J Korean Soc Spine Surg.
2018 Mar;25(1):1-8. 10.4184/jkss.2018.25.1.1.
Neurological Complications of Posterior Spinal Surgery: Incidence and Clinical Features
- Affiliations
-
- 1Seoul Sacred Heart General Hospital, Orthopedic Department, Korea. dr.wonshik@hanmail.net
- KMID: 2408301
- DOI: http://doi.org/10.4184/jkss.2018.25.1.1
Abstract
- STUDY DESIGN: Retrospective study.
OBJECTIVES
To identify clinical features and risk factors helpful for the prevention and early diagnosis of neurological complications. OVERVIEW OF LITERATURE: Previous studies have investigated postoperative complications only for specific disease entities and did not present distinctive clinical features.
MATERIALS AND METHODS
This was an observational study of patients who underwent posterior thoracolumbar spinal surgery in the orthopedic department of a single hospital over the course of 19 years (1995-2013). The incidence, cause, onset time, and risk factors of complications were investigated. Neurological deterioration was graded on a 5-point numeric scale: G1, increased leg pain or sensory loss, G2, unilateral motor weakness; G3, bilateral motor weakness; G4, cauda equina syndrome; and G5, complete paraplegia.
RESULTS
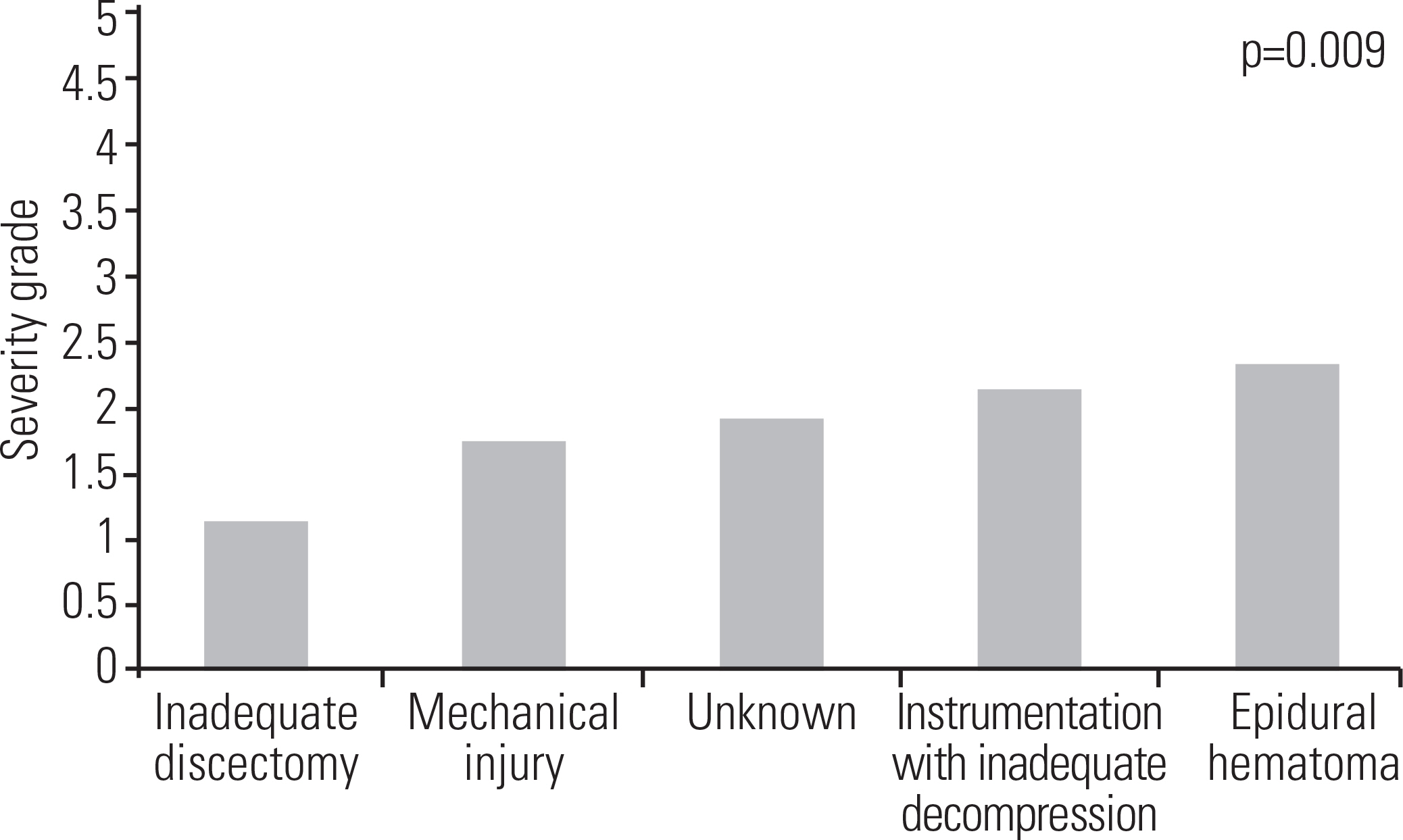
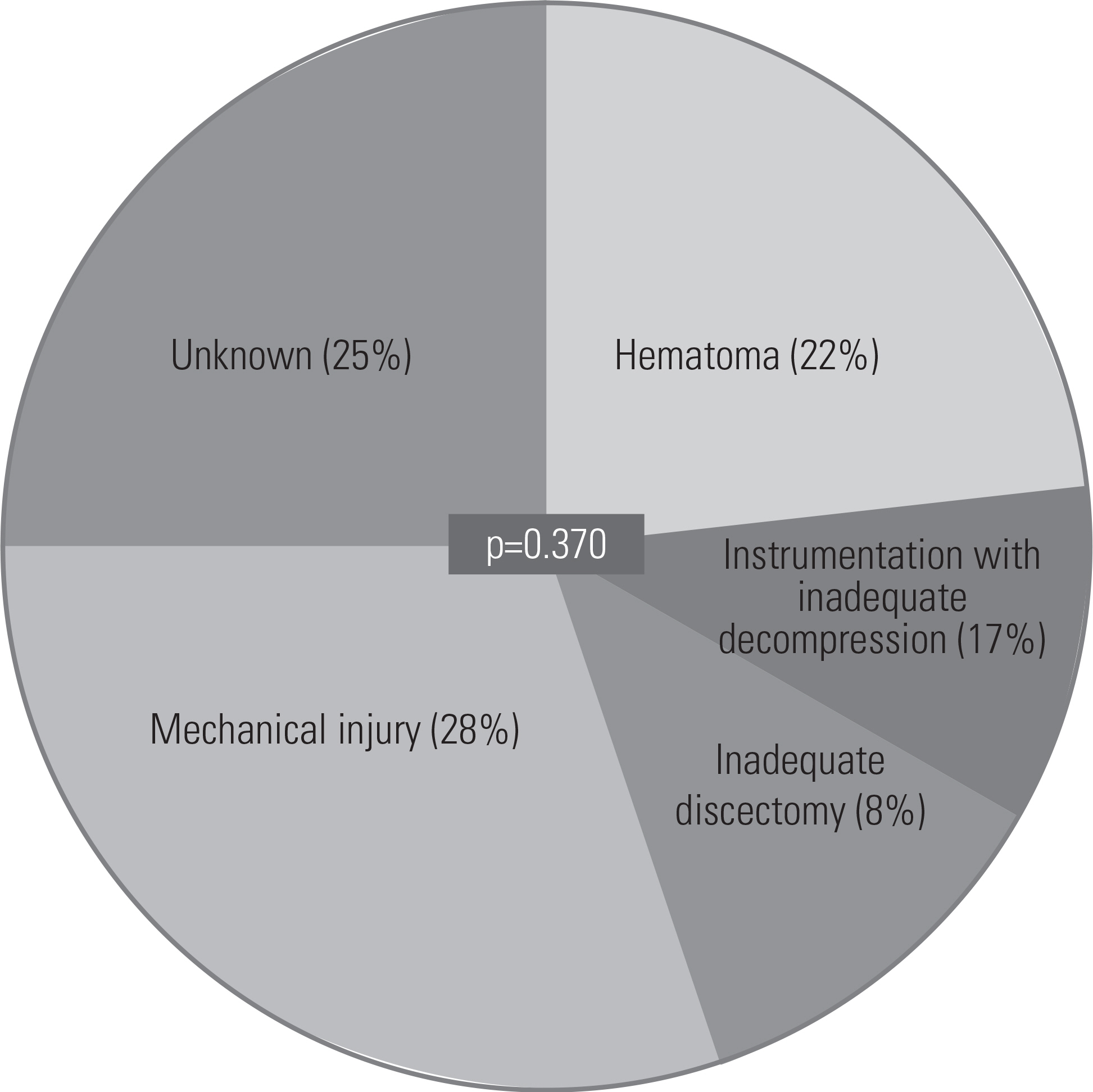
