Perinatology.
2017 Dec;28(4):140-145. 10.14734/PN.2017.28.4.140.
Staphylococcus capitis Induced Late-onset Sepsis in Very Low Birth Weight Infants
- Affiliations
-
- 1Department of Pediatrics, Ulsan University Hospital, University of Ulsan College of Medicine, Ulsan, Korea. pentawish@hanmail.net
- 2Department of Laboratory Medicine, Ulsan University Hospital, University of Ulsan College of Medicine, Ulsan, Korea.
- KMID: 2409121
- DOI: http://doi.org/10.14734/PN.2017.28.4.140
Abstract
OBJECTIVE
To determine the causative organisms of late-onset sepsis (LOS) and describe LOS induced by Staphylococcus capitis (S. capitis) in very low birth weight infants (VLBWI).
METHODS
The medical records of VLBWI with blood culture proven LOS admitted to Ulsan University Hospital between January 2010 and December 2016 were investigated retrospectively.
RESULTS
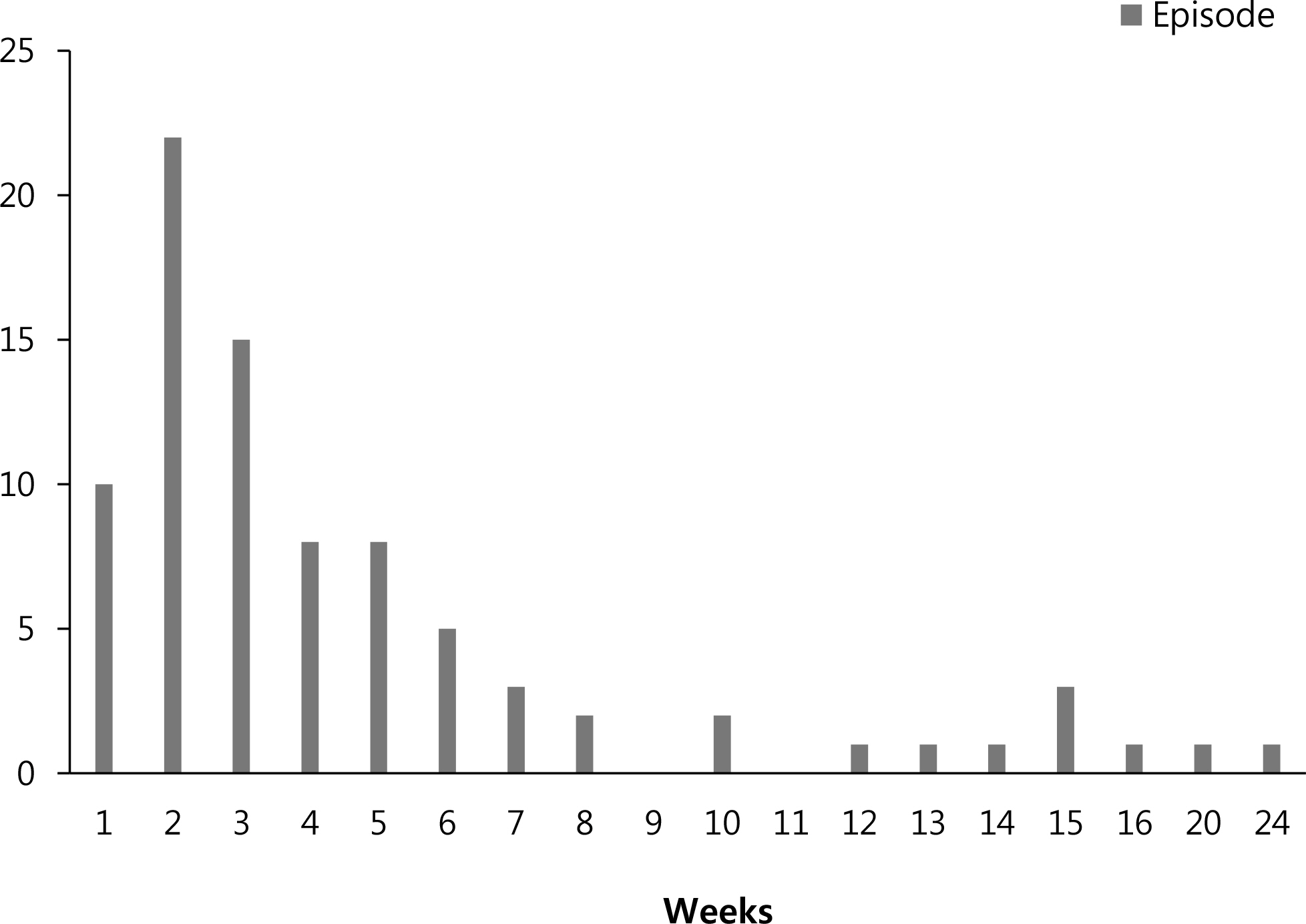
Among 329 VLBWI, 84 episodes of LOS occurred in 60 neonates (18.2%). Forty-two (50.0%) episodes were caused by coagulase-negative staphylococci (CoNS) and S. capitis and S. epidermidis were the leading organisms. S. capitis LOS developed in 21 VLBWI with 26 (30.9%) episodes. Necrotizing enterocolitis developed in 3 patients and 1 was diagnosed with infectious endocarditis. Six neonates died and death in 2 patients was directly related to S. capitis LOS. All episodes of S. capitis LOS demonstrated oxacillin and multi-drug resistance.
