Clin Endosc.
2018 Mar;51(2):161-166. 10.5946/ce.2017.087.
Retention Esophagitis as a Significant Clinical Predictor of Progression to Esophageal Cancer in Achalasia
- Affiliations
-
- 1Department of Internal Medicine, Gangnam Severance Hospital, Yonsei University College of Medicine, Seoul, Korea. hjpark21@yuhs.ac
- 2Digestive Disease Center and Research Institute, Soonchunhyang University School of Medicine, Bucheon, Korea.
- 3Department of Pathology, Gangnam Severance Hospital, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 2410983
- DOI: http://doi.org/10.5946/ce.2017.087
Abstract
- BACKGROUND/AIMS
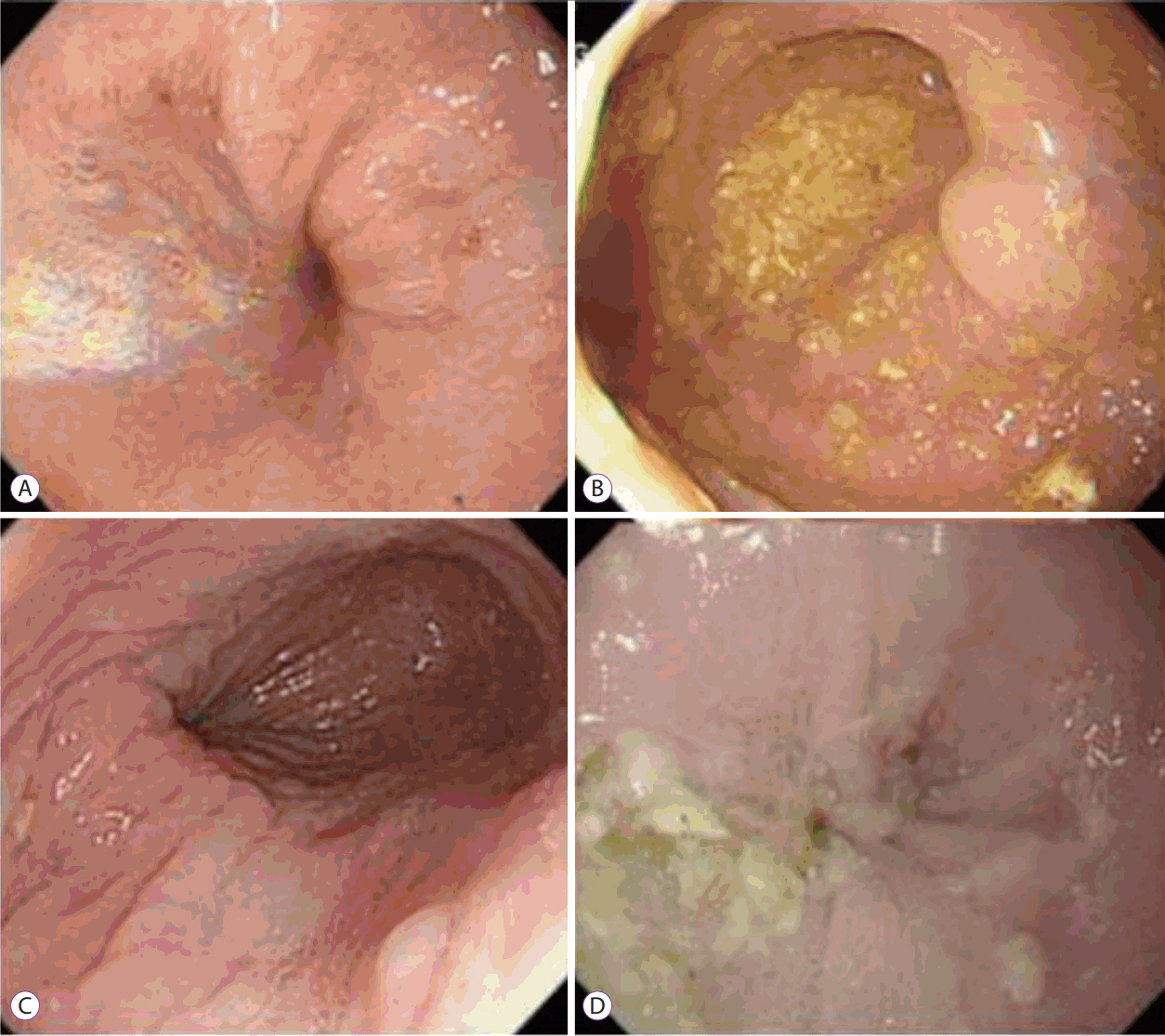
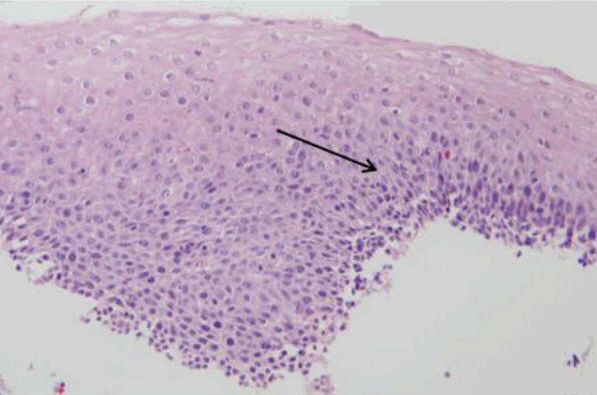
Chronic liquid and/or food stasis caused by retention esophagitis (RE) in achalasia is a notable endoscopic finding because of the presence of a thickened or whitish esophageal mucosa and histologically altered squamous hyperplasia. We aimed to identify the clinical features of RE associated with achalasia and to clarify the clinical definition of RE in achalasia as a precancerous lesion identified by analyzing biomarker expressions.
METHODS
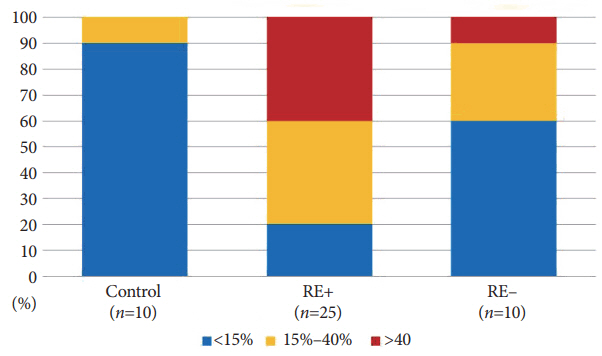
