J Korean Soc Spine Surg.
2018 Mar;25(1):30-34. 10.4184/jkss.2018.25.1.30.
Widespread Lumbosacral Subdural Abscess after Bee Venom Therapy: A Case Report
- Affiliations
-
- 1Department of Orthopedic Surgery, Bundang Jesaeng General Hospital, Seongnam, Korea. yslee2808@gmail.com
- KMID: 2408305
- DOI: http://doi.org/10.4184/jkss.2018.25.1.30
Abstract
- STUDY DESIGN: Case report.
OBJECTIVES
We report a case of widespread lumbosacral subdural abscess in a patient who underwent bee venom therapy. SUMMARY OF LITERATURE REVIEW: Subdural abscess is rare, but has a poor prognosis. Therefore, prompt recognition and appropriate treatment are paramount.
MATERIALS AND METHODS
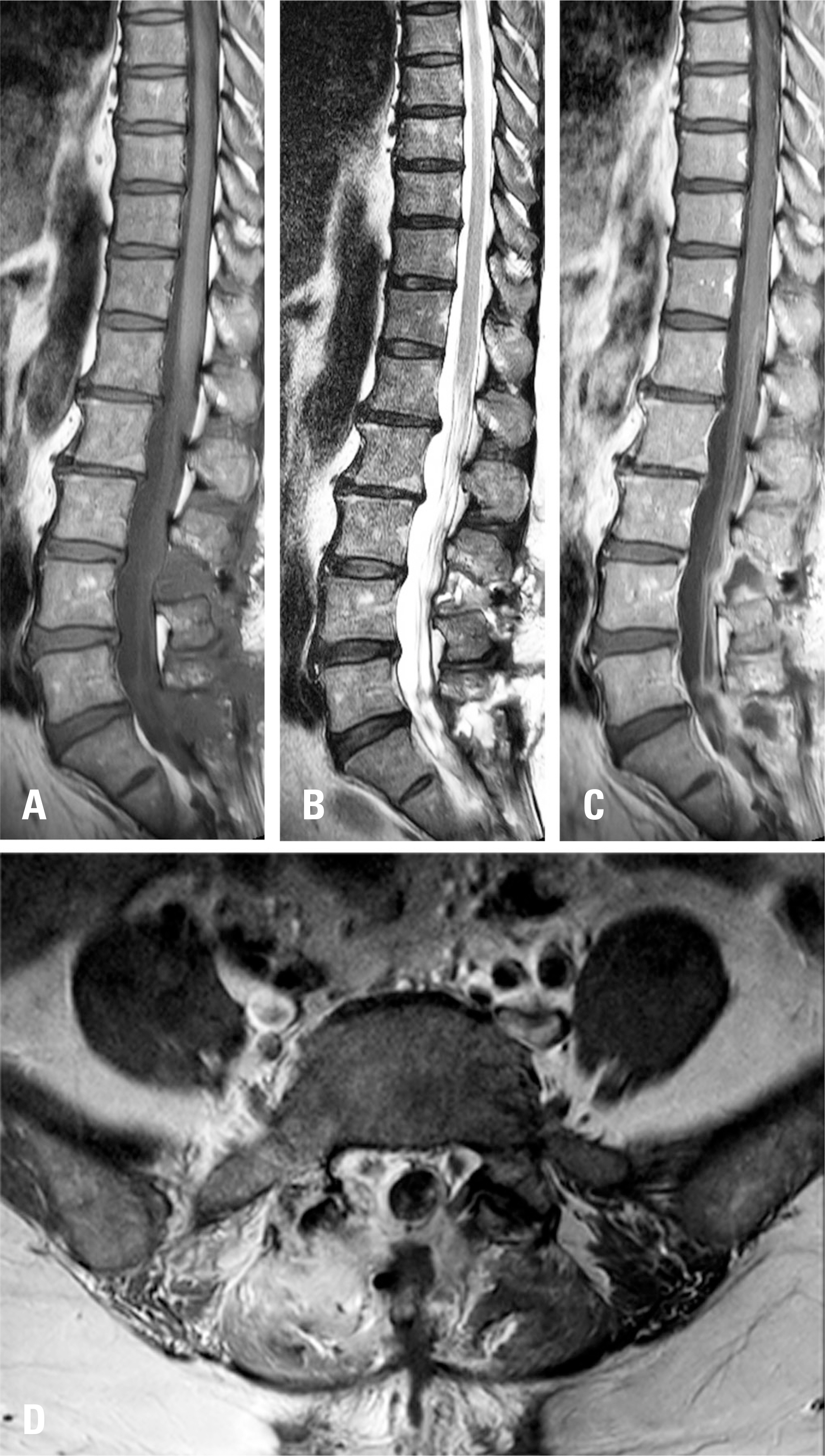
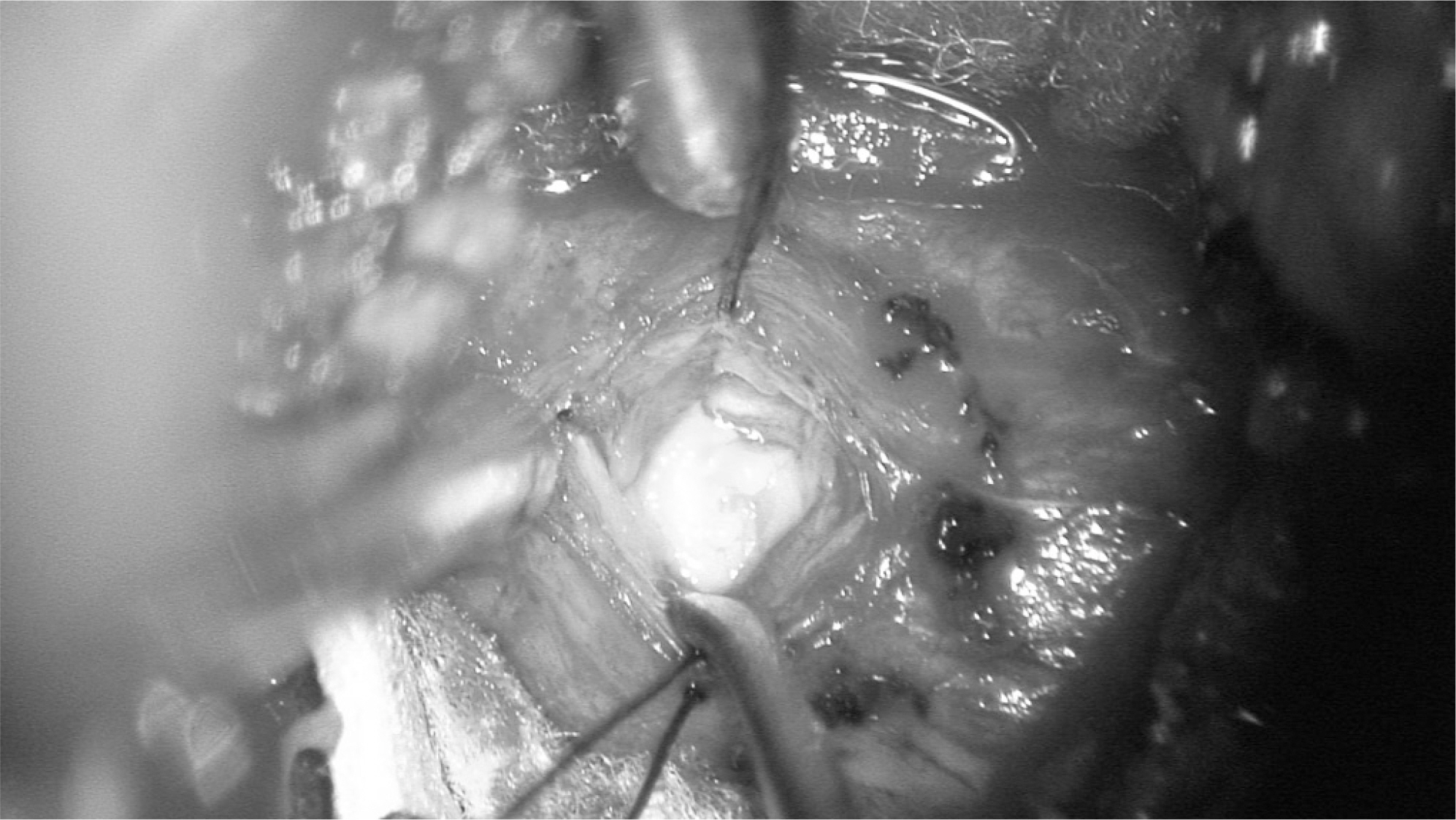
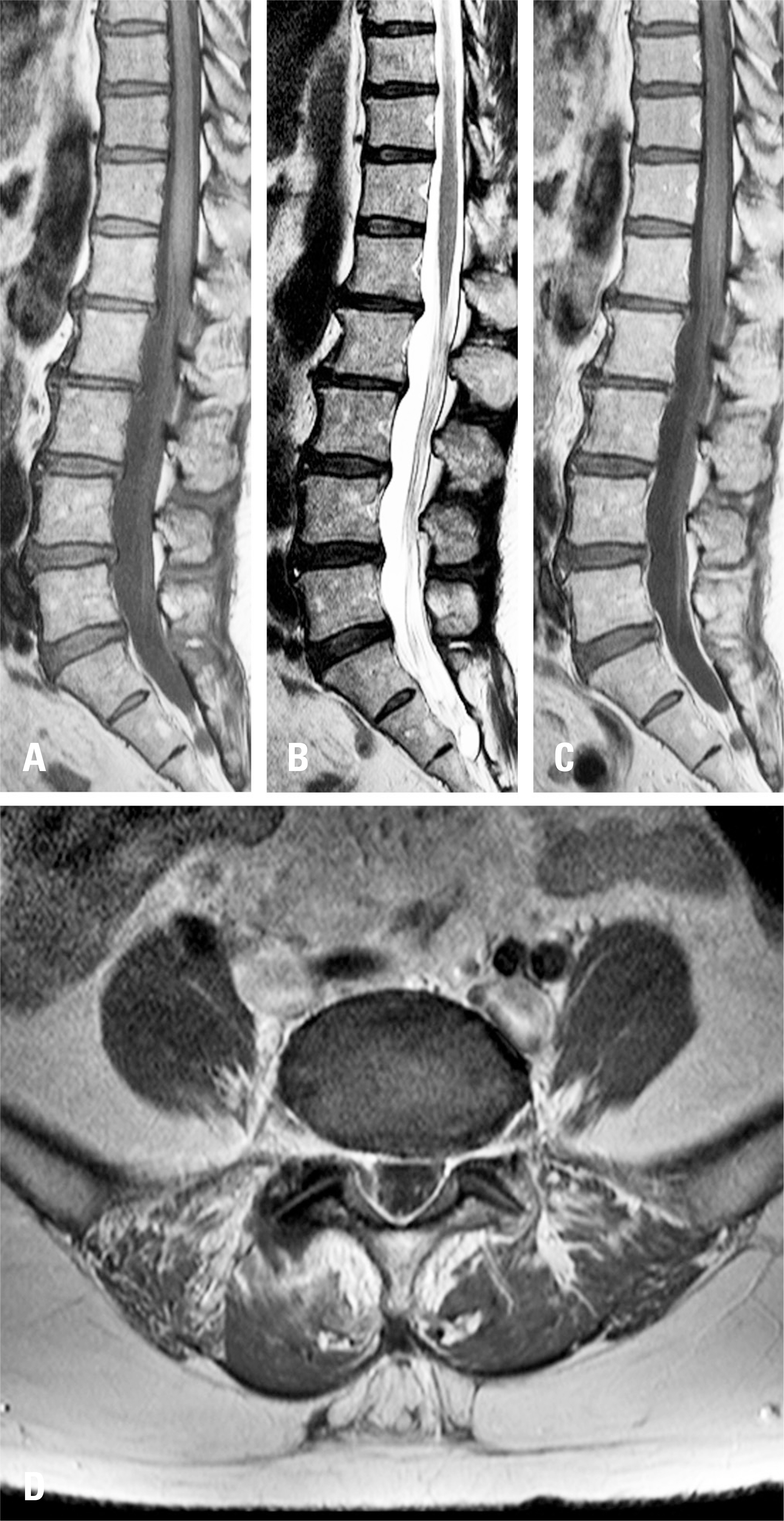
A 54-year-old woman was hospitalized due to severe back pain. Two days previously, she had undergone bee venom therapy. The patient then visited the emergency room because of severe back pain. However, a