Clin Endosc.
2018 Mar;51(2):142-149. 10.5946/ce.2017.102.
Advanced Therapeutic Gastrointestinal Endoscopy in Children – Today and Tomorrow
- Affiliations
-
- 1Department of Gastroenterology, Asian Institute of Gastroenterology, Hyderabad, Telangana, India. aigindia@yahoo.co.in
- KMID: 2410980
- DOI: http://doi.org/10.5946/ce.2017.102
Abstract
- Gastrointestinal (GI) endoscopy plays an indispensable role in the diagnosis and management of various pediatric GI disorders. While the pace of development of pediatric GI endoscopy has increased over the years, it remains sluggish compared to the advancements in GI endoscopic interventions available in adults. The predominant reasons that explain this observation include lack of formal training courses in advanced pediatric GI interventions, economic constraints in establishing a pediatric endoscopy unit, and unavailability of pediatric-specific devices and accessories. However, the situation is changing and more pediatric GI specialists are now performing complex GI procedures such as endoscopic retrograde cholangiopancreatography and endoscopic ultrasonography for various pancreatico-biliary diseases and more recently, per-oral endoscopic myotomy for achalasia cardia. Endoscopic procedures are associated with reduced morbidity and mortality compared to open surgery for GI disorders. Notable examples include chronic pancreatitis, pancreatic fluid collections, various biliary diseases, and achalasia cardia for which previously open surgery was the treatment modality of choice. A solid body of evidence supports the safety and efficacy of endoscopic management in adults. However, additions continue to be made to literature describing the pediatric population. An important consideration in children includes size of children, which in turn determines the selection of endoscopes and type of sedation that can be used for the procedure.
Keyword
MeSH Terms
Figure
Reference
-
1. ASGE Standards of Practice Committee, Lightdale JR, Acosta R, et al. Modifications in endoscopic practice for pediatric patients. Gastrointest Endosc. 2014; 79:699–710.2. Thomson M, Tringali A, Dumonceau JM, et al. Paediatric gastrointestinal endoscopy: European society for paediatric gastroenterology hepatology and nutrition and European society of gastrointestinal endoscopy guidelines. J Pediatr Gastroenterol Nutr. 2017; 64:133–153.
Article3. Tringali A, Thomson M, Dumonceau JM, et al. Pediatric gastrointestinal endoscopy: European society of gastrointestinal endoscopy (ESGE) and European society for paediatric gastroenterology hepatology and nutrition (ESPGHAN) guideline executive summary. Endoscopy. 2017; 49:83–91.
Article4. Varadarajulu S, Wilcox CM, Hawes RH, Cotton PB. Technical outcomes and complications of ERCP in children. Gastrointest Endosc. 2004; 60:367–371.
Article5. Cheng CL, Fogel EL, Sherman S, et al. Diagnostic and therapeutic endoscopic retrograde cholangiopancreatography in children: a large series report. J Pediatr Gastroenterol Nutr. 2005; 41:445–453.
Article6. Issa H, Al-Haddad A, Al-Salem AH. Diagnostic and therapeutic ERCP in the pediatric age group. Pediatr Surg Int. 2007; 23:111–116.
Article7. Dua K, Miranda A, Santharam R, Ramanujam S, Werlin S. ERCP in the evaluation of abdominal pain in children. Gastrointest Endosc. 2008; 68:1081–1085.
Article8. Otto AK, Neal MD, Slivka AN, Kane TD. An appraisal of endoscopic retrograde cholangiopancreatography (ERCP) for pancreaticobiliary disease in children: our institutional experience in 231 cases. Surg Endosc. 2011; 25:2536–2540.9. Enestvedt BK, Tofani C, Lee DY, et al. Endoscopic retrograde cholangiopancreatography in the pediatric population is safe and efficacious. J Pediatr Gastroenterol Nutr. 2013; 57:649–654.
Article10. Agarwal J, Nageshwar Reddy D, Talukdar R, et al. ERCP in the management of pancreatic diseases in children. Gastrointest Endosc. 2014; 79:271–278.
