Clin Orthop Surg.
2017 Sep;9(3):310-316. 10.4055/cios.2017.9.3.310.
Lumbar Single-Level Dynamic Stabilization with Semi-Rigid and Full Dynamic Systems: A Retrospective Clinical and Radiological Analysis of 71 Patients
- Affiliations
-
- 1Department of Neurosurgery, Koc University School of Medicine, Istanbul, Turkey. alifahirozer@gmail.com
- 2Department of Neurosurgery, Mustafa Kemal University, Hatay, Turkey.
- 3Department of Biomedical Engineering, Medipol University, Istanbul, Turkey.
- KMID: 2412267
- DOI: http://doi.org/10.4055/cios.2017.9.3.310
Abstract
- BACKGROUND
This study compares the clinical and radiological results of three most commonly used dynamic stabilization systems in the field of orthopedic surgery.
METHODS
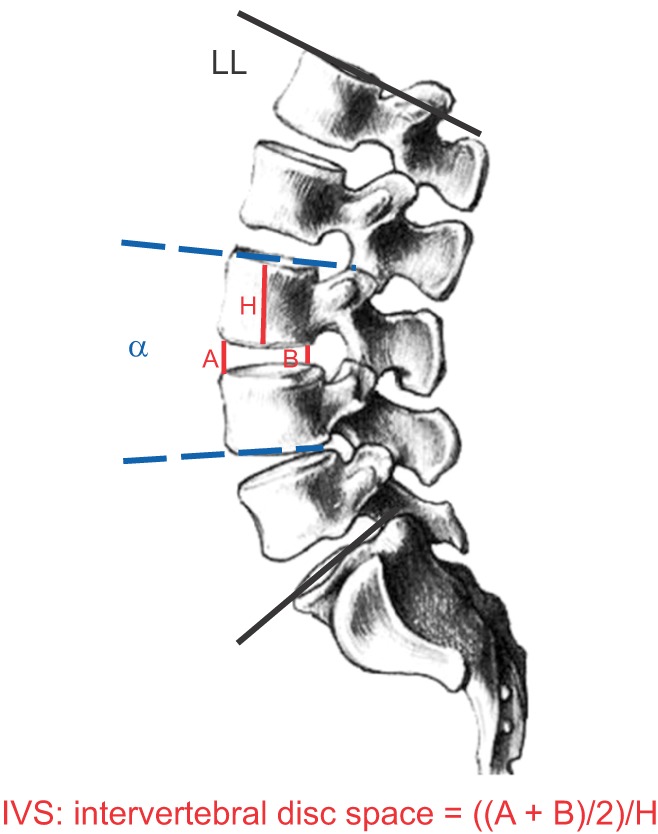
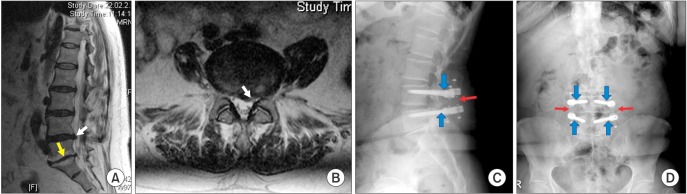
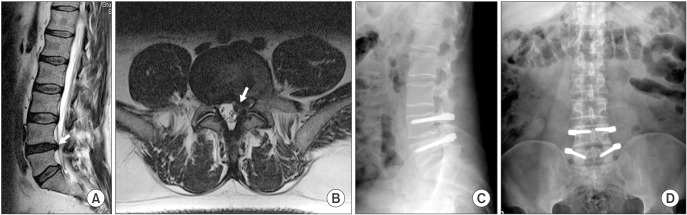
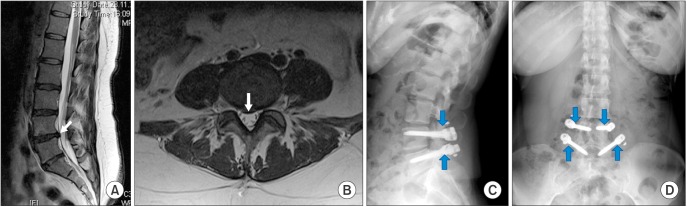
A total of 71 patients underwent single-level posterior transpedicular dynamic stabilization between 2011 and 2014 due to lumbar degenerative disc disease. Three different dynamic systems used include: (1) the Dynesys system; (2) a dynamic screw with a PEEK rod; and (3) a full dynamic system (a dynamic screw with a dynamic rod; BalanC). The mean patient age was 45.8 years. The mean follow-up was 29.7 months. Clinical and radiological data were obtained for each patient preoperatively and at 6, 12, and 24 months of follow-up.
RESULTS
Clinical outcomes were significantly improved in all patients. There were no significant differences in the radiological outcomes among the groups divided according to the system used. Screw loosening was detected in 2 patients, and 1 patient developed screw breakage. All patients with screw loosening or breakage underwent revision surgery.
CONCLUSIONS
Each procedure offered satisfactory outcome regardless of which system was applied.
Keyword
MeSH Terms
Figure
Reference
-
1. Oktenoglu T, Ozer AF, Sasani M, et al. Posterior dynamic stabilization in the treatment of lumbar degenerative disc disease: 2-year follow-up. Minim Invasive Neurosurg. 2010; 53(3):112–116. PMID: 20809451.
