Ann Hepatobiliary Pancreat Surg.
2018 May;22(2):173-177. 10.14701/ahbps.2018.22.2.173.
A long-term survival case of advanced biliary cancer with repeated resection due to recurrence in the pancreaticogastrostomy site after pancreaticoduodenectomy
- Affiliations
-
- 1Department of Surgery, Shikoku Central Hospital, Ehime, Japan. shohey440@yahoo.co.jp
- KMID: 2412435
- DOI: http://doi.org/10.14701/ahbps.2018.22.2.173
Abstract
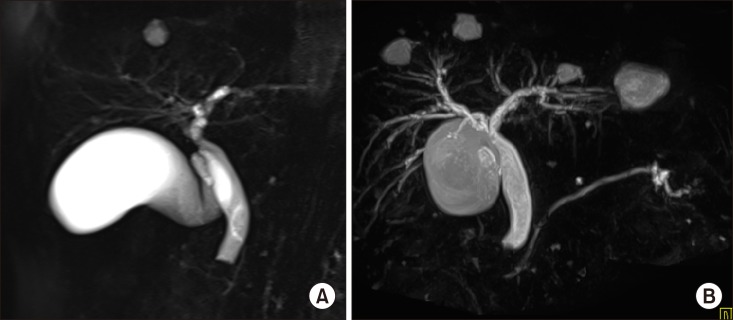
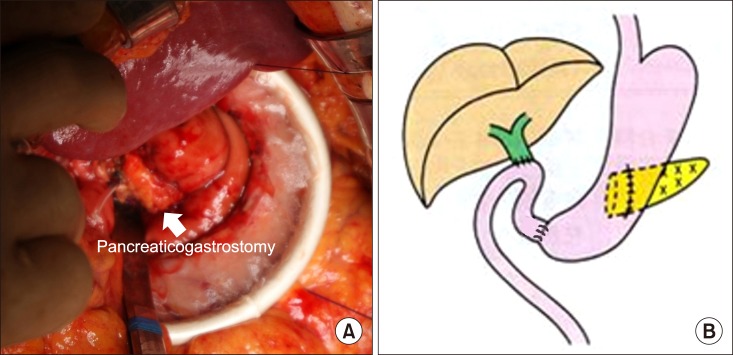
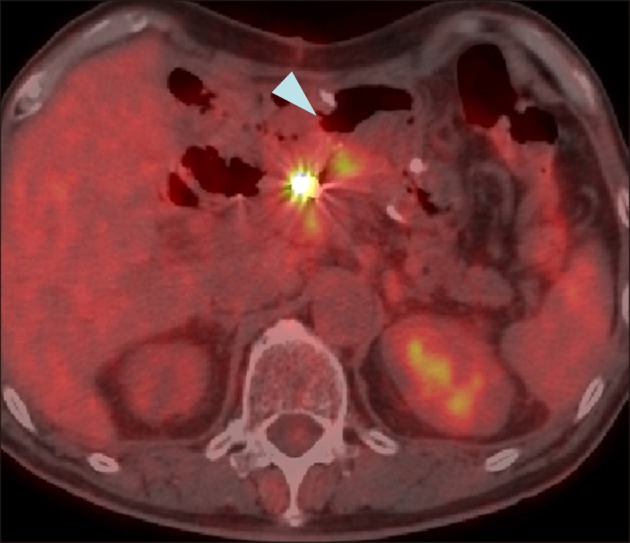
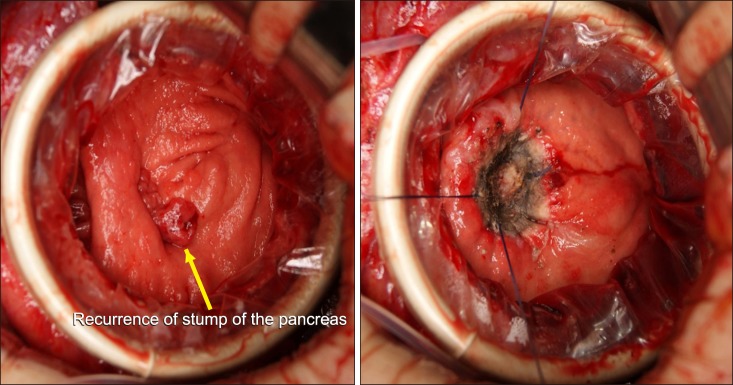
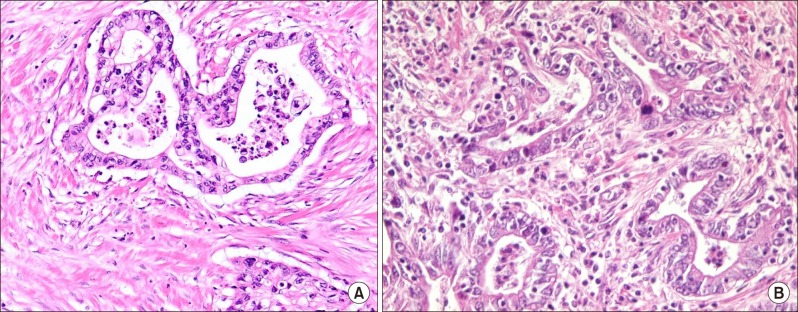
- A 62-year-old man underwent endoscopic mucosal resection for early gastric cancer. The follow-up computed tomography revealed biliary dilatation. The tumor was located in the lower bile duct with biliary dilatation, and no evidence of metastasis in other organs was noted. The patient underwent subtotal stomach-preserving pancreatoduodenectomy with pancreaticogastrostomy and Billroth I anastomosis. At 13 months after the operation, gastrointestinal endoscopy revealed a tumor lesion in the pancreaticogastrostomy site. Computed tomography revealed that the lesion was low enhanced in the pancreaticogastrostomy site and there was no evidence of other distant metastasis. Partial pancreatectomy was performed. Pathological findings of the tumor in the stump of the pancreas revealed findings similar to that of primary biliary carcinoma. Apparently, the patient was diagnosed with recurrence of bile duct cancer via the pancreatic duct. The patient underwent adjuvant chemotherapy for one year subsequent to partial pancreatectomy as the second operation. For 40 months after the second operation, there has been no evidence of recurrence of cancer.