From 2006 to 2015, we retrospectively reviewed 37 patients with achalasia without previous treatment. Among them, 21 patients had diagnostic findings of RE (RE+) and 16 patients had no diagnostic findings of RE (RE−). Immunohistochemical staining of p53, p16, and Ki-67 was performed on the endoscopic biopsy tissues from the patients with achalasia and 10 control patients with non-obstructive dysphagia.
RESULTS
The symptom duration and transit delay were significantly longer in the RE+ group than in the RE− group. We found particularly high p53 positivity rates in the RE+ group (p<0.001). The rate of p16 expression was also significantly higher in the RE+ group than in the other two groups (p=0.003).
CONCLUSIONS
A high p53 expression rate was more frequently found in the RE+ group than in the other two groups. RE could be a meaningful clinical feature of achalasia for predicting esophageal carcinogenesis.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
Retention Esophagitis in Patients with Achalasia Requires Cancer Surveillance
Eun Jeong Gong, Do Hoon Kim
Clin Endosc. 2018;51(2):111-112. doi: 10.5946/ce.2018.037.Non-Exposure Endoscopic-Laparoscopic Cooperative Surgery for Stomach Tumors
Hyo-Jung Oh, Chan-Young Kim
Clin Endosc. 2018;51(2):113-114. doi: 10.5946/ce.2018.048.
Reference
-
1. Moonen A, Boeckxstaens G. Current diagnosis and management of achalasia. J Clin Gastroenterol. 2014; 48:484–490.
Article2. Vaezi MF, Pandolfino JE, Vela MF. ACG clinical guideline: diagnosis and management of achalasia. Am J Gastroenterol. 2013; 108:1238–1249. quiz 1250.