Article11. Saito T, Terui K, Mitsunaga T, et al. Role of pediatric endoscopic retrograde cholangiopancreatography in an era stressing less-invasive imaging modalities. J Pediatr Gastroenterol Nutr. 2014; 59:204–209.
Article12. Giefer MJ, Kozarek RA. Technical outcomes and complications of pediatric ERCP. Surg Endosc. 2015; 29:3543–3550.
Article13. Rosen JD, Lane RS, Martinez JM, et al. Success and safety of endoscopic retrograde cholangiopancreatography in children. J Pediatr Surg. 2017; 52:1148–1151.
Article14. Oracz G, Pertkiewicz J, Dadalski M, et al. Complications of endoscopic retrograde cholangiopancreatography in children with chronic pancreatitis depends on center experience. J Pediatr. 2017; 186:215–216.
Article15. Wang D, Bi YW, Ji JT, et al. Extracorporeal shock wave lithotripsy is safe and effective for pediatric patients with chronic pancreatitis. Endoscopy. 2017; 49:447–455.
Article16. Cho JM, Jeong IS, Kim HJ, Oh SH, Kim KM. Early adverse events and long-term outcomes of endoscopic sphincterotomy in a pediatric population: a single-center experience. Endoscopy. 2017; 49:438–446.
Article17. Usatin D, Fernandes M, Allen IE, Perito ER, Ostroff J, Heyman MB. Complications of endoscopic retrograde cholangiopancreatography in pediatric patients; a systematic literature review and meta-analysis. J Pediatr. 2016; 179:160–165.e3.
Article18. Troendle DM, Abraham O, Huang R, Barth BA. Factors associated with post-ERCP pancreatitis and the effect of pancreatic duct stenting in a pediatric population. Gastrointest Endosc. 2015; 81:1408–1416.19. Roseau G, Palazzo L, Dumontier I, et al. Endoscopic ultrasonography in the evaluation of pediatric digestive diseases: preliminary results. Endoscopy. 1998; 30:477–481.
Article20. Varadarajulu S, Wilcox CM, Eloubeidi MA. Impact of EUS in the evaluation of pancreaticobiliary disorders in children. Gastrointest Endosc. 2005; 62:239–244.
Article21. Bjerring OS, Durup J, Qvist N, Mortensen MB. Impact of upper gastrointestinal endoscopic ultrasound in children. J Pediatr Gastroenterol Nutr. 2008; 47:110–113.
Article22. Cohen S, Kalinin M, Yaron A, Givony S, Reif S, Santo E. Endoscopic ultrasonography in pediatric patients with gastrointestinal disorders. J Pediatr Gastroenterol Nutr. 2008; 46:551–554.
Article23. Attila T, Adler DG, Hilden K, Faigel DO. EUS in pediatric patients. Gastrointest Endosc. 2009; 70:892–898.
Article24. Al-Rashdan A, LeBlanc J, Sherman S, McHenry L, DeWitt J, Al-Haddad M. Role of endoscopic ultrasound for evaluating gastrointestinal tract disorders in pediatrics: a tertiary care center experience. J Pediatr Gastroenterol Nutr. 2010; 51:718–722.
Article25. Scheers I, Ergun M, Aouattah T, et al. Diagnostic and therapeutic roles of endoscopic ultrasound in pediatric pancreaticobiliary disorders. J Pediatr Gastroenterol Nutr. 2015; 61:238–247.
Article26. Mahajan R, Simon EG, Chacko A, et al. Endoscopic ultrasonography in pediatric patients--experience from a tertiary care center in India. Indian J Gastroenterol. 2016; 35:14–19.27. Gordon K, Conway J, Evans J, Petty J, Fortunato JE, Mishra G. EUS and EUS-guided interventions alter clinical management in children with digestive diseases. J Pediatr Gastroenterol Nutr. 2016; 63:242–246.
Article28. Patel S, Marshak J, Daum F, Iqbal S. The emerging role of endoscopic ultrasound for pancreaticobiliary diseases in the pediatric population. World J Pediatr. 2017; 13:300–306.