CONCLUSION
CoNS are the most common cause of LOS in VLBWI. In addition to S. epidermidis, S. capitis should be considered as an important emerging cause of LOS, as it is associated with severe morbidity and increased mortality in VLBWI.
MeSH Terms
Figure
Reference
-
1). Stoll BJ., Hansen N., Fanaroff AA., Wright LL., Carlo WA., Ehrenkranz RA, et al. Late-onset sepsis in very low birth weight neonates: the experience of the NICHD Neonatal Research Network. Pediatrics. 2002. 110(2 Pt 1):285–91.
Article2). Lee SM., Chang M., Kim KS. Blood culture proven early onset sepsis and late onset sepsis in very-low-birth-weight infants in Korea. J Korean Med Sci. 2015. 30(Suppl 1):S67–74.
Article3). Boghossian NS., Page GP., Bell EF., Stoll BJ., Murray JC., Cotton CM, et al. Late-onset sepsis in very low birth weight infants from singleton and multiple-gestation births. J Pediatr. 2013. 162:1120–4.
Article4). Klingenberg C., Rønnestad A., Anderson AS., Abrahamsen TG., Zorman J., Villaruz A, et al. Persistent strains of coagulase-negative staphylococci in a neonatal intensive care unit: virulence factors and invasiveness. Clin Microbiol Infect. 2007. 13:1100–11.
Article5). Ruhe J., Menon A., Mushatt D., Dejace P., Hasbun R. Non-epidermidis coagulase-negative staphylococcal bacteremia: clinical predictors of true bacteremia. Eur J Clin Microbiol Infect Dis. 2004. 23:495–8.6). Park HW., Lim G., Koo SE., Lee BS., Kim KS., Pi SY, et al. Causative agents and antimicrobial sensitivity of neonatal sepsis: ten-year experience in one neonatal intensive care unit. J Korean Soc Neonatol. 2009. 16:172–81.7). Wang SM., Liu CC., Tseng HW., Yang YJ., Lin CH., Huang AH, et al. Staphylococcus capitis bacteremia of very low birth weight premature infants at neonatal intensive care units: clinical significance and antimicrobial susceptibility. J Microbiol Immunol Infect. 1999. 32:26–32.8). Gras-Le Guen C., Fournier S., Andre-Richet B., Caillon J., Chamoux C., Espaze E, et al. Almond oil implicated in a Staphylococcus capitis outbreak in a neonatal intensive care unit. J Perinatol. 2007. 27:713–7.
Article9). Rasigade JP., Raulin O., Picaud JC., Tellini C., Bes M., Grando J, et al. Methicillin-resistant Staphylococcus capitis with reduced vancomycin susceptibility causes late-onset sepsis in intensive care neonates. PLoS One. 2012. 7:e31548.