Article3. Ates F, Vaezi MF. The pathogenesis and management of achalasia: current status and future directions. Gut Liver. 2015; 9:449–463.
Article4. Boeckxstaens GE, Zaninotto G, Richter JE. Achalasia. Lancet. 2014; 383:83–93.
Article5. Streitz JM Jr, Ellis FH Jr, Gibb SP, Heatley GM. Achalasia and squamous cell carcinoma of the esophagus: analysis of 241 patients. Ann Thorac Surg. 1995; 59:1604–1609.
Article6. Dunaway PM, Wong RK. Risk and surveillance intervals for squamous cell carcinoma in achalasia. Gastrointest Endosc Clin N Am. 2001; 11:425–434. ix.
Article7. Leeuwenburgh I, Scholten P, Alderliesten J, et al. Long-term esophageal cancer risk in patients with primary achalasia: a prospective study. Am J Gastroenterol. 2010; 105:2144–2149.
Article8. Chino O, Kijima H, Shimada H, et al. Clinicopathological studies of esophageal carcinoma in achalasia: analyses of carcinogenesis using histological and immunohistochemical procedures. Anticancer Res. 2000; 20:3717–3722.9. Shields TW, LoCicero J 3rd, Reed CE, Feins RH. General thoracic surgery. 7th ed. Philadelphia (PA): Lippincott Williams & Wilkins;2009.10. Crookes PF, Corkill S, DeMeester TR. Gastroesophageal reflux in achalasia. When is reflux really reflux? Dig Dis Sci. 1997; 42:1354–1361.
Article11. Kiraly A, Illés A, Undi S, Varga G, Kalmár K, Horváth PO. Gastroesophageal reflux disease progressing to achalasia. Dis Esophagus. 2005; 18:355–358.12. Goldblum JR, Rice TW, Richter JE. Histopathologic features in esophagomyotomy specimens from patients with achalasia. Gastroenterology. 1996; 111:648–654.
Article13. Goldblum JR, Whyte RI, Orringer MB, Appelman HD. Achalasia. A morphologic study of 42 resected specimens. Am J Surg Pathol. 1994; 18:327–337.14. Lehman MB, Clark SB, Ormsby AH, Rice TW, Richter JE, Goldblum JR. Squamous mucosal alterations in esophagectomy specimens from patients with end-stage achalasia. Am J Surg Pathol. 2001; 25:1413–1418.
Article15. Minami H, Isomoto H, Miuma S, et al. New endoscopic indicator of esophageal achalasia: “pinstripe pattern”. PLoS One. 2015; 10:e0101833.
Article16. Leeuwenburgh I, Gerrits MM, Capello A, et al. Expression of p53 as predictor for the development of esophageal cancer in achalasia patients. Dis Esophagus. 2010; 23:506–511.17. Sikkema M, Kerkhof M, Steyerberg EW, et al. Aneuploidy and overexpression of Ki67 and p53 as markers for neoplastic progression in Barrett’s esophagus: a case-control study. Am J Gastroenterol. 2009; 104:2673–2680.
Article18. Meijssen MA, Tilanus HW, van Blankenstein M, Hop WC, Ong GL. Achalasia complicated by oesophageal squamous cell carcinoma: a prospective study in 195 patients. Gut. 1992; 33:155–158.
Article19. Belsey R. Functional disease of the esophagus. J Thorac Cardiovasc Surg. 1966; 52:164–188.
Article20. Raymond L, Lach B, Shamji FM. Inflammatory aetiology of primary oesophageal achalasia: an immunohistochemical and ultrastructural study of Auerbach’s plexus. Histopathology. 1999; 35:445–453.
Article21. Sherr CJ. Cancer cell cycles. Science. 1996; 274:1672–1677.
Article22. Boller D, Spieler P, Schoenegg R, et al. Lugol chromoendoscopy combined with brush cytology in patients at risk for esophageal squamous cell carcinoma. Surg Endosc. 2009; 23:2748–2754.
Article