hart J, Leung DY, et al. Risk factors of atopic dermatitis patients for eczema herpeticum. J Invest Dermatol. 2007; 127:1261–3.
Article20. Bin L, Kim BE, Brauweiler A, Goleva E, Streib J, Ji Y, et al. Staphylococcus aureus alpha-toxin modulates skin host response to viral infection. J Allergy Clin Immunol. 2012; 130:683–91.e2.21. Gao PS, Rafaels NM, Mu D, Hand T, Murray T, Boguniewicz M, et al. Genetic variants in thymic stromal lymphopoietin are associated with atopic dermatitis and eczema herpeticum. J Allergy Clin Immunol. 2010; 125:1403–7.e4.
Article22. Wollenberg A, Zoch C, Wetzel S, Plewig G, Przybilla B. Predisposing factors and clinical features of eczema herpeticum: a retrospective analysis of 100 cases. J Am Acad Dermatol. 2003; 49:198–205.
Article23. Howell MD, Gao P, Kim BE, Lesley LJ, Streib JE, Taylor PA, et al. The signal transducer and activator of transcription 6 gene (STAT6) increases the propensity of patients with atopic dermatitis toward disseminated viral skin infections. J Allergy Clin Immunol. 2011; 128:1006–14.
Article24. Howell MD, Gallo RL, Boguniewicz M, Jones JF, Wong C, Streib JE, et al. Cytokine milieu of atopic dermatitis skin subverts the innate immune response to vaccinia virus. Immunity. 2006; 24:341–8.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Severe Eczema Herpeticum in an Adult Patient with Atopic Dermatitis Following Herbal Medicine and Acupuncture
- Disseminated Eczema Herpeticum Transmitted by Self-inoculation
- Two Cases of Severe Eczema Herpeticum after Herbal Medication in Children with Atopic Dermatitis
- A Case of Eczema Herpeticum Occurring in Atopic Dermatitis
- Two Cases of Widespread Eczema Herpeticum with Low Serum Vitamin D Levels