Article2. Roberts S, Evans H, Trivedi J, Menage J. Histology and pathology of the human intervertebral disc. J Bone Joint Surg Am. 2006; 88(Suppl 2):10–14.
Article3. Graf H. Lumbar instability: surgical treatment without fusion. Rachis. 1992; 4(2):123–137.4. Smith D, McMurray N, Disler P. Early intervention for acute back injury: can we finally develop an evidence-based approach? Clin Rehabil. 2002; 16(1):1–11.
Article5. Harrop JS, Youssef JA, Maltenfort M, et al. Lumbar adjacent segment degeneration and disease after arthrodesis and total disc arthroplasty. Spine (Phila Pa 1976). 2008; 33(15):1701–1707. PMID: 18594464.
Article6. Fay LY, Wu JC, Tsai TY, et al. Intervertebral disc rehydration after lumbar dynamic stabilization: magnetic resonance image evaluation with a mean followup of four years. Adv Orthop. 2013; 2013:437570. PMID: 23738082.
Article7. Gomleksiz C, Sasani M, Oktenoglu T, Ozer AF. A short history of posterior dynamic stabilization. Adv Orthop. 2012; 2012:629698. PMID: 23326674.
Article8. Song JJ, Barrey CY, Ponnappan RK, Bessey JT, Shimer AL, Vaccaro AR. Pedicle screw-based dynamic stabilization of the lumbar spine. Pan Arab J Neurosurg. 2010; 14(1):1–8.9. Bozkus H, Senoglu M, Baek S, et al. Dynamic lumbar pedicle screw-rod stabilization: in vitro biomechanical comparison with standard rigid pedicle screw-rod stabilization. J Neurosurg Spine. 2010; 12(2):183–189. PMID: 20121354.10. Oktenoglu T, Erbulut DU, Kiapour A, et al. Pedicle screw-based posterior dynamic stabilisation of the lumbar spine: in vitro cadaver investigation and a finite element study. Comput Methods Biomech Biomed Engin. 2015; 18(11):1252–1261. PMID: 24708377.11. Wurgler-Hauri CC, Kalbarczyk A, Wiesli M, Landolt H, Fandino J. Dynamic neutralization of the lumbar spine after microsurgical decompression in acquired lumbar spinal stenosis and segmental instability. Spine (Phila Pa 1976). 2008; 33(3):E66–E72. PMID: 18303447.12. Grob D, Benini A, Junge A, Mannion AF. Clinical experience with the Dynesys semirigid fixation system for the lumbar spine: surgical and patient-oriented outcome in 50 cases after an average of 2 years. Spine (Phila Pa 1976). 2005; 30(3):324–331. PMID: 15682014.13. Strempel A. Nonfusion stabilization of the degenerated lumbar spine with Cosmic. In : Kim DH, Cammisa FP, Fessler RG, editors. Dynamic reconstruction of the spine. New York, NY: Thieme Medical Publishers. Inc.;2006. p. 330–339.14. Strempel A, Moosmann D, Stoss C, Martin A. Stabilisation of the degenerated lumbar spine in the nonfusion technique with cosmic posterior dynamic system. Wall St J. 2006; 1(1):40–47.15. von Strempel A, Neekritz A, de Muelenaere P, du Toit G. Dynamic versus rigid spinal implants. In : Gunzburg R, Szpalski M, editors. Lumbar spinal stenosis. Philadelphia, PA: Lippincott Williams & Wilkins;2000. p. 275–285. .16. Erbulut DU, Kiapour A, Oktenoglu T, Ozer AF, Goel VK. A computational biomechanical investigation of posterior dynamic instrumentation: combination of dynamic rod and hinged (dynamic) screw. J Biomech Eng. 2014; 136(5):051007. PMID: 24599026.
Article17. Erbulut DU, Zafarparandeh I, Hassan CR, Lazoglu I, Ozer AF. Determination of the biomechanical effect of an interspinous process device on implanted and adjacent lumbar spinal segments using a hybrid testing protocol: a finiteelement study. J Neurosurg Spine. 2015; 23(2):200–208. PMID: 25932601.
Article18. Mohi Eldin MM, Ali AM. Lumbar transpedicular implant failure: a clinical and surgical challenge and its radiological assessment. Asian Spine J. 2014; 8(3):281–297. PMID: 24967042.
Article19. Park P, Garton HJ, Gala VC, Hoff JT, McGillicuddy JE. Adjacent segment disease after lumbar or lumbosacral fusion: review of the literature. Spine (Phila Pa 1976). 2004; 29(17):1938–1944. PMID: 15534420.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Does the Addition of a Dynamic Pedicle Screw to a Fusion Segment Prevent Adjacent Segment Pathology in the Lumbar Spine?
- The Incidence of Adjacent Segment Degeneration after the Use of a Versatile Dynamic Hybrid Stabilization Device in Lumbar Stenosis: Results of a 5–8-Year Follow-up
- Pedicle Screw-based Dynamic Stabilization with a Hinged Screw Head System in the Treatment of Lumbar Degenerative Disorders
- NFlex Dynamic Stabilization System : Two-Year Clinical Outcomes of Multi-Center Study
- Severe Retrolisthesis at the Adjacent Segment after Lumbar Fusion Combined with Dynamic Stabilization