Sixty-five cases out of 6574 (0.989%) developed neurological complications due to the following causes: epidural hematoma, 0.380%; instrumentation with inadequate decompression, 0.213%; mechanical injury, 0.167%; inadequate discectomy, 0.061%; and unknown cause, 0.167% (p=0.000). The grade of neurological deterioration was G1 in 0.167% of patients, G2 in 0.517%, G3 in 0.228%, G4 in 0.046%, and G5 in 0.030%. Neurological deterioration was most severe in patients who experienced epidural hematoma, followed by those in whom complications occurred due to instrumentation with inadequate decompression, unknown causes, mechanical injury, and inadequate discectomy, in order (p=0.009). Revision surgery was a significant risk factor (p=0.000; odds ratio, 2.741). The time that elapsed until symptom development was as follows, in order: unknown cause, 0.6 hours; epidural hematoma, 5.4 hours; mechanical injury, 6.6 hours; inadequate discectomy, 18.0 hours; and instrumentation with insufficient decompression, 36.0 hours (p=0.001).
CONCLUSIONS
The incidence of neurological complications in our cohort was 1%. Revision surgery increased the risk by 3 times. Severe cases (cauda equina syndrome or complete paraplegia) rarely developed, occurring in 0.08% of patients. The major causes of neurological decline were