paraspinal infection was not detected on enhanced magnetic resonance imaging (MRI). Six days after admission, the patient showed signs of meningeal irritation and an emergency cerebrospinal fluid analysis showed typical findings of bacterial meningitis. Although adequate antibiotic treatment was administered, 20 days after admission, the patient's symptoms became aggravated. Pachymeningeal enhancement, myelomeningitis, and subdural abscess compressing the cauda equina were found on enhanced MRI. Thus, laminectomy between L3-L4 and L5-S1 was performed, as well as subdural abscess drainage. Antibiotic agents were applied for 6 weeks after the operation, and resolution of the subdural abscess was identified on follow-up MRI.
RESULTS
In this patient, lumbosacral subdural abscess occurred due to bee venom therapy. It was cured by adequate surgical and antibiotic treatment.
CONCLUSIONS
Bee venom therapy can cause subdural abscess of the spinal cord. Even if it is a rare case, this possibility is worth consideration in the Korean medical context.
Keyword
MeSH Terms
Figure
Reference
-
1. Darouiche RO. Spinal epidural abscess and subdural empyema. Handb Clin Neurol. 2000; 96:91–9. DOI: 10.1016/s0072-9752 (09)96007-9.
Article2. Bluman EM, Palumbo MA, Lucas PR. Spinal epidural abscess in adults. J Am Acad Orthop Surg. 2004 May-Jun; 12(3):155–63. DOI: 10.5435/00124635-200405000-00003.
Article3. Bartels RH, de Jong TR, Grotenhuis JA. Spinal subdural abscess: Case report. J Neurosurg. 1992 Feb; 76(2):307–11. DOI: 10.3171/jns.1992.76.2.0307.4. Levy ML, Weider BH, Schneider J, et al. Subdural empyema of the cervical spine: Clinicopathological correlates and magnetic resonance imaging: Report of three cases. J Neurosurg. 1993 Dec; 79(6):929–35. DOI: 10.3171/jns.1993.79.6.0929.5. Chen CY, Lin KL, Wang HS, et al. Dermoid cyst with dermal sinus tract complicated with spinal subdural abscess. Pediatr Neurol. 1999 Feb; 20(2):157–60. DOI: 10.1016/s0887-8994 (98)00126-x.
Article6. Lim HY, Choi HJ, Kim SJ, et al. Chronic spinal subdural abscess mimicking an intradural–extramedullary tumor. Eur Spine J. 2013 May; 22(3 Suppl):497–500. DOI: 10.1007/s00586-013-2700-1.
Article7. Vural M, Arslantaş A, Adapinar B, et al. Spinal subdural Staphylococcus aureus abscess: case report and review of the literature. Acta Neurol Scand. 2005 Nov; 112(5):343–6. DOI: 10.1111/j.1600-0404.2005.00496.x.
Article8. Bluman EM, Palumbo MA, Lucas PR. Spinal epidural abscess in adults. J Am Acad Orthop Surg. 2004 May-Jun; 12(3):155–63. DOI: 10.5435/00124635-200405000-00003.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Bee Venom Therapy for Musculoskeletal Disorders
- A Case of Newly Developed Pemphigus Foliaceus and Possible Association with Alternative Bee-Venom Therapy
- Infectious Spondylodiscitis Accompanied by Widespread Thoracolumbar Subdural Abscess
- A Case of Ischemic Stroke Following Bee Venom Acupuncture
- Serum sickness reaction with skin involvement induced by bee venom injection therapy