Article10). Ben Said M., Hays S., Bonfils M., Jourdes E., Rasigade JP., Laurent F, et al. Late-onset sepsis due to Staphylococcus capitis tneonatalis' in low-birthweight infants: a new entity? J Hosp Infect. 2016. 94:95–8.11). Van Der Zwet WC., Debets-Ossenkopp YJ., Reinders E., Kapi M., Savelkoul PH., Van Elburg RM, et al. Nosocomial spread of a Staphylococcus capitis strain with heteroresistance to vancomycin in a neonatal intensive care unit. J Clin Microbiol. 2002. 40:2520–5.12). Butin M., Rasigade JP., Martins-Simões P., Meugnier H., Lemriss H., Goering RV, et al. Wide geographical dissemination of the multiresistant Staphylococcus capitis NRCS-A clone in neonatal intensive-care units. Clin Microbiol Infect. 2016. 22:46–52.
Article13). Hornik CP., Fort P., Clark RH., Watt K., Benjamin DK Jr., Smith PB, et al. Early and late onset sepsis in very-low-birth weight infants from a large group of neonatal intensive care units. Early Hum Dev. 2012. 88(Suppl 2):S69–74.14). Mularoni A., Madrid M., Azpeitia A., Valls i Soler A. The role of coagulase-negative staphylococci in early onset sepsis in a large European cohort of very low birth weight infants. Pediatr Infect Dis J. 2014. 33:e121–5.
Article15). Stoll BJ., Hansen N., Fanaroff AA., Wright LL., Carlo WA., Ehrenkranz RA, et al. Changes in pathogens causing early-onset sepsis in very-low-birth-weight infants. N Engl J Med. 2002. 347:240–7.
Article16). Van den Hoogen A., Gerards LJ., Verboon-Maciolek MA., Fleer A., Krediet TG. Long-term trends in the epidemiology of neonatal sepsis and antibiotic susceptibility of causative agents. Neonatology. 2010. 97:22–8.
Article17). Schmidt BK., Kirpalani HM., Corey M., Low DE., Philip AG., Ford-Jones EL. Coagulase-negative staphylococci as true pathogens in newborn infants: a cohort study. Pediatr Infect Dis J. 1987. 6:1026–31.18). Sohn AH., Garrett DO., Sinkowitz-Cochran RL., Grohskopf LA., Levine GL., Stover BH, et al. Prevalence of nosocomial infections in neonatal intensive care unit patients: results from the first national point-prevalence survey. J Pediatr. 2001. 139:821–7.
Article19). Gray JE., Richardson DK., McCormick MC., Goldmann DA. Coagulase-negative staphylococcal bacteremia among very low birth weight infants: relation to admission illness severity, resource use, and outcome. Pediatrics. 1995. 95:225–30.
Article20). Freeman J., Goldmann DA., Smith NE., Sidebottom DG., Epstein MF., Platt R. Association of intravenous lipid emulsion and coagulase-negative staphylococcal bacteremia in neonatal intensive care units. N Engl J Med. 1990. 323:301–8.
Article21). Johnson-Robbins LA., el-Mohandes AE., Simmens SJ., Keiser JF. Staphylococcus epidermidis sepsis in the intensive care nursery: a characterization of risk associations in infants < 1,000 g. Biol Neonate. 1996. 69:249–56.22). Goldmanln DA. Bacterial colonization and infection in the neonate. Am J Med. 1981. 70:417–22.23). Horan TC., Andrus M., Dudeck MA. CDC/NHSN surveillance definition of health care-associated infection and criteria for specific types of infections in the acute care setting. Am J Infect Control. 2008. 36:309–32.
Article24). Isaacs D. Australasian Study Group For Neonatal Infections. A ten year, multicentre study of coagulase negative staphylococcal infections in Australasian neonatal units. Arch Dis Child Fetal Neonatal Ed. 2003. 88:F89–93.
Article25). Ng PC., Chow VC., Lee CH., Ling JM., Wong HL., Chan RC. Persistent Staphylococcus capitis septicemia in a preterm infant. Pediatr Infect Dis J. 2006. 25:652–4.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Blood Culture Proven Early Onset Sepsis and Late Onset Sepsis in Very-Low-Birth-Weight Infants in Korea
- Changes in Pathogens and Antibiotic Sensitivities in very Low Birth Weight Infants with Neonatal Sepsis
- Early-Onset Sepsis Due to Listeria Monocytogenes in a Extremely Low Birth Weight Infant
- Extubation Time by Birth Weight and the Predictors for Success/Failure at the First Extubation in Extremely Low Birth Weight Infants
- Clinical Observation of Neonatal Sepsis according to Onset of Disease