Cancer Res Treat.
2018 Apr;50(2):575-581. 10.4143/crt.2017.182.
Low-Dose Radiation Therapy for Primary Conjunctival Marginal Zone B-Cell Lymphoma
- Affiliations
-
- 1Department of Ophthalmology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. eyeminded@skku.edu
- 2Department of Radiation Oncology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. ahnyc@skku.edu
- 3Division of Hematology and Oncology, Department of Internal Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 4Department of Pathology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- KMID: 2411145
- DOI: http://doi.org/10.4143/crt.2017.182
Abstract
- PURPOSE
The purpose of this study was to evaluate the clinical features and the long-term outcomes of primary conjunctival marginal zone B-cell lymphoma (MZBCL) patients who were treated with radiation therapy (RT).
MATERIALS AND METHODS
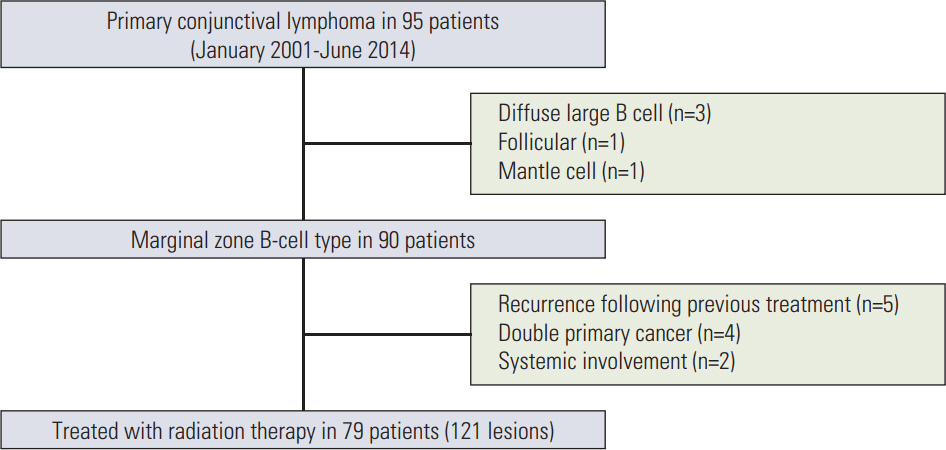
Retrospective data of 79 patients with 121 primary conjunctival MZBCL lesions were collected from January 1, 2001 till June 30, 2014. All lesions were treated by local RT (26 Gy) with patient-specific customized lens-shielding device.
RESULTS
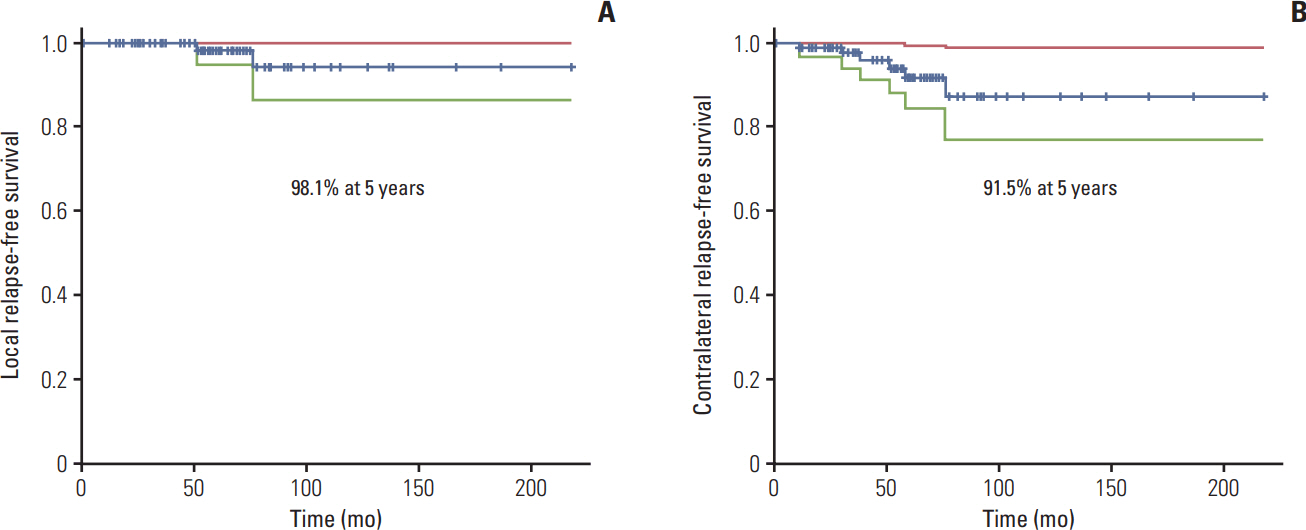
The current Korean patients' cohort showed younger median age at diagnosis (38 years), great female preponderance (78.5%) and more frequent bilateral involvement (53.2%) than the previous studies. Following 26 Gy's RT, excellent clinical outcomes were achieved: 5-year rates of overall survival, local relapse-free survival, and contralateral relapse-free survival were 100%, 98.1%, and 91.5%, respectively. Two patients (2.5%) developed local relapse and five (6.3%) developed relapse at initially uninvolved contralateral conjunctiva with median interval of 52.9 months, and late adverse events of grade 2 and 3 occurred in seven (8.8%) and two (2.5%) patients, respectively.