MeSH Terms
Figure
Cited by 1 articles
-
ALKBH5 gene is a novel biomarker that predicts the prognosis of pancreatic cancer: A retrospective multicohort study
Sung Hwan Cho, Mihyang Ha, Yong Hoon Cho, Je Ho Ryu, Kwangho Yang, Kang Ho Lee, Myoung-Eun Han, Sae-Ock Oh, Yun Hak Kim
Ann Hepatobiliary Pancreat Surg. 2018;22(4):305-309. doi: 10.14701/ahbps.2018.22.4.305.
Reference
-
1. Miyakawa S, Ishihara S, Horiguchi A, Takada T, Miyazaki M, Nagakawa T. Biliary tract cancer treatment: 5,584 results from the Biliary Tract Cancer Statistics Registry from 1998 to 2004 in Japan. J Hepatobiliary Pancreat Surg. 2009; 16:1–7. PMID: 19110652.
Article2. Takashima A, Morizane C, Ishii H, Nakamura K, Fukuda H, Okusaka T, et al. Randomized phase II study of gemcitabine plus S-1 combination therapy vs. S-1 in advanced biliary tract cancer: Japan Clinical Oncology Group Study (JCOG0805). Jpn J Clin Oncol. 2010; 40:1189–1191. PMID: 20630899.
Article3. Valle JW. Advances in the treatment of metastatic or unresectable biliary tract cancer. Ann Oncol. 2010; 21(Suppl 7):vii345–vii348. PMID: 20943640.
Article4. Song SC, Heo JS, Choi DW, Choi SH, Kim WS, Kim MJ. Survival benefits of surgical resection in recurrent cholangiocarcinoma. J Korean Surg Soc. 2011; 81:187–194. PMID: 22066120.
Article5. Noji T, Tsuchikawa T, Mizota T, Okamura K, Nakamura T, Tamoto E, et al. Surgery for recurrent biliary carcinoma: results for 27 recurrent cases. World J Surg Oncol. 2015; 13:82. PMID: 25884694.
Article6. Ishikawa O, Ohigashi H, Eguchi H, Yokoyama S, Yamada T, Takachi K, et al. Long-term follow-up of glucose tolerance function after pancreaticoduodenectomy: comparison between pancreaticogastrostomy and pancreaticojejunostomy. Surgery. 2004; 136:617–623. PMID: 15349110.
Article7. Que W, Fang H, Yan B, Li J, Guo W, Zhai W, et al. Pancreaticogastrostomy versus pancreaticojejunostomy after pancreaticoduodenectomy: a meta-analysis of randomized controlled trials. Am J Surg. 2015; 209:1074–1082. PMID: 25743406.8. Bassi C, Falconi M, Molinari E, Salvia R, Butturini G, Sartori N, et al. Reconstruction by pancreaticojejunostomy versus pancreaticogastrostomy following pancreatectomy: results of a comparative study. Ann Surg. 2005; 242:767–771. discussion 771–773. PMID: 16327486.9. Fernández-Cruz L, Cosa R, Blanco L, López-Boado MA, Astudillo E. Pancreatogastrostomy with gastric partition after pylorus-preserving pancreatoduodenectomy versus conventional pancreatojejunostomy: a prospective randomized study. Ann Surg. 2008; 248:930–938. PMID: 19092337.10. Wada H, Numata A, Fukunaga A, Sasamura Y, Takeyama S, Nenohi M. A case of recurrent intraductal papillary mucinous carcinoma at the pancreaticogastrostomy portion. Pancreas. 2012; 27:206–211.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Clinical Review of 123 Cases of Pancreaticoduodenectomy
- Clinical Results in the Treatment of Extrahepatic Bile Duct Cancer and Long-term Survivors' Characteristics after Surgical Resection
- A Case of Long Term Survival in Patient with Early Intrahepatic Recurrence and Extrahepatic Metastasis after Curative Resection of Hepatocellular Carcinoma
- Pancreaticoduodenectomy with combined hepatic artery and portal vein resection after laparoscopic division of pancreaticosplenic ligament due to FOLFIRINOX-induced hepatic toxicity related secondary hypersplenism
- Pancreaticoduodenectomy for recurrence of intraductal papillary neoplasm of bile duct at seven years after curative resection