epidural hematoma and instrumentation with inadequate decompression. Close observation in the early period was important for the diagnosis because most patients developed symptoms within 12 hours. Delayed diagnosis was most common in complications caused by instrumentation with inadequate decompression.
MeSH Terms
Figure
Reference
-
1. Deyo RA, Cherkin DC, Loeser JD, et al. Morbidity and mortality in association with operations on the lumbar spine. The influence of age, diagnosis, and procedure. J Bone Joint Surg Am. 1992 Apr; 74(4):536–43. DOI: 10.2106/00004623-199274040-00009.
Article2. Lapp MA, Bridwell KH, Lenke LG, et al. Long-term complications in adult spinal deformity patients having combined surgery a comparison of primary to revision patients. Spine (Phila Pa 1976). 2001 Apr 15; 26(8):973–83. DOI: 10.1097/00007632-200104150-00025.3. Bridwell KH, Lenke LG, Baldus C, et al. Major intraoperative neurologic deficits in pediatric and adult spinal deformity patients. Incidence and etiology at one institution. Spine (Phila Pa 1976). 1998 Feb 1; 23(3):324–31. DOI: 10.1097/00007632-199802010-00008.4. Cervellati S, Bettini N, Bianco T, et al. Neurological complications in segmental spinal instrumentation: analysis of 750 patients. Eur Spine J. 1996 Jun; 5(3):161–6. DOI: 10.1007/bf00395507.