CONCLUSION
26 Gy's RT was highly effective and safe, with the use of lens-shielding device, in treating patients with primary conjunctival MZBCL.
MeSH Terms
Figure
Reference
-
References
1. Kirkegaard MM, Coupland SE, Prause JU, Heegaard S. Malignant lymphoma of the conjunctiva. Surv Ophthalmol. 2015; 60:444–58.
Article2. Kirkegaard MM, Rasmussen PK, Coupland SE, Esmaeli B, Finger PT, Graue GF, et al. Conjunctival lymphoma: an international multicenter retrospective study. JAMA Ophthalmol. 2016; 134:406–14.3. Matsuo T, Ichimura K, Yoshino T. Spontaneous regression of bilateral conjunctival extranodal marginal zone B-cell lymphoma of mucosa-associated lymphoid tissue. J Clin Exp Hematop. 2007; 47:79–81.
Article4. Tanimoto K, Kaneko A, Suzuki S, Sekiguchi N, Maruyama D, Kim SW, et al. Long-term follow-up results of no initial therapy for ocular adnexal MALT lymphoma. Ann Oncol. 2006; 17:135–40.
Article5. Han JJ, Kim TM, Jeon YK, Kim MK, Khwarg SI, Kim CW, et al. Long-term outcomes of first-line treatment with doxycycline in patients with previously untreated ocular adnexal marginal zone B cell lymphoma. Ann Hematol. 2015; 94:575–81.
Article6. Ferreri AJ, Govi S, Pasini E, Mappa S, Bertoni F, Zaja F, et al. Chlamydophila psittaci eradication with doxycycline as firstline targeted therapy for ocular adnexae lymphoma: final results of an international phase II trial. J Clin Oncol. 2012; 30:2988–94.7. Ohga S, Nakamura K, Shioyama Y, Sasaki T, Yoshitake T, Atsumi K, et al. Radiotherapy for early-stage primary ocular adnexal mucosa-associated lymphoid tissue lymphoma. Anticancer Res. 2013; 33:5575–8.8. Uno T, Isobe K, Shikama N, Nishikawa A, Oguchi M, Ueno N, et al. Radiotherapy for extranodal, marginal zone, B-cell lymphoma of mucosa-associated lymphoid tissue originating in the ocular adnexa: a multiinstitutional, retrospective review of 50 patients. Cancer. 2003; 98:865–71.
Article9. Ferrufino-Ponce ZK, Henderson BA. Radiotherapy and cataract formation. Semin Ophthalmol. 2006; 21:171–80.
Article10. Hashimoto N, Sasaki R, Nishimura H, Yoshida K, Miyawaki D, Nakayama M, et al. Long-term outcome and patterns of failure in primary ocular adnexal mucosa-associated lymphoid tissue lymphoma treated with radiotherapy. Int J Radiat Oncol Biol Phys. 2012; 82:1509–14.
Article11. Hoskin PJ, Kirkwood AA, Popova B, Smith P, Robinson M, Gallop-Evans E, et al. 4 Gy versus 24 Gy radiotherapy for patients with indolent lymphoma (FORT): a randomised phase 3 non-inferiority trial. Lancet Oncol. 2014; 15:457–63.