Article29. Lakhole A, Liu QY. Role of endoscopic ultrasound in pediatric disease. Gastrointest Endosc Clin N Am. 2016; 26:137–153.
Article30. Johal AS, Khara HS, Maksimak MG, Diehl DL. Endoscopic ultrasound-guided liver biopsy in pediatric patients. Endosc Ultrasound. 2014; 3:191–194.
Article31. Nabi Z, Talukdar R, Reddy DN. Endoscopic management of pancreatic fluid collections in children. Gut Liver. 2017; 11:474–480.
Article32. Nabi Z, Lakhtakia S, Basha J, et al. Endoscopic drainage of pancreatic fluid collections: long-term outcomes in children. Dig Endosc. 2017; 29:790–797.
Article33. Lakhtakia S, Agarwal J, Gupta R, Ramchandani M, Kalapala R, Nageshwar Reddy D. EUS-guided transesophageal drainage of peripancreatic fluid collections in children. Gastrointest Endosc. 2015; 82:587–588.
Article34. Ramesh J, Bang JY, Trevino J, Varadarajulu S. Endoscopic ultrasound-guided drainage of pancreatic fluid collections in children. J Pediatr Gastroenterol Nutr. 2013; 56:30–35.
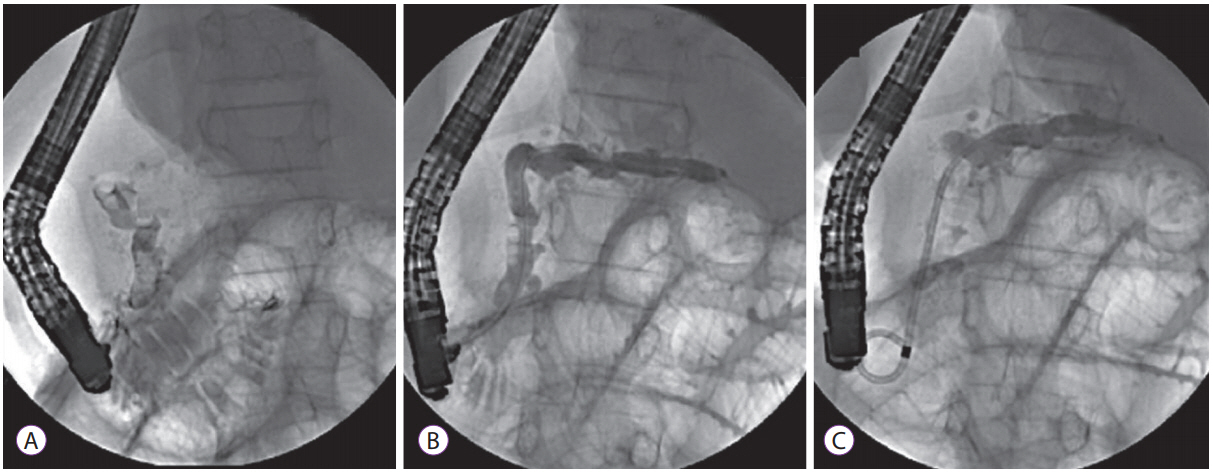
Article35. Jazrawi SF, Barth BA, Sreenarasimhaiah J. Efficacy of endoscopic ultrasound-guided drainage of pancreatic pseudocysts in a pediatric population. Dig Dis Sci. 2011; 56:902–908.
Article36. Nabi Z, Basha J, Reddy DN. Endoscopic management of pancreatic fluid collections-revisited. World J Gastroenterol. 2017; 23:2660–2672.
Article37. Siddiqui AA, Adler DG, Nieto J, et al. EUS-guided drainage of peripancreatic fluid collections and necrosis by using a novel lumen-apposing stent: a large retrospective, multicenter U.S. experience (with videos). Gastrointest Endosc. 2016; 83:699–707.
Article38. Rinninella E, Kunda R, Dollhopf M, et al. EUS-guided drainage of pancreatic fluid collections using a novel lumen-apposing metal stent on an electrocautery-enhanced delivery system: a large retrospective study (with video). Gastrointest Endosc. 2015; 82:1039–1046.