Article5. Henriques T, Olerud C, Petren-Mallmin M, et al. Cauda equina syndrome as a postoperative complication in five patients operated for lumbar disc herniation. Spine (Phila Pa 1976). 2001 Feb 1; 26(3):293–7. DOI: 10.1097/00007632200102010-00015.
Article6. MacEwen GD, Bunnell WP, Sriram K. Acute neurological complications in the treatment of scoliosis. A report of the Scoliosis Research Society. J Bone Joint Surg Am. 1975 Apr; 57(3):404–8. DOI: 10.2106/00004623-197557030-00020.
Article7. Qiu Y, Wang S, Wang B, et al. Incidence and risk factors of neurological deficits of surgical correction for scoliosis: analysis of 1373 cases at one Chinese institution. Spine (Phila Pa 1976). 2008 Mar; 33(5):519–26. DOI: 10.1097/brs.0b013e3181657d93.8. Duncan JW, Bailey RA. Cauda equina syndrome following decompression for spinal stenosis. Global Spine J. 2011 Dec; 1(1):15–8. DOI: 10.1055/s-0031-1296051.
Article9. McLaren AC, Bailey SI. Cauda equina syndrome: a complication of lumbar discectomy. Clin Orthop Relat Res. 1986 Mar; 204:143–9. DOI: 10.1097/00003086-198603000-00015.10. Cramer DE, Maher PC, Pettigrew DB, et al. Major neurologic deficit immediately after adult spinal surgery: incidence and etiology over 10 years at a single training institution. J Spinal Disord Tech. 2009 Dec; 22(8):565–70. DOI: 10.1097/bsd.0b013e318193452a.11. Gerlach R, Raabe A, Beck J, et al. Postoperative nadroparin administration for prophylaxis of thromboembolic events is not associated with an increased risk of hemorrhage after spinal surgery. Eur Spine J. 2004 Feb; 13(1):9–13. DOI: 10.1007/s00586-003-0642-8.12. Platzer P, Thalhammer G, Jaindl M, et al. Thromboembolic complications after spinal surgery in trauma patients. ActaOrthop. 2006 Oct; 77(5):755–60. DOI: 10.1080/17453670610012944.
Article13. Uribe J, Moza K, Jimenez O, et al. Delayed postoperative spinal epidural hematomas. Spine J. 2003 Mar-Apr; 3(2):125–9. DOI: 10.1016/s1529-9430 (02)00535-1.
Article14. Awad JN, Kebaish KM, Donigan J, et al. Analysis of the risk factors for the development of post-operative spinal epidural haematoma. J Bone Joint Surg Br. 2005 Sep; 87(9):1248–52. DOI: 10.1302/0301-620x.87b9.16518.
Article15. Dickman CA, Fessler RG, MacMillan M, et al. Transpedicular screw-rod fixation of the lumbar spine: operative technique and outcome in 104 cases. J Neurosurg. 1992 Dec; 77(6):860–70. DOI: 10.3171/jns.1992.77.6.0860.
Article16. Lawton MT, Porter RW, Heiserman JE, et al. Surgical management of spinal epidural hematoma: relationship between surgical timing and neurological outcome. J Neurosurg. 1995 Jul; 83(1):1–7. DOI: 10.3171/jns.1995.83.1.0001.
Article17. Scaduto AA, Gamradt SC, Yu WD, et al. Perioperative complications of threaded cylindrical lumbar interbody fusion devices: anterior versus posterior approach. J Spinal Disord Tech. 2003 Dec; 16(6):502–7. DOI: 10.1097/00024720-200312000-00003.18. Scavarda D, Peruzzi P, Bazin A, et al. [Postoperative spinal extradural hematomas. 14 cases]. Neurochirurgie. 1997; 43(4):220–7.19. Sokolowski MJ, Garvey TA, Perl J, et al. Postoperative lumbar epidural hematoma: does size really matter? Spine (Phila Pa 1976). 2008 Jan 1; 33(1):114–9. DOI: 10.1097/brs.0b013e31815e3a26.20. Brown MD, Brookfield KF. A randomized study of closed wound suction drainage for extensive lumbar spine surgery. Spine (Phila Pa 1976). 2004 May 15; 29(10):1066–8. DOI: 10.1097/00007632-200405150-00003.
