Ann Surg Treat Res.
2018 Jun;94(6):322-329. 10.4174/astr.2018.94.6.322.
Impact of CT imaging on predicting the surgical management of acute diverticulitis
- Affiliations
-
- 1Department of Surgery, Daegu Catholic University Medical Center, Catholic University of Daegu School of Medicine, Daegu, Korea. gsyangcs@gmail.com
- 2Department of Radiology, Daegu Catholic University Medical Center, Catholic University of Daegu School of Medicine, Daegu, Korea.
- KMID: 2412402
- DOI: http://doi.org/10.4174/astr.2018.94.6.322
Abstract
- PURPOSE
The incidence of colonic diverticular disease is increasing, and several grading systems based on CT findings have been developed. The objective of this study was to define the impact of various CT findings of colonic diverticulitis and to demonstrate which factors affect the need for operative treatment.
METHODS
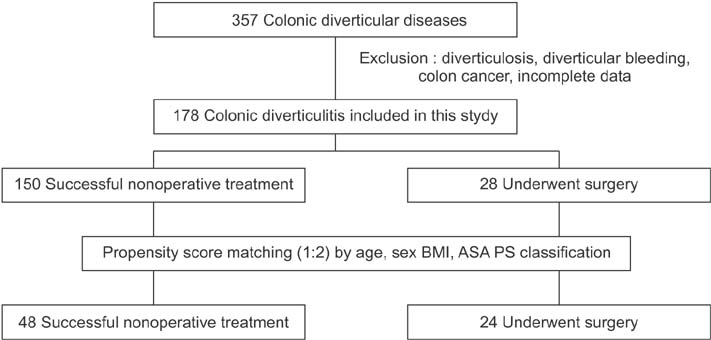
Three hundred fifty-seven patients diagnosed with colonic diverticulitis from January 2010 to July 2016 were retrospectively evaluated. Patients were excluded if pure diverticulosis, diverticular bleeding, colon cancer, or relevant data deficiencies, and the remaining patients (n = 178) were reviewed. Patients were categorized into a successful nonoperation group and an operation group. The operation group was then matched 1:2 with the nonoperative group based on age, gender, American Society of Anesthesiologists physical status classification, and body mass index.
RESULTS
After propensity score matching, there were no significant differences regarding patients' demographic characteristics between the 2 groups. Left location was more associated with need for operation than the right side (79.2% vs. 31.3%, P < 0.001). CT findings such as distant intraperitoneal air, pericolic air, and free fluid were significantly more apparent in the operation group. When these factors were evaluated in a multivariate analysis, distant intraperitoneal air showed statistical significance (P = 0.046) and pericolic air and left location a significant trend (P = 0.071 and P = 0.067, respectively).
CONCLUSION
This study suggests that distant intraperitoneal air is the most important factor in the need for surgery in patients with colonic diverticulitis. Further study will be able to identify more detailed CT findings and verify their significance, and will be helpful in designing practical scoring and classification systems.
MeSH Terms
Figure
Cited by 1 articles
-
Predictive factors for conservative treatment failure of right colonic diverticulitis
Youn Young Park, Soomin Nam, Jeong Hee Han, Jaeim Lee, Chinock Cheong
Ann Surg Treat Res. 2021;100(6):347-355. doi: 10.4174/astr.2021.100.6.347.
Reference
-
1. Kaiser AM, Jiang JK, Lake JP, Ault G, Artinyan A, Gonzalez-Ruiz C, et al. The management of complicated diverticulitis and the role of computed tomography. Am J Gastroenterol. 2005; 100:910–917.
Article2. Chabok A, Pahlman L, Hjern F, Haapaniemi S, Smedh K. AVOD Study Group. Randomized clinical trial of antibiotics in acute uncomplicated diverticulitis. Br J Surg. 2012; 99:532–539.3. Klarenbeek BR, de Korte N, van der Peet DL, Cuesta MA. Review of current classifications for diverticular disease and a translation into clinical practice. Int J Colorectal Dis. 2012; 27:207–214.
Article4. Sher ME, Agachan F, Bortul M, Nogueras JJ, Weiss EG, Wexner SD. Laparoscopic surgery for diverticulitis. Surg Endosc. 1997; 11:264–267.