Article12. Nam H, Ahn YC, Kim YD, Ko Y, Kim WS. Prognostic significance of anatomic subsites: results of radiation therapy for 66 patients with localized orbital marginal zone B cell lymphoma. Radiother Oncol. 2009; 90:236–41.
Article13. Woolf DK, Kuhan H, Shoffren O, Akinnawo EM, Sivagurunathan B, Boyce H, et al. Outcomes of primary lymphoma of the ocular adnexa (orbital lymphoma) treated with radiotherapy. Clin Oncol (R Coll Radiol). 2015; 27:153–9.
Article14. Goda JS, Le LW, Lapperriere NJ, Millar BA, Payne D, Gospodarowicz MK, et al. Localized orbital mucosa-associated lymphoma tissue lymphoma managed with primary radiation therapy: efficacy and toxicity. Int J Radiat Oncol Biol Phys. 2011; 81:e659–66.
Article15. Harada K, Murakami N, Kitaguchi M, Sekii S, Takahashi K, Yoshio K, et al. Localized ocular adnexal mucosa-associated lymphoid tissue lymphoma treated with radiation therapy: a long-term outcome in 86 patients with 104 treated eyes. Int J Radiat Oncol Biol Phys. 2014; 88:650–4.
Article16. Parikh RR, Moskowitz BK, Maher E, Della Rocca D, Della Rocca R, Culliney B, et al. Long-term outcomes and patterns of failure in orbital lymphoma treated with primary radiotherapy. Leuk Lymphoma. 2015; 56:1266–70.
Article17. Ferry JA, Fung CY, Zukerberg L, Lucarelli MJ, Hasserjian RP, Preffer FI, et al. Lymphoma of the ocular adnexa: a study of 353 cases. Am J Surg Pathol. 2007; 31:170–84.
Article18. Tran KH, Campbell BA, Fua T, MacManus M, Ryan G, Chesson B, et al. Efficacy of low dose radiotherapy for primary orbital marginal zone lymphoma. Leuk Lymphoma. 2013; 54:491–6.
Article19. Bayraktar S, Bayraktar UD, Stefanovic A, Lossos IS. Primary ocular adnexal mucosa-associated lymphoid tissue lymphoma (MALT): single institution experience in a large cohort of patients. Br J Haematol. 2011; 152:72–80.
Article20. Ohga S, Nakamura K, Shioyama Y, Sasaki T, Yamaguchi T, Yoshitake T, et al. Treatment outcome of radiotherapy for localized primary ocular adnexal MALT lymphoma: prognostic effect of the AJCC tumor-node-metastasis clinical staging system. Anticancer Res. 2015; 35:3591–7.21. Yahalom J, Illidge T, Specht L, Hoppe RT, Li YX, Tsang R, et al. Modern radiation therapy for extranodal lymphomas: field and dose guidelines from the International Lymphoma Radiation Oncology Group. Int J Radiat Oncol Biol Phys. 2015; 92:11–31.
Article22. Goda JS, Gospodarowicz M, Pintilie M, Wells W, Hodgson DC, Sun A, et al. Long-term outcome in localized extranodal mucosa-associated lymphoid tissue lymphomas treated with radiotherapy. Cancer. 2010; 116:3815–24.
Article23. Aronow ME, Portell CA, Rybicki LA, Sweetenham JW, Singh AD. Ocular adnexal lymphoma: assessment of a tumor-nodemetastasis staging system. Ophthalmology. 2013; 120:1915–9.
Article24. Henk JM, Whitelocke RA, Warrington AP, Bessell EM. Radiation dose to the lens and cataract formation. Int J Radiat Oncol Biol Phys. 1993; 25:815–20.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Primary Cutaneous Marginal Zone B-cell Lymphoma
- Two Cases of Primary Cutaneous Marginal Zone B-cell Lymphoma
- A Case of Primary Nodal Type Marginal Zone B-Cell Lymphoma of the Intra-Parotid Lymph Node Mistaken to Primary Benign Parotid Mass
- Bilateral Conjunctival Mucosa-Associated Lymphoid Tissue (MALT) Lymphoma Misdiagnosed as Allergic Conjunctivitis
- A Case of Primary Gastric Marginal Zone B-Cell Lymphoma Presenting as Multiple Polyps