Article21. Chimenti P, Molinari R. Post-operative spinal epidural hematoma causing American Spinal Injury Association B spinal cord injury in patients with suction wound drains. J Spinal Cord Med. 2013 May; 36(3):213–9. DOI: 10.1179/2045772312y.0000000070.
Article22. Kanayama M, Oha F, Togawa D, et al. Is closed-suction drainage necessary for single-level lumbar decompression?: Review of 560 cases. Clin Orthop Relat Res. 2010 Oct; 468(10):2690–4. DOI: 10.1007/s11999-010-1235-6.
Article23. Parker MJ, Livingstone V, Clifton R, et al. Closed suction surgical wound drainage after orthopaedic surgery. Cochrane Database Syst Rev. 2007 Jul 18; 3:CD001825. DOI: 10.1002/14651858.CD001825.pub2.
Article24. Walid MS, Abbara M, Tolaymat A, et al. The role of drains in lumbar spine fusion. World Neurosurg. 2012 Mar-Apr; 77(3-4):564–8. DOI: 10.1016/j.wneu.2011.05.058.
Article25. Yi S, Yoon DH, Kim KN, et al. Postoperative spinal epidural hematoma: risk factor and clinical outcome. Yonsei Med J. 2006 Jun 30; 47(3):326–32. DOI: 10.3349/ymj.2006.47.3.326.
Article26. Mirzai H, Eminoglu M, Orguc S. Are drains useful for lumbar disc surgery? A prospective, randomized clinical study. J Spinal Disord Tech. 2006 May; 19(3):171–7. DOI: 10.1097/01.bsd.0000190560.20872.a7.27. Alander DH, Stauffer ES. Gelfoam-induced acute quadriparesis after cervical decompression and fusion. Spine (Phila Pa 1976). 1995 Apr 15; 20(8):970–1. DOI: 10.1097/00007632-199504150-00016.
Article28. Buchowski JM, Bridwell KH, Lenke LG, et al. Epidural spinal cord compression with neurologic deficit associated with intrapedicular application of hemostatic gelatin matrix during pedicle screw insertion. Spine (Phila Pa 1976). 2009 Jun; 34(13):E473–7. DOI: 10.1097/BRS.0b013e3181a56a21.
Article29. Epstein NE, Silvergleid RS, Hollingsworth R. Increased postoperative cervical myelopathy and cord compression resulting from the use of Gelfoam. Spine J. 2009 Feb; 9(2):E19–21. DOI: 10.1016/j.spinee.2008.03.009.
Article30. Friedman J, Whitecloud TS 3rd. Lumbar cauda equina syndrome associated with the use of gelfoam: case report. Spine (Phila Pa 1976). 2001 Oct; 26(20):E485–7. DOI: 10.1097/00007632-200110150-00029.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Ossification of the Posterior Longitudinal Ligament in Cervical Spine: Prevalence, Management, and Prognosis
- Epidural Hematoma Presenting with Severe Neck Pain without Neurological Deficit - A Late Complication of Posterior Cervical Spine Surgery: Presentation of Three Unusual Cases
- The Result of Early Decompression of Progressive Neurologic Deficit after Spine Surgery: A Case Report
- Selective Angiography to Detect Anterior Spinal Artery Stenosis in Thoracic Ossification of the Posterior Longitudinal Ligament
- Analysis of the Prevalence and Distribution of Cervical and Thoracic Compressive Lesions of the Spinal Cord in Lumbar Degenerative Disease