Article5. Ambrosetti P, Becker C, Terrier F. Colonic diverticulitis: impact of imaging on surgical management -- a prospective study of 542 patients. Eur Radiol. 2002; 12:1145–1149.
Article6. Matrana MR, Margolin DA. Epidemiology and pathophysiology of diverticular disease. Clin Colon Rectal Surg. 2009; 22:141–146.
Article7. Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004; 240:205–213.8. Kim SY, Oh TH, Seo JY, Jeon TJ, Seo DD, Shin WC, et al. The clinical factors for predicting severe diverticulitis in Korea: a comparison with Western countries. Gut Liver. 2012; 6:78–85.
Article9. Park NS, Jeen YT, Choi HS, Kim ES, Kim YJ, Keum B, et al. Risk factors for severe diverticulitis in computed tomography-confirmed acute diverticulitis in Korea. Gut Liver. 2013; 7:443–449.
Article10. Tan JP, Barazanchi AW, Singh PP, Hill AG, Maccormick AD. Predictors of acute diverticulitis severity: a systematic review. Int J Surg. 2016; 26:43–52.
Article11. Brian West A. The pathology of diverticulosis: classical concepts and mucosal changes in diverticula. J Clin Gastroenterol. 2006; 40:Suppl 3. S126–S131.
Article12. Hall JF, Roberts PL, Ricciardi R, Read T, Scheirey C, Wald C, et al. Long-term follow-up after an initial episode of diverticulitis: what are the predictors of recurrence? Dis Colon Rectum. 2011; 54:283–288.
Article13. Ambrosetti P, Grossholz M, Becker C, Terrier F, Morel P. Computed tomography in acute left colonic diverticulitis. Br J Surg. 1997; 84:532–534.
Article14. Poletti PA, Platon A, Rutschmann O, Kinkel K, Nyikus V, Ghiorghiu S, et al. Acute left colonic diverticulitis: can CT findings be used to predict recurrence? AJR Am J Roentgenol. 2004; 182:1159–1165.15. Buchs NC, Konrad-Mugnier B, Jannot AS, Poletti PA, Ambrosetti P, Gervaz P. Assessment of recurrence and complications following uncomplicated diverticulitis. Br J Surg. 2013; 100:976–979.
Article16. Sallinen V, Mali J, Leppaniemi A, Mentula P. Assessment of risk for recurrent diverticulitis: a proposal of risk score for complicated recurrence. Medicine (Baltimore). 2015; 94:e557.17. Sallinen VJ, Leppaniemi AK, Mentula PJ. Staging of acute diverticulitis based on clinical, radiologic, and physiologic parameters. J Trauma Acute Care Surg. 2015; 78:543–551.
Article18. Shaikh S, Krukowski ZH. Outcome of a conservative policy for managing acute sigmoid diverticulitis. Br J Surg. 2007; 94:876–879.
Article19. Trenti L, Kreisler E, Galvez A, Golda T, Frago R, Biondo S. Long-term evolution of acute colonic diverticulitis after successful medical treatment. World J Surg. 2015; 39:266–274.
Article20. Costi R, Cauchy F, Le Bian A, Honart JF, Creuze N, Smadja C. Challenging a classic myth: pneumoperitoneum associated with acute diverticulitis is not an indication for open or laparoscopic emergency surgery in hemodynamically stable patients. A 10-year experience with a nonoperative treatment. Surg Endosc. 2012; 26:2061–2071.
Article21. Bridoux V, Antor M, Schwarz L, Cahais J, Khalil H, Michot F, et al. Elective operation after acute complicated diverticulitis: is it still mandatory? World J Gastroenterol. 2014; 20:8166–8172.
Article22. Sallinen VJ, Mentula PJ, Leppäniemi AK. Nonoperative management of perforated diverticulitis with extraluminal air is safe and effective in selected patients. Dis Colon Rectum. 2014; 57:875–881.
Article23. Dharmarajan S, Hunt SR, Birnbaum EH, Fleshman JW, Mutch MG. The efficacy of nonoperative management of acute complicated diverticulitis. Dis Colon Rectum. 2011; 54:663–671.
Article