Article39. Sharaiha RZ, Tyberg A, Khashab MA, et al. Endoscopic therapy with lumen-apposing metal stents is safe and effective for patients with pancreatic walled-off necrosis. Clin Gastroenterol Hepatol. 2016; 14:1797–1803.40. Bang JY, Varadarajulu S. Endoscopic treatment of walled-off necrosis in children: clinical experience and treatment outcomes. J Pediatr Gastroenterol Nutr. 2016; 63:e31–e35.
Article41. Nabi Z, Lakhtakia S, Basha J, et al. Endoscopic ultrasound-guided drainage of walled-off necrosis in children with fully covered self-expanding metal stents. J Pediatr Gastroenterol Nutr. 2017; 64:592–597.
Article42. Trikudanathan G, Arain M, Mallery S, Freeman M, Attam R. Endoscopic necrosectomy in children. J Pediatr Gastroenterol Nutr. 2014; 59:270–273.
Article43. Kheder J, Han S, Wassef WY. Successful endoscopic pancreatic necrosectomy in 5-year-old child. Am J Gastroenterol. 2016; 111:443–444.
Article44. Nabi Z, Reddy DN. Achalasia cardia–recent advances in diagnosis and endoscopic management. J Gastrointest Dig Syst. 2016; 6:393.45. Nabi Z, Ramchandani M, Reddy DN, et al. Per oral endoscopic myotomy in children with achalasia cardia. J Neurogastroenterol Motil. 2016; 22:613–619.
Article46. Nabi Z, Ramchandani M, Chavan R, et al. Per-oral endoscopic myotomy for achalasia cardia: outcomes in over 400 consecutive patients. Endosc Int Open. 2017; 5:E331–E339.
Article47. Inoue H, Sato H, Ikeda H, et al. Per-oral endoscopic myotomy: a series of 500 patients. J Am Coll Surg. 2015; 221:256–264.
Article48. Tan Y, Zhu H, Li C, Chu Y, Huo J, Liu D. Comparison of peroral endoscopic myotomy and endoscopic balloon dilation for primary treatment of pediatric achalasia. J Pediatr Surg. 2016; 51:1613–1618.
Article49. Chen WF, Li QL, Zhou PH, et al. Long-term outcomes of peroral endoscopic myotomy for achalasia in pediatric patients: a prospective, single-center study. Gastrointest Endosc. 2015; 81:91–100.
Article50. Li C, Tan Y, Wang X, Liu D. Peroral endoscopic myotomy for treatment of achalasia in children and adolescents. J Pediatr Surg. 2015; 50:201–205.
Article51. Nabi Z, Ramchandani M, Chavan R, et al. Per-oral endoscopic myotomy in children- first experience with a new triangular knife. J Pediatr Gastroenterol Nutr. 2017; Jun. 2. [Epub]. https://doi.org/10.1097/mpg.0000000000001636.
Article52. Khashab MA, El Zein M, Kumbhari V, et al. Comprehensive analysis of efficacy and safety of peroral endoscopic myotomy performed by a gastroenterologist in the endoscopy unit: a single-center experience. Gastrointest Endosc. 2016; 83:117–125.
Article53. Nabi Z, Ramchandani M, Reddy DN. Peroral endoscopic myotomy in a child with achalasia cardia. J Pediatr Gastroenterol Nutr. 2017; 65:e44.
Article54. Caldaro T, Familiari P, Romeo EF, et al. Treatment of esophageal achalasia in children: today and tomorrow. J Pediatr Surg. 2015; 50:726–730.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Tuberculosis in Korea - yesterday, today, today and Tomorrow
- Medical Dispute Related to Gastrointestinal Endoscopy Complications: Prevention and Management
- Enteral nutrition in the biologic era: learn from yesterday, live for today, hope for tomorrow
- Upper gastrointestinal diseases diagnosed by upper gastrointestinal fiberoptic endoscopy in children
- Role of Endoscopy in Motility Disorders of Upper Gastrointestinal Tract